Abstract
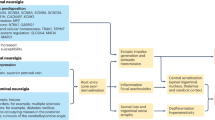
Trans-sphenoidal neurosurgery is the gold standard treatment for pituitary adenomas, but it can be contraindicated or ineffective. Stereotactic radiosurgery is a procedure aimed at controlling hormone hypersecretion and tumor size of pituitary adenomas. This Review discusses the long-term efficacy and adverse effects of stereotactic radiosurgery with the Gamma Knife® in secreting and nonsecreting pituitary adenomas. Long-term data confirm the antisecretory efficacy of the procedure (about 50% remission in hypersecreting tumors) but also a previously unknown low risk of recurrence (2–10% of cases). The time to remission is estimated to range from 12 to 60 months. The antitumoral efficacy of this treatment against nonsecreting tumors is observed in about 90% of cases. Hypopituitarism is the main adverse effect, observed in 20–40% of cases. Comparisons with conventional fractionated radiotherapy reveal a lower rate of remission with Gamma Knife® radiosurgery, counterbalanced by a more rapid efficacy and a lower rate of hypopituitarism. Short-term follow-up results on stereotactic fractionated radiotherapy suggest a risk of hypopituitarism similar to the one observed with radiosurgery. Therefore, stereotactic radiosurgery is probably still useful to treat some cases of pituitary adenoma, despite the fact that antisecretory drugs, particularly for acromegaly and prolactinomas, are becoming more effective and are well tolerated, thus increasing the probability of success with nonsurgical therapy.
Key Points
-
Gamma knife radiosurgery is a neurosurgical technique that uses radiation aimed at controlling hormonal secretion and tumor volume in pituitary adenomas
-
Antisecretory efficacy is observed in 40–50% of cases of secreting adenomas; the main predictive factors are low target volume, low initial hormone levels and possibly concomitant medication at the time of radiosurgery
-
Antitumoral efficacy is observed in more than 90–95% of cases of nonsecreting adenomas
-
The long-term recurrence risk is substantial, particularly in Cushing disease, where 10–20% of cases recur, usually several years after the radiosurgical procedure
-
The main adverse effect is hypopituitarism, observed in 20–40% of cases, whose risk increases with time after radiosurgery, decreasing after about 120 months
-
Results from long-term follow-up studies do not modify our current algorithms for treating pituitary adenomas, but they draw attention to the necessity for a regular follow-up after radiosurgery
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Chanson, P. & Salenave, S. Acromegaly. Orphanet J. Rare Dis. 3, 17 (2008).
Newell-Price, J., Bertagna, X., Grossman, A. B. & Nieman, L. K. Cushing's syndrome. Lancet 367, 1605–1617 (2006).
Brue, T., Delemer, B. & French Society of Endocrinology (SFE) work group on the consensus on hyperprolactinemia. Diagnosis and management of hyperprolactinemia: expert consensus—French Society of Endocrinology. Ann. Endocrinol. (Paris) 68, 58–64 (2007).
Dekkers, O. M., Pereira, A. M. & Romijn, J. A. Treatment and follow-up of clinically nonfunctioning pituitary macroadenomas. J. Clin. Endocrinol. Metab. 93, 3717–3726 (2008).
Eastman, R. C., Gorden, P., Glatstein, E. & Roth, J. Radiation therapy of acromegaly. Endocrinol. Metab. Clin. North Am. 21, 693–712 (1992).
Minniti, G., Gilbert, D. C. & Brada, M. Modern techniques for pituitary radiotherapy. Rev. Endocr. Metab. Disord. 10, 135–144 (2009).
Brada, M. & Jankowska, P. Radiotherapy for pituitary adenomas. Endocrinol. Metab. Clin. North Am. 37, 263–275 (2008).
Chen, C. C., Chapman, P., Petit, J. & Loeffler, J. Proton radiosurgery in neurosurgery. Neurosurg. Focus 23, E5 (2007).
Adler, J. R. Jr, Gibbs, I. C., Puataweepong, P. & Chang, S. D. Visual field preservation after multisession cyberknife radiosurgery for perioptic lesions. Neurosurgery 59, 244–254 (2006).
Tuniz, F. et al. Multisession cyberknife stereotactic radiosurgery of large, benign cranial base tumors: preliminary study. Neurosurgery 65, 898–907 (2009).
Castinetti, F., Morange, I., Dufour, H., Regis, J. & Brue, T. Radiotherapy and radiosurgery in acromegaly. Pituitary 12, 3–10 (2009).
Castinetti, F. et al. Long-term results of stereotactic radiosurgery in secretory pituitary adenomas. J. Clin. Endocrinol. Metab. 94, 3400–3407 (2009).
Ronchi, C. L. et al. Efficacy and tolerability of gamma knife radiosurgery in acromegaly: a 10-year follow-up study. Clin. Endocrinol. (Oxf.) 71, 846–852 (2009).
Pouratian, N. et al. Gamma knife radiosurgery for medically and surgically refractory prolactinomas. Neurosurgery 59, 255–266 (2006).
Jagannathan, J. et al. Gamma knife surgery for Cushing's disease. J. Neurosurg. 106, 980–987 (2007).
Jagannathan, J. et al. Gamma knife radiosurgery for acromegaly: outcomes after failed transsphenoidal surgery. Neurosurgery 62, 1262–1270 (2008).
Jezková, J. et al. Use of the Leksell gamma knife in the treatment of prolactinoma patients. Clin. Endocrinol. (Oxf.) 70, 732–741 (2008).
Jezková, J. et al. Gamma knife radiosurgery for acromegaly--long-term experience. Clin. Endocrinol. (Oxf.) 64, 588–595 (2006).
Vik-Mo, E. O. et al. Gamma knife stereotactic radiosurgery for acromegaly. Eur. J. Endocrinol. 157, 255–263 (2007).
Pollock, B. E., Jacob, J. T., Brown, P. D. & Nippoldt, T. B. Radiosurgery of growth hormone-producing pituitary adenomas: factors associated with biochemical remission. J. Neurosurg. 106, 833–838 (2007).
Losa, M. et al. The role of stereotactic radiotherapy in patients with growth hormone-secreting pituitary adenoma. J. Clin. Endocrinol. Metab. 93, 2546–2552 (2008).
Laws, E. R. et al. Stereotactic radiosurgery for pituitary adenomas: a review of the literature. J. Neurooncol. 69, 257–272 (2004).
Castinetti, F. et al. Outcome of gamma knife radiosurgery in 82 patients with acromegaly: correlation with initial hypersecretion. J. Clin. Endocrinol. Metab. 90, 4483–4488 (2005).
Landolt, A. M. et al. Octreotide may act as a radioprotective agent in acromegaly. J. Clin. Endocrinol. Metab. 85, 1287–1289 (2000).
Kobayashi, T., Kida, Y. & Mori, Y. Gamma knife radiosurgery in the treatment of Cushing disease: long-term results. J. Neurosurg. 97 (Suppl. 5), 422–428 (2002).
Höybye, C. et al. Adrenocorticotropic hormone-producing pituitary tumors: 12- to 22-year follow-up after treatment with stereotactic radiosurgery. Neurosurgery 49, 284–292 (2001).
Castinetti, F., Morange, I., Jaquet, P., Conte-Devolx, B. & Brue, T. Ketoconazole revisited: a preoperative or postoperative treatment in Cushing's disease. Eur. J. Endocrinol. 158, 91–99 (2008).
Castinetti, F. et al. Gamma knife radiosurgery is a successful adjunctive treatment in Cushing's disease. Eur. J. Endocrinol. 156, 91–98 (2007).
Stalla, G. K., Stalla, J., Loeffler, J. P., von Werder, K. & Müller, O. A. Pharmacological modulation of CRH-stimulated ACTH secretion by ketoconazole. Horm. Metab. Res. Suppl. 16, 31–36 (1987).
Pan, L. et al. Gamma knife radiosurgery as a primary treatment for prolactinomas. J. Neurosurg. 93 (Suppl. 3), 10–13 (2000).
Landolt, A. M. & Lomax, N. Gamma knife radiosurgery for prolactinomas. J. Neurosurg. 93 (Suppl. 3), 14–18 (2000).
Sheehan, J. P., Jagannathan, J., Pouratian, N. & Steiner, L. Stereotactic radiosurgery for pituitary adenomas: a review of the literature and our experience. Front. Horm. Res. 34, 185–205 (2006).
Pamir, M. N., Kiliç, T., Belirgen, M., Abacioglu, U. & Karabekiroglu, N. Pituitary adenomas treated with gamma knife radiosurgery: volumetric analysis of 100 cases with minimum 3 year follow-up. Neurosurgery 61, 270–280 (2007).
Pollock, B. E. et al. Gamma knife radiosurgery for patients with nonfunctioning pituitary adenomas: results from a 15-year experience. Int. J. Radiat. Oncol. Biol. Phys. 70, 1325–1329 (2008).
Höybye, C. & Rähn, T. Adjuvant Gamma Knife radiosurgery in non-functioning pituitary adenomas; low risk of long-term complications in selected patients. Pituitary 12, 211–216 (2009).
Mingione, V. et al. Gamma surgery in the treatment of nonsecretory pituitary macroadenoma. J. Neurosurg. 104, 876–883 (2006).
Castinetti, F. et al. Outcome of gamma knife radiosurgery in 82 patients with acromegaly: correlation with initial hypersecretion. J. Clin. Endocrinol. Metab. 90, 4483–4488 (2005).
Brada, M., Ajithkumar, T. V. & Minniti, G. Radiosurgery for pituitary adenomas. Clin. Endocrinol. (Oxf.) 61, 531–543 (2004).
Tishler, R. B. et al. Tolerance of cranial nerves of the cavernous sinus to radiosurgery. Int. J. Radiat. Oncol. Biol. Phys. 27, 215–221 (1993).
Jagannathan, J., Yen, C. P., Pouratian, N., Laws, E. R. & Sheehan, J. P. Stereotactic radiosurgery for pituitary adenomas: a comprehensive review of indications, techniques and long-term results using the Gamma Knife. J. Neurooncol. 92, 345–356 (2009).
Rowe, J. et al. Risk of malignancy after gamma knife stereotactic radiosurgery. Neurosurgery 60, 60–66 (2007).
Voges, J. et al. Linear accelerator radiosurgery for pituitary macroadenomas: a 7-year follow-up study. Cancer 107, 1355–1364 (2006).
Chen, C. C., Chapman, P., Petit, J. & Loeffler, J. Proton radiosurgery in neurosurgery. Neurosurg. Focus 23, E5 (2007).
Petit, J. H. et al. Proton stereotactic radiosurgery in management of persistent acromegaly. Endocr. Pract. 13, 726–734 (2007).
Aghi, M. K. et al. Management of recurrent and refractory Cushing's disease with reoperation and/or proton beam radiosurgery. Clin. Neurosurg. 55, 141–144 (2008).
Kim, J. W. et al. Preliminary report of multisession gamma knife radiosurgery for benign perioptic lesions: visual outcome in 22 patients. J. Korean Neurosurg. Soc. 44, 67–71 (2008).
Knisely, J. P., Bond, J. E., Yue, N. J., Studholme, C. & de Lotbinière, A. C. Image registration and calculation of a biologically effective dose for multisession radiosurgical treatments. Technical note. J. Neurosurg. 93 (Suppl. 3), 208–218 (2000).
Estrada, J. et al. The long-term outcome of pituitary irradiation after unsuccessful transsphenoidal surgery in Cushing's disease. N. Engl. J. Med. 336, 172–177 (1997).
Jenkins, P. J., Bates, P., Carson, M. N., Stewart, P. M. & Wass, J. A. Conventional pituitary irradiation is effective in lowering serum growth hormone and insulin-like growth factor-I in patients with acromegaly. J. Clin. Endocrinol. Metab. 91, 1239–1245 (2006).
McCord, M. W. et al. Radiotherapy for pituitary adenoma: long-term outcome and sequelae. Int. J. Radiat. Oncol. Biol. Phys. 39, 437–444 (1997).
Biermasz, N. R., van Dulken, H. & Roelfsema, F. Long-term follow-up results of postoperative radiotherapy in 36 patients with acromegaly. J. Clin. Endocrinol. Metab. 85, 2476–2482 (2000).
Barrande, G. et al. Hormonal and metabolic effects of radiotherapy in acromegaly: long-term results in 128 patients followed in a single center. J. Clin. Endocrinol. Metab. 85, 3779–3785 (2000).
Sonino, N., Zielezny, M., Fava, G. A., Fallo, F. & Boscaro, M. Risk factors and long-term outcome in pituitary-dependent Cushing's disease. J. Clin. Endocrinol. Metab. 81, 2647–2652 (1996).
al-Mefty, O., Kersh, J. E., Routh, A. & Smith, R. R. The long-term side effects of radiation therapy for benign brain tumors in adults. J. Neurosurg. 73, 502–512 (1990).
Mokry, M., Ramschak-Schwarzer, S., Simbrunner, J., Ganz, J. C. & Pendl, G. A six year experience with the postoperative radiosurgical management of pituitary adenomas. Stereotact. Funct. Neurosurg. 72 (Suppl. 1), 88–100 (1999).
Brada, M. et al. Risk of second brain tumour after conservative surgery and radiotherapy for pituitary adenoma. BMJ 304, 1343–1346 (1992).
Erfurth, E. M., Bülow, B., Mikoczy, Z., Svahn-Tapper, G. & Hagmar, L. Is there an increase in second brain tumours after surgery and irradiation for a pituitary tumour? Clin. Endocrinol. (Oxf.) 55, 613–616 (2001).
Tsang, R. W. et al. Glioma arising after radiation therapy for pituitary adenoma. A report of four patients and estimation of risk. Cancer 72, 2227–2233 (1993).
Colin, P. et al. Treatment of pituitary adenomas by fractionated stereotactic radiotherapy: a prospective study of 110 patients. Int. J. Radiat. Oncol. Biol. Phys. 62, 333–341 (2005).
Minniti, G., Traish, D., Ashley, S., Gonsalves, A. & Brada, M. Fractionated stereotactic conformal radiotherapy for secreting and nonsecreting pituitary adenomas. Clin. Endocrinol. (Oxf.) 64, 542–548 (2006).
Biermasz, N. R., van Dulken, H. & Roelfsema, F. Ten-year follow-up results of transsphenoidal microsurgery in acromegaly. J. Clin. Endocrinol. Metab. 85, 4596–4602 (2000).
Freda, P. U., Wardlaw, S. L. & Post, K. D. Long-term endocrinological follow-up evaluation in 115 patients who underwent transsphenoidal surgery for acromegaly. J. Neurosurg. 89, 353–358 (1998).
Swearingen, B. et al. Long-term mortality after transsphenoidal surgery and adjunctive therapy for acromegaly. J. Clin. Endocrinol. Metab. 83, 3419–3426 (1998).
Shimon, I., Cohen, Z. R., Ram, Z. & Hadani, M. Transsphenoidal surgery for acromegaly: endocrinological follow-up of 98 patients. Neurosurgery 48, 1239–1245 (2001).
Atkinson, A. B., Kennedy, A., Wiggam, M. I., McCance, D. R. & Sheridan, B. Long-term remission rates after pituitary surgery for Cushing's disease: the need for long-term surveillance. Clin. Endocrinol. (Oxf.) 63, 549–559 (2005).
Chee, G. H., Mathias, D. B., James, R. A. & Kendall-Taylor, P. Transsphenoidal pituitary surgery in Cushing's disease: can we predict outcome? Clin. Endocrinol. (Oxf.) 54, 617–626 (2001).
Rees, D. A. et al. Long-term follow-up results of transsphenoidal surgery for Cushing's disease in a single centre using strict criteria for remission. Clin. Endocrinol. (Oxf.) 56, 541–551 (2002).
Shimon, I., Ram, Z., Cohen, Z. R. & Hadani, M. Transsphenoidal surgery for Cushing's disease: endocrinological follow-up monitoring of 82 patients. Neurosurgery 51, 57–62 (2002).
Utz, A. L., Swearingen, B. & Biller, B. M. Pituitary surgery and postoperative management in Cushing's disease. Endocrinol. Metab. Clin. North Am. 34, 459–478 (2005).
Melmed, S. et al. Guidelines for acromegaly management: an update. J. Clin. Endocrinol. Metab. 94, 1509–1517 (2009).
Casanueva, F. F. et al. Guidelines of the Pituitary Society for the diagnosis and management of prolactinomas. Clin. Endocrinol. (Oxf.) 65, 265–273 (2006).
Biller, B. M. et al. Treatment of adrenocorticotropin-dependent Cushing's syndrome: a consensus statement. J. Clin. Endocrinol. Metab. 93, 2454–2462 (2008).
Dekkers, O. M., Pereira, A. M. & Romijn, J. A. Treatment and follow-up of clinically nonfunctioning pituitary macroadenomas. J. Clin. Endocrinol. Metab. 93, 3717–3726 (2008).
Acknowledgements
Charles P. Vega, University of California, Irvine, CA, is the author of and is solely responsible for the content of the learning objectives, questions and answers of the MedscapeCME-accredited continuing medical education activity associated with this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
J. Régis has received research support from the following companies: Accuray, Brainlab, Elekta, TomoTherapy. The other authors, the Journal Editor V. Heath and the CME questions author C. P. Vega declare no competing interests.
Rights and permissions
About this article
Cite this article
Castinetti, F., Régis, J., Dufour, H. et al. Role of stereotactic radiosurgery in the management of pituitary adenomas. Nat Rev Endocrinol 6, 214–223 (2010). https://doi.org/10.1038/nrendo.2010.4
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrendo.2010.4
This article is cited by
-
Endocrine disorders after primary gamma knife radiosurgery for pituitary adenomas: A systematic review and meta-analysis
Pituitary (2022)
-
Characterization of the ability of a, second-generation SST-DA chimeric molecule, TBR-065, to suppress GH secretion from human GH-secreting adenoma cells
Pituitary (2021)
-
Aggressive pituitary neuroendocrine tumors: current practices, controversies, and perspectives, on behalf of the EANS skull base section
Acta Neurochirurgica (2021)
-
Initial Gamma Knife radiosurgery for nonfunctioning pituitary adenomas: results from a 26-year experience
Endocrine (2020)
-
Transsphenoidal resection for pituitary adenoma in elderly versus younger patients: a systematic review and meta-analysis
Acta Neurochirurgica (2020)