Abstract
Near-infrared spectroscopy is a noninvasive method for monitoring brain oxygenation. The aim of the study was to investigate differences between cerebral oxygenation in different brain regions in newborns. In a prospective study, we monitored simultaneously left and right frontoparietal and temporo-occipital regional cerebral oxygen saturation (rScO2) and cerebral fractional tissue extraction (cFTOE: (arterial oxygen saturation (SaO2) − rScO2)/SaO2) using near-infrared spectroscopy. A 2-h measurement was performed on d 1, 3, and 7. We included 10 very preterm (GA <32 wk), 10 preterm (GA: 32–37 wk), and 10 term (GA ≥37 wk) neonates. Limits of agreement for difference of the measurements between different places were determined using the Bland-Altman method. In all subgroups, the rScO2 and cFTOE values at different regions were not different. Limits of agreement were between ±14 and ±18% for all subgroups. Left-to-right differences were small between different postnatal and GAs. A decrease and increase over time for rScO2 and cFTOE values was detected for all four brain regions, most pronounced for infants with GA <32 wk. Cerebral oxygenation in stable preterm and term neonates seems not to differ between different regions of the brain during the early neonatal period. However, variability of individual measurements was quite high as indicated by large limits of agreement.
Similar content being viewed by others
Main
Near-infrared spectroscopy (NIRS) is an increasingly accepted noninvasive method for monitoring regional cerebral oxygen saturation (rScO2) and cerebral fractional tissue oxygen extraction (cFTOE) in preterm and term neonates (1–3).
NIRS-determined cerebral oxygenation is usually unilaterally measured on the frontal or frontoparietal part of the neonatal skull (4,5). Although mostly used unilaterally, it has been shown that regional changes in cerebral blood flow and oxygenation may occur because of regional neuronal activation (6–8). Moreover, Chiron et al. (9) reported a right brain hemisphere dominance in infants, which may imply a different oxygenation/extraction pattern. Recently, we compared left-to-right frontoparietal NIRS-determined rScO2 in stable preterm and term neonates in the first week of life and found comparable rScO2values at both sensor positions, although there was a tendency of the rScO2 on d 3 to be higher at the right side. Furthermore, left-to-right differences occasionally occurred, in particular, during unstable arterial oxygen saturation (SaO2) patterns suggesting an uneven oxygenation of the brain, at least during and shortly after systemic desaturation (10). Finally, in the scarce bilateral NIRS-determined regional saturation studies done in neonates and infants, only oxygenation of the frontal (11) or frontoparietal (12) regions of the brain were investigated. However, no information is available yet with respect to the temporo-occipital brain regions, which have a higher rate of metabolism than the frontal region of the brain suggesting a more critical equilibrant in the delivery and consumption of oxygen (9).
Recently, there have become smaller NIRS sensors available, which enables us to monitor various regions of the neonatal brain at the same time, even in the smallest baby. Therefore, we performed a prospective observational study in which we monitored cerebral oxygenation and cerebral extraction bilaterally using NIRS in the frontoparietal and temporo-occipital regions of the brain of neonates with different GAs during the first week of life. We intended to investigate if there are significant differences in rScO2 and cFTOE between the left and right frontoparietal and temporo-occipital regions of the brain during a stable clinical condition. We hypothesized, also on basis of our earlier study (10), that during stable conditions, no differences of importance could be detected between the four regions simultaneously under investigation in the preterm infants but that lateralization may be a possibility in the term infant.
METHODS
Patient population.
Thirty infants admitted to the Neonatal Intensive Care and Medium Care Unit of the Wilhelmina Children's Hospital were included into this study. In total, we included 20 preterm and 10 term neonates in which we monitored NIRS-determined rScO2. Ten patients had a GA of <32 wk (very preterms), 10 patients had a GA between 32 and 36 completed weeks (preterms), and 10 patients were born with a GA of 37 wk or more. We included those infants to be expected to attend our hospital for at least 7 d for preterm infants and 3 d for term infants. Infants with periventricular/intraventricular hemorrhages grade 2 or higher according to the grading of Papile et al. (13) were excluded as were infants with chromosomal and/or syndromic abnormalities. Infants with unstable blood pressure or who developed a hemodynamically important ductus arteriosus during the recordings of NIRS-monitored rScO2 were also excluded because of its important impact on rScO2 (14). Finally, also infants with hyperbilirubinemia treated with phototherapy were excluded. Informed parental consent was obtained in all instances. The study was approved by the Medical Ethical Committee of the University Medical Centre, Utrecht.
Clinical data.
Obstetrical and intrapartum data were collected from the hospital records. Neonatal data were collected prospectively. Treatment decisions were made by the attending neonatologist. The SaO2 was monitored continuously by pulse oximetry.
Monitoring of cerebral tissue oxygenation and oxygen extraction.
NIRS-determined rScO2 was used as an estimator for changes in regional cerebral oxygenation. Because absolute values are provided, rScO2 is less dependent on the movement artifacts, and comparisons over time are possible (1).
Measurements were obtained using a near infrared spectrometer (INVOS 5100c; Somanetics Corp., Troy, MI). Four transducers (OxyAlert NIRSensor for Neonates), each containing a light-emitting diode and two distant detectors located 3 and 4 cm from the light-emitting diode, were attached symmetrically to the frontoparietal and temporo-occipital left and right side of the skull. The two different detectors allow us to remove the extracranial contribution of absorbed and scattered light by the application of a substraction algorithm. The rScO2 was calculated from the differential signals obtained from these two sensors, expressed as the venous-weighted percentage of oxygenated Hb (oxygenated Hb/total Hb); (total Hb = oxygenated Hb (O2Hb) + deoxygenated Hb (HHb). To investigate the balance between oxygen delivery and oxygen consumption, the relative cFTOE can be formulated as a ratio: (SaO2 − rScO2)/SaO2 (1,2).
An increase of cFTOE might indicate a reduced oxygen delivery to the brain with a constant oxygen consumption of the brain or higher oxygen consumption than oxygen delivery. A decrease of cFTOE suggests a decrease of oxygen extraction of the brain because of less use of oxygen or a constant oxygen consumption of the brain with an increased oxygen delivery to the brain (2).
Study design.
In this prospective observational study, we monitored infants with a GA in the three different groups as mentioned above. The recordings of NIRS-monitored rScO2 were collected with four neonatal transducers positioned on the left and right frontoparietal and temporo-occipital part of the skull. The neonatal transducers were coupled to the NIRS device, which was set to sample once every 5 s.
The transducers were numbered 1 to 4. We positioned transducer 1 left frontoparietally, transducer 2 right frontoparietally, number 3 right temporo-occipitally, and number 4 left temporo-occipitally, as shown in Figure 1. We coupled transducer 1 and 2 to the first preamplifier and transducer 3 and 4 to the second preamplifier. In our clinical setting, we experienced earlier that positioning transducer 1 and 3 at the front and transducer 2 and 4 at the back side of the head can cause interference. The position of the transducers mentioned above prevented this problem. Positioned like this, the distance between 1 and 3 and between 2 and 4 would be as far as possible and therefore the signals of the transducer were optimally received. The transducers were positioned and secured in place with an elastic opaque bandage to shield the optodes from any ambient light that may potentially interfere with light absorption recordings.
(A) Schematic overview of the placement of the sensors on the infant's skull, showing the four transducers with the position of the emitter (red dot) in two distant detectors (black dots). Sensors are numbered 1–4, with number 1 placed frontoparietal on the left side (left front), number 2 frontoparietal on the right side (right front), number 3 placed temporo-occipital on the right side (right back), and number 4 temporo-occipital on the left side (left back). Transducers were coupled to two preamplifiers (B). Sensor 1 and 2 were coupled to one preamplifier and sensor 3 and 4 to the second.
We aimed to obtain about 120 min of recordings, from which we could collect a minimum of 30 min of a stable clinical episode, without feeding, care, or painful procedures, to use for our analyses. After an accommodation period, data collection started and downloaded to a storage disk every 10 s. Although the data were collected during a stable period, we did not differentiate between sleep and awakeness state. The recordings were performed on d 1 (postnatal age 0–24 h: T1) and again on d 3 (postnatal age 48–72 h: T2), and for the preterm infants also a recording was made on d 7 (postnatal age 144–168 h: T3). Simultaneously, we monitored SaO2 with pulse oximetry (Nellcor pulse oximeter) with a sample rate of once per 10 s.
The simultaneously collected data and monitored parameters like blood pressure and heart rate were retrieved from the patient data management system (Metavision iMDsoft Boston, MA, sample frequency of 1 per minute). Arterial blood gasses were measured every 4 h in the preterm infants during the first day of life less frequent if the clinical situation was stable.
Cranial ultrasound studies were performed shortly after birth in all preterms and repeated every 24 h during the first 3 d in the very preterms and at the end of the first week. For the term infants, blood gasses and cranial ultrasound were only performed when indicated by the attending neonatologist.
Statistical analysis.
Data were summarized as mean values ±SD or as median values and ranges where appropriate. Comparisons of the four recordings of rScO2 and of cFTOE were done based on ANOVA test for repeated measurements, Pearson correlation coefficient, and Bland-Altman analyses. Adjustments for multiple comparisons were made by a Bonferroni test.
A selection of the NIRS data were made, to get a comparative set of data of one value for every 10 s, like collected with the pulse oximeter. Recordings of the NIRS-measured rScO2 were supposed to be saved on the NIRS-device every 5 s. By retrieving the data to process them on a personal computer, it seemed that the sample frequency varied from 6 to 8 s. We, therefore, selected six NIRS values every minute, choosing the ones most closely to 0, 10, 20, 30, 40, and 50 s, respectively. After this adaptation, comparisons were done from rScO2 or cFTOE values of a reliable recording providing us with rScO2 and cFTOE values for each transducer per patient every 10 s. A p < 0.05 was considered statistically significant. For the statistical analysis, SPSS 15.0 (SPSS Inc., Chicago, IL) was used.
RESULTS
Clinical characteristics.
Because we lost data of three infants, one of the very preterm subgroup and two of the term subgroup because of technical problems (unreliable tracings of rScO2), we eventually included 27 patients, 14 male and 13 female: 9, 10, and 8 infants in each subgroup (GA <32; 32–37; and ≥37 wk, respectively). The most important clinical data of the included infants are shown in Table 1. Most patients (70%) had no respiratory support, 4 (15%) had continuous positive airway pressure (CPAP), and 4 (15%) were on synchronized intermittent mandatory ventilation (SIMV) with mild ventilation conditions at the moment of recording. Any full-term infant needed respiratory support, (arterial) blood gasses, and Hb values was always stable and within normal limits (pCO2 between 40 and 50 mm Hg; Hb between 8 and 12 mM; not shown). Only one very preterm infant had a grade 1 periventricular hemorrhage.
Table 2 shows the median postnatal age with ranges at the time of recording for the different subgroups at T1 (postnatal age 0–24 h, d 1), T2 (postnatal age 48–72 h, d 3), and T3 (postnatal age 144–168 h, d 7). For all patients, the median postnatal age was 21, 63, and 151 h for T1, T2, and T3, respectively.
Patterns of rScO2 and cFTOE.
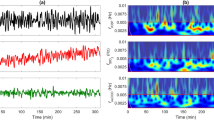
The total recording time was 3930 min (average of 64 min per measurement). For the statistical analysis, we only used the episodes of stable arterial saturation. Figure 2A and B provides the box-whisker plots (median and ranges) of rScO2 and cFTOE of the respective brain regions during the three subsequent postnatal ages of the three subgroups. No significant differences of rScO2 or cFTOE between the four regions under investigation could be detected at any postnatal age. However, we found sometimes a substantial variability between the rScO2 patterns and the cFTOE of the four regions under investigation as illustrated by a representative tracing (Fig. 3A and B). However, these differences seemed to be completely ad random, and there were no consistent or significant differences between the four brain regions: As also shown in Figure 2A and B, there was a significant decrease and increase, respectively, for rScO2 and cFTOE over the first week of life in all GA subgroups.
Mean rScO2 (A) and cFTOE (B) of all brain regions on postnatal age d 1 ( ) and postnatal age d 3 (
) and postnatal age d 3 ( ) for GA <32 wk, GA between 32 and 37 wk, and GA >37 wk, and postnatal age d 7 (
) for GA <32 wk, GA between 32 and 37 wk, and GA >37 wk, and postnatal age d 7 ( ) for GA <32 wk and GA between 32 and 37 wk, demonstrating the decrease and increase, respectively, for values of rScO2 and cFTOE as a function of postnatal age.
) for GA <32 wk and GA between 32 and 37 wk, demonstrating the decrease and increase, respectively, for values of rScO2 and cFTOE as a function of postnatal age.
Simple linear regression analysis revealed significant correlations between rScO2 for the left and right frontoparietal positions (r = 0.51, p < 0.01), the left and right temporo-occipital positions (r = 0.57, p < 0.01), the left frontoparietal and temporo-occipital positions (r = 0.49, p < 0.01), and the right frontoparietal and temporo-occipital positions (r = 0.55, p < 0.01). Also significant correlations were found between cFTOE for the left and right frontoparietal positions (r = 0.48, p < 0.01), the left and right temporo-occipital positions (r = 0.59, p < 0.01), the left frontoparietal and temporo-occipital positions (r = 0.50, p < 0.01), and the right frontoparietal and temporo-occipital positions (r = 0.56, p < 0.01).
The limits of agreement using the Bland-Altman method between the differences of rScO2 measured at the four brain regions during the first week of life were similar for the three subgroups and between ±15 and ±17% for the infants with a GA <32 wk; ±16 and ±18% for the infants with a GA between 32 and 37 wk; and between ±12 and ±16% for infants with a GA >37 wk. Figure 4 shows the limits of agreement of rScO2 of all three GA subgroups together for the four brain regions. The limits of agreement using the Bland-Altman method between the differences of cFTOE had a similar pattern compared with the rScO2 and was between ±0.13 and ±0.19 for the infants with a GA <32 wk; between ±0.18 and ±0.20 for the infants with a GA between 32 and 37 wk; and between ±0.10 and ±0.14 for infants with a GA >37 wk. Figure 5 shows the limits of agreement of cFTOE of all three GA subgroups together for the four brain regions.
Limits of agreement according to Bland and Altman (dotted lines) including all infants between NIRS-monitored rScO2 between left and right frontoparietal (±16%) (A), left and right temporo-occipital (±14%) (B), left frontoparietal and temporo-occipital (±15%) (C), and right frontoparietal and temporo-occipital (±15) sensor positions (D) during d 1, 3, and 7 (only preterm subgroups included).
Limits of agreement according to Bland and Altman (dotted lines) including all infants between NIRS-calculated cFTOE between left and right frontoparietal (±0.17) (A), left and right temporo-occipital (±0.16) (B), left frontoparietal and temporo-occipital (±0.18) (C), and right frontoparietal and temporo-occipital (±0.16) sensor positions (D) during d 1, 3, and 7 (only preterm subgroups included).
DISCUSSION
The present data show that simultaneously NIRS-determined rScO2 and extraction (cFTOE) for the different brain regions as investigated in this study, the right and left frontoparietal regions and the right and left temporo-occipital regions, is not different. Furthermore, a decrease and increase occurred within the first week of life, which is in agreement with others who investigated this issue in newly born infants (15,16). However, we must also conclude that differences up to 18% can exist between the investigated brain regions for rScO2, regardless postnatal age or GA in this cohort of stable preterm and term neonates. Consequently, the limits of agreement of these variables between the brain regions investigated are therefore also quite large. It must be admitted, however, that in our study for analysis, 10-s sampled values were used. Because most studies use 1-min averaged values to estimate rScO2, limits of agreement will probably improve when calculating the 1-min average values (4).
What do these findings mean for monitoring cerebral oxygenation and extraction using NIRS in clinical practice? First, we noted that the obtained results confirmed those of an earlier study of our group in which we also found no substantial differences between rScO2 values simultaneously measured over the left compared with the right frontoparietal region of the brain in clinically stable (preterm) infants (10). The knowledge that there is also no consistent difference in cerebral saturation with the occipital regions of the brain strengthens our earlier suggestion that unilateral NIRS-monitoring can serve as a trend monitoring in the individual patient to detect substantial changes in rScO2 and cFTOE, larger than the limits of agreement, providing the physician with important clinical information (10). This seemed to be true despite the fact that the temporo-occipital region of the brain has a very high perfusion and metabolism, even in the preterm infant (9). At the same time, the present results stress again that rScO2 lacks the precision to be used as a robust quantitative variable of cerebral oxygenation, given the variability of rScO2 values between the respective regions of the brain and the quite large limits of agreement between these regions (4). In fact, more sensitive quantitative methods such as fNIRS, functional MRI, and PET scans can detect small differences between regions (17,18) but are less useful in daily clinical care with prolonged periods of registration. Furthermore, it remains to be investigated if during conditions with unstable hemodynamics and/or suboptimal systemic oxygenation, not uncommon in the sick preterm and term infant, single unilateral monitoring of rScO2 is still tenable. In fact, we found during significant drops in arterial saturation an uneven NIRS-measured rScO2 between left and right frontoparietal regions (10), advocating bilateral monitoring of rScO2 in the sick infant. Further additional studies in unstable infants are therefore necessary to further unravel this issue.
We found remarkably high rScO2 values in the present study in which we used the OxyAlert NIRSensor for Neonates. These values are substantially higher than those measured with the small adult sensor of the same NIRS device and which we are using routinely in clinical practice (1,10). Moreover, previous studies measuring rScO2 or with NIRS devices using the spatially resolved spectroscopy technique (19–22), which measures a comparable indicator of mixed cerebral oxygen saturation, the tissue oxygenation index (TOI), find lower values that are in line with earlier studies of our group and others using the rScO2 (1). These studies report reference values of rScO2 ranging between 61 and 75% for preterm and term infants with standard deviations of about 5 to 7% (1,20,21), whereas values in the present study are up to 10% higher as is the variability of the signal. These differences are probably related to differences in processing of the received light signal. According to the manufacturer, the neonatal OxyAlert NIRSensor has been engineered for higher sensitivity, and the algorithm used in the neonatal sensor is indeed adjusted for the stronger signal reflected because of the thinner skull of the child, which makes ambient light to enter the head more easily. These adaptations may account for the ∼10% higher mean values and the higher variability in the rScO2. However, the new neonatal sensor is optically identical to the pediatric sensor, as has been validated in comparison with blood samples in a piglet model (unpublished data). Another possibility for high rScO2 values may be possible interference between the four sensors attached to the skull. However, this seems very unlikely because the scheme of the preamplifier and the distances between the sensors prevent interference of the two connected transducers.
Although low Hb concentrations can influence oxygen delivery and especially extraction, it is not probable that this issue was important in our study group, because all infants were stable, and no low Hb values are reported (<8 mM) (23,24).
The present study has also some limitations. First, are there effects of changes of head and/or body position on rScO2? Although head position was not consistently registered, a recent report showed that changing the position of the head or body from supine to prone position, did not consistently change rScO2 values, at least not in the stable preterm baby (25). Furthermore, we did not relate the measured rScO2 and cFTOE values to the (physical) activity of the infant. Infants were mostly, but not always, in a quiet sleeping phase, and especially the term infants were more often moving and caring procedures were sometimes done while monitoring cerebral oxygenation. These activities and procedures may have influenced the detected values of rScO2 and cFTOE.
In conclusion, in the relatively stable preterm and term infant in the first days of life, no substantial differences of rScO2 and cFTOE between frontoparietal and temporo-occipital brain regions were detected. We suggest therefore that unilateral NIRS monitoring can serve as a trend monitoring in the individual patient to detect important changes in rScO2 and cFTOE in most situations and can provide us with important clinical information. With the development of new commercial machines and their different techniques and algorithms, it is mandatory to determine reliable reference values, which makes it possible to compare results between relevant studies.
Abbreviations
- cFTOE:
-
cerebral fractional tissue oxygen extraction
- NIRS:
-
near infrared spectroscopy
- rScO2:
-
regional cerebral oxygen saturation
- SaO2:
-
arterial oxygen saturation
- T1:
-
postnatal age 0–24 hours, day 1
- T2:
-
postnatal age 48–72 hours, day 3
- T3:
-
postnatal age 144–168 hours, day 7
References
van Bel F, Lemmers P, Naulaers G 2008 Monitoring neonatal regional cerebral oxygen saturation in clinical practice: value and pitfalls. Neonatology 94: 237–244
Naulaers G, Meyns B, Miserez M, Leunens V, Van Huffel S, Casaer P, Weindling M, Devlieger H 2007 Use of tissue oxygenation index and fractional tissue oxygen extraction as non-invasive parameters for cerebral oxygenation. A validation study in piglets. Neonatology 92: 120–126
Sorensen LC, Greisen G 2006 Precision of measurement of cerebral tissue oxygenation index using near-infrared spectroscopy in preterm neonates. J Biomed Opt 11: 054005
Greisen G 2006 Is near-infrared spectroscopy living up to its promises?. Semin Fetal Neonatal Med 11: 498–502
Toet MC, Lemmers PM 2009 Brain monitoring in neonates. Early Hum Dev 85: 77–84
Kamba M, Sung YW, Ogawa S 2007 Alteration of blood oxygenation level-dependent signaling by local circulatory condition. J Magn Reson Imaging 26: 1506–1513
Higami T, Kozawa S, Asada T, Obo H, Gan K, Iwahashi K, Nohara H 1999 Retrograde cerebral perfusion versus selective cerebral perfusion as evaluated by cerebral oxygen saturation during aortic arch reconstruction. Ann Thorac Surg 67: 1091–1096
Bartocci M, Winberg J, Papendieck G, Mustica T, Serra G, Lagercrantz H 2001 Cerebral hemodynamic response to unpleasant odors in the preterm newborn measured by near-infrared spectroscopy. Pediatr Res 50: 324–330
Chiron C, Jambaque I, Nabbout R, Lounes R, Syrota A, Dulac O 1997 The right brain hemisphere is dominant in human infants. Brain 120: 1057–1065
Lemmers PM, van Bel F 2009 Left-to-right differences of regional cerebral oxygen saturation and oxygen extraction in preterm infants during the first days of life. Pediatr Res 65: 226–230
Kussman BD, Wypij D, DiNardo JA, Newburger J, Jonas RA, Bartlett J, McGrath E, Laussen PC 2005 An evaluation of bilateral monitoring of cerebral oxygen saturation during pediatric cardiac surgery. Anesth Analg 101: 1294–1300
Andropoulos DB, Diaz LK, Fraser CD Jr, McKenzie ED, Stayer SA 2004 Is bilateral monitoring of cerebral oxygen saturation necessary during neonatal aortic arch reconstruction? Anesth Analg 98: 1267–1272, table of contents
Papile LA, Munsick-Bruno G, Schaefer A 1983 Relationship of cerebral intraventricular hemorrhage and early childhood neurologic handicaps. J Pediatr 103: 273–277
Lemmers PM, Toet MC, van Bel F 2008 Impact of patent ductus arteriosus and subsequent therapy with indomethacin on cerebral oxygenation in preterm infants. Pediatrics 121: 142–147
Verhagen EA, Keating P, Ter Horst HJ, Martijn A, Bos AF 2009 Cerebral oxygen saturation and extraction in preterm infants with transient periventricular echodensities. Pediatrics 124: 294–301
Roche-Labarbe N, Carp SA, Surova A, Patel M, Boas DA, Grant PE, Franceschini MA 2010 Noninvasive optical measures of CBV, StO(2), CBF index, and rCMRO(2) in human premature neonates' brains in the first six weeks of life. Hum Brain Mapp 31: 341–352
Wolf M, Greisen G 2009 Advances in near-infrared spectroscopy to study the brain of the preterm and term neonate. Clin Perinatol 36: 807–834, vi
Benders MJ, Hendrikse J, de Vries LS, van Bel F, Groenendaal F 2011 Phase-contrast magnetic resonance angiography measurements of global cerebral blood flow in the neonate. Pediatr Res 69: 544–547
Dullenkopf A, Frey B, Baenziger O, Gerber A, Weiss M 2003 Measurement of cerebral oxygenation state in anaesthetized children using the INVOS 5100 cerebral oximeter. Paediatr Anaesth 13: 384–391
Weiss M, Dullenkopf A, Kolarova A, Schulz G, Frey B, Baenziger O 2005 Near-infrared spectroscopic cerebral oxygenation reading in neonates and infants is associated with central venous oxygen saturation. Paediatr Anaesth 15: 102–109
Dullenkopf A, Kolarova A, Schulz G, Frey B, Baenziger O, Weiss M 2005 Reproducibility of cerebral oxygenation measurement in neonates and infants in the clinical setting using the NIRO 300 oximeter. Pediatr Crit Care Med 6: 344–347
Naulaers G, Morren G, Van HS, Casaer P, Devlieger H 2002 Cerebral tissue oxygenation index in very premature infants. Arch Dis Child Fetal Neonatal Ed 87: F189–F192
Dani C, Pratesi S, Fontanelli G, Barp J, Bertini G 2010 Blood transfusions increase cerebral, splanchnic, and renal oxygenation in anemic preterm infants. Transfusion 50: 1220–1226
van Hoften JC, Verhagen EA, Keating P, Ter Horst HJ, Bos AF 2010 Cerebral tissue oxygen saturation and extraction in preterm infants before and after blood transfusion. Arch Dis Child Fetal Neonatal Ed 95: F352–F358
Ancora G, Maranella E, Aceti A, Pierantoni L, Grandi S, Corvaglia L, Faldella G 2010 Effect of posture on brain hemodynamics in preterm newborns not mechanically ventilated. Neonatology 97: 212–217
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wijbenga, R., Lemmers, P. & van Bel, F. Cerebral Oxygenation During the First Days of Life in Preterm and Term Neonates: Differences Between Different Brain Regions. Pediatr Res 70, 389–394 (2011). https://doi.org/10.1203/PDR.0b013e31822a36db
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e31822a36db
This article is cited by
-
Cerebral oxygen saturation in neonates: a bedside comparison between neonatal and adult NIRS sensors
Pediatric Research (2023)
-
Neonatal NIRS monitoring: recommendations for data capture and review of analytics
Journal of Perinatology (2021)
-
Cerebral oxygen saturation and peripheral perfusion in the extremely premature infant with intraventricular and/or pulmonary haemorrhage early in life
Scientific Reports (2018)
-
Correlations between near-infrared spectroscopy, perfusion index, and cardiac outputs in extremely preterm infants in the first 72 h of life
European Journal of Pediatrics (2018)
-
Effects of antenatal magnesium sulfate treatment for neonatal neuro-protection on cerebral oxygen kinetics
Pediatric Research (2015)