Abstract
Background
Cerebral near-infrared spectroscopy is a non-invasive tool used to measure regional cerebral tissue oxygenation (rScO2) initially validated in adult and pediatric populations. Preterm neonates, vulnerable to neurologic injury, are attractive candidates for NIRS monitoring; however, normative data and the brain regions measured by the current technology have not yet been established for this population.
Methods
This study’s aim was to analyze continuous rScO2 readings within the first 6–72 h after birth in 60 neonates without intracerebral hemorrhage born at ≤1250 g and/or ≤30 weeks’ gestational age (GA) to better understand the role of head circumference (HC) and brain regions measured.
Results
Using a standardized brain MRI atlas, we determined that rScO2 in infants with smaller HCs likely measures the ventricular spaces. GA is linearly correlated, and HC is non-linearly correlated, with rScO2 readings. For HC, we infer that rScO2 is lower in infants with smaller HCs due to measuring the ventricular spaces, with values increasing in the smallest HCs as the deep cerebral structures are reached.
Conclusion
Clinicians should be aware that in preterm infants with small HCs, rScO2 displayed may reflect readings from the ventricular spaces and deep cerebral tissue.
Impact
-
Clinicians should be aware that in preterm infants with small head circumferences, cerebral near-infrared spectroscopy readings of rScO2 displayed may reflect readings from the ventricular spaces and deep cerebral tissue.
-
This highlights the importance of rigorously re-validating technologies before extrapolating them to different populations.
-
Standard rScO2 trajectories should only be established after determining whether the mathematical models used in NIRS equipment are appropriate in premature infants and the brain region(s) NIRS sensors captures in this population, including the influence of both gestational age and head circumference.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request. De-identified NIRS data are subject to an institutional data use agreement. Fetal T2 MRI brain images in the Harvard Fetal Brain Atlas are available online at http://crl.med.harvard.edu/research/fetal_brain_atlas/.
References
Alderliesten et al. Reference values of regional cerebral oxygen saturation during the first 3 days of life in preterm neonates. Pediatr. Res. 79, 55–64 (2016).
Vaidya, R. et al. Utilizing near infra-red spectroscopy to identify physiologic variations during digital retinal imaging in preterm infants. J. Perinatol. 42, 378–384. https://doi.org/10.1038/s41372-021-01294-1 (2022).
Tataranno, M. L. et al. Early oxygen-utilization and brain activity in preterm infants. PLoS One 10, e0124623 (2015).
Vesoulis, Z. A., Mintzer, J. P. & Chock, V. Y. Neonatal NIRS monitoring: recommendations for data capture and review of analytics. J. Perinatol. 41, 675–688 (2021).
Pichler, G. et al. Cerebral regional tissue Oxygen Saturation to Guide Oxygen Delivery in preterm neonates during immediate transition after birth (COSGOD III): multicentre randomised phase 3 clinical trial. BMJ 380, e072313 (2023).
Chock, V. Y. et al. Cerebral oxygenation and autoregulation in preterm infants (Early NIRS Study). J. Pediatr. 227, 94–100.e101 (2020).
Mintzer, J. P. & Moore, J. E. Regional tissue oxygenation monitoring in the neonatal intensive care unit: evidence for clinical strategies and future directions. Pediatr. Res. 86, 296–304 (2019).
Gilmore, J. H., Knickmeyer, R. C. & Gao, W. Imaging structural and functional brain development in early childhood. Nat. Rev. Neurosci. 19, 123–137 (2018).
Hansen, M. L. et al. Cerebral near-infrared spectroscopy monitoring versus treatment as usual for extremely preterm infants: a protocol for the SafeBoosC randomised clinical phase III trial. Trials 20, 811 (2019).
Pichler, G. et al. Reference ranges for regional cerebral tissue oxygen saturation and fractional oxygen extraction in neonates during immediate transition after birth. J. Pediatr. 163, 1558–1563 (2013).
Mohamed et al. Changes in cerebral tissue oxygenation and fractional oxygen extraction with gestational age and postnatal maturation in preterm infants. J. Perinatol. 41, 836–842 (2021).
Hyttel-Sorensen et al. Cerebral near-infrared spectroscopy monitoring for prevention of brain injury in very preterm infants. Cochrane Database Syst. Rev. 9, Cd011506 (2017).
Hyttel-Sorensen et al. A phase II randomized clinical trial on cerebral near-infrared spectroscopy plus a treatment guideline versus treatment as usual for extremely preterm infants during the first three days of life (SafeBoosC): study protocol for a randomized controlled trial. Trials 14, 120 (2013).
Medtronic. Quick Reference Guide For Premature Neonates. Product Guide. Medtronic. Boulder, CO. (2021).
Garvey, A. A. & Dempsey, E. M. Applications of near infrared spectroscopy in the neonate. Curr. Opin. Pediatr. 30, 209–215 (2018).
Dix, L. M. et al. Comparing near-infrared spectroscopy devices and their sensors for monitoring regional cerebral oxygen saturation in the neonate. Pediatr. Res. 74, 557–563 (2013).
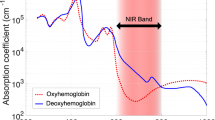
Kamran, M. A., Mannann, M. M. N. & Jeong, M. Y. Differential path-length factor’s effect on the characterization of brain’s hemodynamic response function: a functional near-infrared study. Front Neuroinform 12, 37 (2018).
Andresen, B., Greisen, G. & Hyttel-Sorensen, S. Comparison of INVOS 5100C and Nonin SenSmart X-100 oximeter performance in preterm infants with spontaneous apnea. Pediatr. Res. 87, 1244–1250 (2020).
Zhang, Y. et al. Neonate and infant brain development from birth to 2 years assessed using MRI-based quantitative susceptibility mapping. Neuroimage 185, 349–360 (2019).
Law, J. B. et al. Intracranial hemorrhage and 2-year neurodevelopmental outcomes in infants born extremely preterm. J. Pediatr. 238, 124–134.e110 (2021).
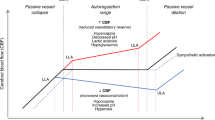
Rhee, C. J. et al. Neonatal cerebrovascular autoregulation. Pediatr. Res. 84, 602–610 (2018).
Covidien. Operations Manual INVOS® System, Model 5100C (2013).
Li, Z. et al. A statistical skull geometry model for children 0-3 years old. PLoS One 10, e0127322 (2015).
Gholipour, A. et al. A normative spatiotemporal MRI atlas of the fetal brain for automatic segmentation and analysis of early brain growth. Sci. Rep. 7, 476 (2017).
Jenkinson, M. et al. FSL. Neuroimage 62, 782–790 (2012).
Computational Radiology Laboratory at Boston Children’s Hospital. (ed. Gholipour, A.) Harvard Fetal Brain Atlas (Boston, MA). (2017).
Liang, K. Y. & Zeger, S. L. Regression analysis for correlated data. Annu. Rev. Public Health 14, 43–68 (1993).
R: A Language and Environment for Statistical Computing (R Core Team, 2019).
Duncan, A. et al. Optical pathlength measurements on adult head, calf and forearm and the head of the newborn infant using phase resolved optical spectroscopy. Phys. Med. Biol. 40, 295–304 (1995).
Demel, A. et al. Correlation between skin, bone, and cerebrospinal fluid layer thickness and optical coefficients measured by multidistance frequency-domain near-infrared spectroscopy in term and preterm infants. J. Biomed. Opt. 19, 17004 (2014).
Ostojic, D. et al. Impact of skull thickness on cerebral NIRS oximetry in neonates: an in silico study. Adv. Exp. Med. Biol. 1232, 33–38 (2020).
Delpy, D. T. et al. Estimation of optical pathlength through tissue from direct time of flight measurement. Phys. Med. Biol. 33, 1433–1442 (1988).
Jaekel, J. et al. Head growth and intelligence from birth to adulthood in very preterm and term born individuals. J. Int. Neuropsychol. Soc. 25, 48–56 (2019).
Bushby, K. M. et al. Centiles for adult head circumference. Arch. Dis. Child 67, 1286–1287 (1992).
Li, T., Gong, H. & Luo, Q. Visualization of light propagation in visible Chinese human head for functional near-infrared spectroscopy. J. Biomed. Opt. 16, 045001 (2011).
Hoshi, Y. Functional near-infrared spectroscopy: current status and future prospects. J. Biomed. Opt. 12, 062106 (2007).
Okada, E. et al. Theoretical and experimental investigation of near-infrared light propagation in a model of the adult head. Appl Opt. 36, 21–31 (1997).
Okada, E. & Delpy, D. T. Near-infrared light propagation in an adult head model. I. Modeling of low-level scattering in the cerebrospinal fluid layer. Appl Opt. 42, 2906–2914 (2003).
Owen-Reece, H. et al. Near infrared spectroscopy. Br. J. Anaesth. 82, 418–426 (1999).
Yoshitani, K. et al. Measurements of optical pathlength using phase-resolved spectroscopy in patients undergoing cardiopulmonary bypass. Anesth. Analg. 104, 341–346 (2007).
Svaasand, L. O. & Ellingsen, R. Optical properties of human brain. Photochem. Photobio. 38, 293–299 (1983).
Barkovich, A. J. Magnetic resonance techniques in the assessment of myelin and myelination. J. Inherit. Metab. Dis. 28, 311–343 (2005).
Suppan, E. et al. Three physiological components that influence regional cerebral tissue oxygen saturation. Front. Pediatr. 10, 913223 (2022).
Kratzer, I., Chip, S. & Vexler, Z. S. Barrier mechanisms in neonatal stroke. Front. Neurosci. 8, 359 (2014).
Jiang, D. et al. Vessel-specific quantification of neonatal cerebral venous oxygenation. Magn. Reson. Med. 82, 1129–1139 (2019).
Schwaberger, B. et al. Cerebral blood volume during neonatal transition in term and preterm infants with and without respiratory support. Front. Pediatr. 6, 132 (2018).
Dawson, J. A. et al. Defining the reference range for oxygen saturation for infants after birth. Pediatrics 125, e1340–e1347 (2010).
Baytur, Y. B. et al. Assessment of fetal cerebral arterial and venous blood flow before and after vaginal delivery or Cesarean section. Ultrasound Obstet. Gynecol. 24, 522–528 (2004).
Baik, N. et al. Blood pressure during the immediate neonatal transition: is the mean arterial blood pressure relevant for the cerebral regional oxygenation? Neonatology 112, 97–102 (2017).
Laurichesse-Delmas, H. et al. Color Doppler study of the venous circulation in the fetal brain and hemodynamic study of the cerebral transverse sinus. Ultrasound Obstet. Gynecol. 13, 34–42 (1999).
Sood, B. G., McLaughlin, K. & Cortez, J. Near-infrared spectroscopy: applications in neonates. Semin. Fetal Neonatal Med. 20, 164–172 (2015).
Baenziger, O. et al. The influence of the timing of cord clamping on postnatal cerebral oxygenation in preterm neonates: a randomized, controlled trial. Pediatrics 119, 455–459 (2007).
Tobias, J. D. Assessment of cerebral oxygenation using near infrared spectroscopy during isovolemic hemodilution in pediatric patients. J. Clin. Monit. Comput. 25, 171–174 (2011).
Kurth, C. D. & Uher, B. Cerebral hemoglobin and optical pathlength influence near-infrared spectroscopy measurement of cerebral oxygen saturation. Anesth. Analg. 84, 1297–1305 (1997).
Zhang, Y. et al. Cerebral near-infrared spectroscopy analysis in preterm infants with intraventricular hemorrhage. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2011, 1937–1940 (2011).
Pavlek, L. R. et al. Near-infrared spectroscopy in extremely preterm infants. Front. Pediatr. 8, 624113 (2020).
Beausoleil, T. P. et al. Cerebral oxygen saturation and peripheral perfusion in the extremely premature infant with intraventricular and/or pulmonary haemorrhage early in life. Sci. Rep. 8, 6511 (2018).
Korček, P. et al. The role of near-infrared spectroscopy monitoring in preterm infants. J. Perinatol. 37, 1070–1077 (2017).
Kahn, R. A. & Anyanwu, A. Near-infrared spectroscopy in vegetables and humans: an observational study. Eur. J. Anaesthesiol. 35, 907–910 (2018).
Acknowledgements
We would like to thank the nursing staff at the University of Washington Medical Center in Seattle, Washington, who provided excellent bedside care to the neonates throughout data collection.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The study was supported by an internal grant provided by the Division of Child Neurology at Seattle Children’s Hospital.
Author information
Authors and Affiliations
Contributions
Substantial contributions to the conception and design, acquisition of data, or analysis and interpretation of data: S.E.K., R.M., O.B., J.B.L., N.N., M.D., T.R.W., P.D.M., U.M. Drafting the article or revising it critically for important intellectual content: S.E.K., T.R.W., P.M., U.M. Final approval of the version to be published: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kolnik, S.E., Marquard, R., Brandon, O. et al. Preterm infants variability in cerebral near-infrared spectroscopy measurements in the first 72-h after birth. Pediatr Res 94, 1408–1415 (2023). https://doi.org/10.1038/s41390-023-02618-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02618-x