Abstract
High-fidelity intracranial electrode arrays for recording and stimulating brain activity have facilitated major advances in the treatment of neurological conditions over the past decade. Traditional arrays require direct implantation into the brain via open craniotomy, which can lead to inflammatory tissue responses, necessitating development of minimally invasive approaches that avoid brain trauma. Here we demonstrate the feasibility of chronically recording brain activity from within a vein using a passive stent-electrode recording array (stentrode). We achieved implantation into a superficial cortical vein overlying the motor cortex via catheter angiography and demonstrate neural recordings in freely moving sheep for up to 190 d. Spectral content and bandwidth of vascular electrocorticography were comparable to those of recordings from epidural surface arrays. Venous internal lumen patency was maintained for the duration of implantation. Stentrodes may have wide ranging applications as a neural interface for treatment of a range of neurological conditions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Deuschl, G. et al. A randomized trial of deep-brain stimulation for Parkinson's disease. N. Engl. J. Med. 355, 896–908 (2006).
Mallet, L. et al. Subthalamic nucleus stimulation in severe obsessive-compulsive disorder. N. Engl. J. Med. 359, 2121–2134 (2008).
Wilson, B.S. et al. Better speech recognition with cochlear implants. Nature 352, 236–238 (1991).
Weiland, J.D., Cho, A.K. & Humayun, M.S. Retinal prostheses: current clinical results and future needs. Ophthalmology 118, 2227–2237 (2011).
Hochberg, L.R. et al. Reach and grasp by people with tetraplegia using a neurally controlled robotic arm. Nature 485, 372–375 (2012).
Morrell, M.J. Responsive cortical stimulation for the treatment of medically intractable partial epilepsy. Neurology 77, 1295–1304 (2011).
Cook, M.J. et al. Prediction of seizure likelihood with a long-term, implanted seizure advisory system in patients with drug-resistant epilepsy: a first-in-man study. Lancet Neurol. 12, 563–571 (2013).
Hochberg, L.R. et al. Neuronal ensemble control of prosthetic devices by a human with tetraplegia. Nature 442, 164–171 (2006).
Yanagisawa, T. et al. Electrocorticographic control of a prosthetic arm in paralyzed patients. Ann. Neurol. 71, 353–361 (2012).
Wang, W. et al. An electrocorticographic brain interface in an individual with tetraplegia. PLoS One 8, e55344 (2013).
Polikov, V.S., Tresco, P.A. & Reichert, W.M. Response of brain tissue to chronically implanted neural electrodes. J. Neurosci. Methods 148, 1–18 (2005).
Karumbaiah, L. et al. Relationship between intracortical electrode design and chronic recording function. Biomaterials 34, 8061–8074 (2013).
Saxena, T. et al. The impact of chronic blood-brain barrier breach on intracortical electrode function. Biomaterials 34, 4703–4713 (2013).
Yanagisawa, T. et al. Neural decoding using gyral and intrasulcal electrocorticograms. Neuroimage 45, 1099–1106 (2009).
Driller, J. et al. Development and use of the POD catheter in the cerebral vascular system. Med. Res. Eng. 8, 11–16 (1969).
Penn, R.D., Hilal, S.K., Michelsen, W.J., Goldensohn, E.S. & Driller, J. Intravascular intracranial EEG recording. Technical note. J. Neurosurg. 38, 239–243 (1973).
Boniface, S.J. & Antoun, N. Endovascular electroencephalography: the technique and its application during carotid amytal assessment. J. Neurol. Neurosurg. Psychiatry 62, 193–195 (1997).
Bower, M.R. et al. Intravenous recording of intracranial, broadband EEG. J. Neurosci. Methods 214, 21–26 (2013).
Mikuni, N. et al. “Cavernous sinus EEG”: a new method for the preoperative evaluation of temporal lobe epilepsy. Epilepsia 38, 472–482 (1997).
Watanabe, H., Takahashi, H., Nakao, M., Walton, K. & Llinás, R.R. Intravascular neural interface with nanowire electrode. Electron. Commun. Jpn. 92, 29–37 (2009).
Furman, S. & Schwedel, J.B. An intracardiac pacemaker for Stokes-Adams seizures. N. Engl. J. Med. 261, 943–948 (1959).
Mirowski, M. et al. Termination of malignant ventricular arrhythmias with an implanted automatic defibrillator in human beings. N. Engl. J. Med. 303, 322–324 (1980).
Chimowitz, M.I. et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N. Engl. J. Med. 365, 993–1003 (2011).
Puffer, R.C., Mustafa, W. & Lanzino, G. Venous sinus stenting for idiopathic intracranial hypertension: a review of the literature. J. Neurointerv. Surg. 5, 483–486 (2013).
Berkhemer, O.A. et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N. Engl. J. Med. 372, 11–20 (2015).
Campbell, B.C.V. et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N. Engl. J. Med. 372, 1009–1018 (2015).
Hoffmann, A. et al. The ovine cerebral venous system: comparative anatomy, visualization, and implications for translational research. PLoS One 9, e92990 (2014).
Shao, Y., Sun, J.-L., Yang, Y., Cui, Q.-K. & Zhang, Q.-L. Endoscopic and microscopic anatomy of the superior sagittal sinus and torcular herophili. J. Clin. Neurosci. 16, 421–424 (2009).
Van Belle, E. et al. Stent endothelialization. Time course, impact of local catheter delivery, feasibility of recombinant protein administration, and response to cytokine expedition. Circulation 95, 438–448 (1997).
van der Giessen, W.J. et al. Coronary stenting with a new, radiopaque, balloon-expandable endoprosthesis in pigs. Circulation 83, 1788–1798 (1991).
Franks, W., Schenker, I., Schmutz, P. & Hierlemann, A. Impedance characterization and modeling of electrodes for biomedical applications. IEEE Trans. Biomed. Eng. 52, 1295–1302 (2005).
Henle, C. et al. First long term in vivo study on subdurally implanted micro-ECoG electrodes, manufactured with a novel laser technology. Biomed. Microdevices 13, 59–68 (2011).
Cedzich, C., Taniguchi, M., Schäfer, S. & Schramm, J. Somatosensory evoked potential phase reversal and direct motor cortex stimulation during surgery in and around the central region. Neurosurgery 38, 962–970 (1996).
Allison, T. et al. Human cortical potentials evoked by stimulation of the median nerve. I. Cytoarchitectonic areas generating short-latency activity. J. Neurophysiol. 62, 694–710 (1989).
Lukatch, H.S., Kiddoo, C.E. & Maciver, M.B. Anesthetic-induced burst suppression EEG activity requires glutamate-mediated excitatory synaptic transmission. Cereb. Cortex 15, 1322–1331 (2005).
Shimoda, K., Nagasaka, Y., Chao, Z.C. & Fujii, N. Decoding continuous three-dimensional hand trajectories from epidural electrocorticographic signals in Japanese macaques. J. Neural Eng. 9, 036015 (2012).
Bundy, D.T. et al. Characterization of the effects of the human dura on macro- and micro-electrocorticographic recordings. J. Neural Eng. 11, 016006 (2014).
Torres Valderrama, A., Oostenveld, R., Vansteensel, M.J., Huiskamp, G.M. & Ramsey, N.F. Gain of the human dura in vivo and its effects on invasive brain signal feature detection. J. Neurosci. Methods 187, 270–279 (2010).
Stoney, W.S. et al. The incidence of venous thrombosis following long-term transvenous pacing. Ann. Thorac. Surg. 22, 166–170 (1976).
Teplitzky, B.A., Connolly, A.T., Bajwa, J.A. & Johnson, M.D. Computational modeling of an endovascular approach to deep brain stimulation. J. Neural Eng. 11, 026011–026014 (2014).
Ahmed, R.M. et al. Transverse sinus stenting for idiopathic intracranial hypertension: a review of 52 patients and of model predictions. AJNR Am. J. Neuroradiol. 32, 1408–1414 (2011).
Fortescue, E.B. et al. Patient, procedural, and hardware factors associated with pacemaker lead failures in pediatrics and congenital heart disease. Heart Rhythm 1, 150–159 (2004).
Ho, J.S. et al. Wireless power transfer to deep-tissue microimplants. Proc. Natl. Acad. Sci. USA 111, 7974–7979 (2014).
Muller, R. et al. A miniaturized 64-channel 225μW wireless electrocorticographic neural sensor. 2014 IEEE International Solid-State Circuits Conference (ISSCC) 412–413 (IEEE, 2014).
Sun, J., Wang, J., Jie, L., Wang, H. & Gong, X. Visualization of the internal cerebral veins on MR phase-sensitive imaging: comparison with 3D gadolinium-enhanced MR venography and fast-spoiled gradient recalled imaging. AJNR Am. J. Neuroradiol. 32, E191–E193 (2011).
Fedorov, A. et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn. Reson. Imaging 30, 1323–1341 (2012).
Dill, T. et al. Pulmonary vein diameter reduction after radiofrequency catheter ablation for paroxysmal atrial fibrillation evaluated by contrast-enhanced three-dimensional magnetic resonance imaging. Circulation 107, 845–850 (2003).
Dale, A.M., Fischl, B. & Sereno, M.I. Cortical surface-based analysis. I. Segmentation and surface reconstruction. Neuroimage 9, 179–194 (1999).
Fischl, B., Sereno, M.I. & Dale, A.M. Cortical surface-based analysis. II: Inflation, flattening, and a surface-based coordinate system. Neuroimage 9, 195–207 (1999).
Antiga, L. et al. An image-based modeling framework for patient-specific computational hemodynamics. Med. Biol. Eng. Comput. 46, 1097–1112 (2008).
Bagley, C. Cortical motor mechanism of the sheep brain. Arch. Neurol. Psychiatry 7, 417–453 (1922).
Simpson, S. & King, J.L. Localisation of the motor area in the sheep. Exp. Physiol. 4, 53–65 (1911).
Grovum, W.L. & Gonzalez, J.S. Electrical stimulation of the medial frontal lobe elicits a pattern of body movements in sheep. Brain Res. 851, 252–253 (1999).
Johnson, J.I., Rubel, E.W. & Hatton, G.I. Mechanosensory projections to cerebral cortex of sheep. J. Comp. Neurol. 158, 81–107 (1974).
Oostenveld, R., Fries, P., Maris, E. & Schoffelen, J.-M. FieldTrip: open source software for advanced analysis of MEG, EEG, and invasive electrophysiological data. Comput. Intell. Neurosci. 2011, 156869 (2011).
Metscher, B.D. MicroCT for comparative morphology: simple staining methods allow high-contrast 3D imaging of diverse non-mineralized animal tissues. BMC Physiol. 9, 11 (2009).
Stevenson, A.W. et al. First experiments on the Australian Synchrotron Imaging and Medical beamline, including investigations of the effective source size in respect of X-ray imaging. J. Synchrotron Radiat. 17, 75–80 (2010).
Morlacchi, S. et al. Hemodynamics and in-stent restenosis: micro-CT images, histology, and computer simulations. Ann. Biomed. Eng. 39, 2615–2626 (2011).
Nieman, K., Cademartiri, F., Raaijmakers, R., Pattynama, P. & de Feyter, P. Noninvasive angiographic evaluation of coronary stents with multi-slice spiral computed tomography. Herz 28, 136–142 (2003).
Williams, J.C., Hippensteel, J.A., Dilgen, J., Shain, W. & Kipke, D.R. Complex impedance spectroscopy for monitoring tissue responses to inserted neural implants. J. Neural Eng. 4, 410–423 (2007).
Ghoshal, N.G. & Getty, R. Innervation of the forearm and fin the ox (Bos taurus), sheep (Ovis aries) and goat (Capra hircus). Iowa State Univ. Vet. 29, 19–29 (1967).
Ogawa, T., Shingu, K., Shibata, M., Osawa, M. & Mori, K. The divergent actions of volatile anaesthetics on background neuronal activity and reactive capability in the central nervous system in cats. Can. J. Anaesth. 39, 862–872 (1992).
Villeneuve, M.Y. & Casanova, C. On the use of isoflurane versus halothane in the study of visual response properties of single cells in the primary visual cortex. J. Neurosci. Methods 129, 19–31 (2003).
Palahniuk, R.J., Shnider, S.M. & Eger, E.I. II. Pregnancy decreases the requirement for inhaled anesthetic agents. Anesthesiology 41, 82–83 (1974).
Chiappa, K.H. Evoked Potentials in Clinical Medicine (Lippincott Williams & Wilkins, 1997).
Rampil, I.J. A primer for EEG signal processing in anesthesia. Anesthesiology 89, 980–1002 (1998).
Thomson, D.J. Spectrum estimation and harmonic analysis. Proc. IEEE 70, 1055–1096 (1982).
Acknowledgements
The research was supported by US Defense Advanced Research Projects Agency (DARPA) Microsystems Technology Office contract N66001-12-1-4045; Office of Naval Research (ONR) Global N62909-14-1-N020; National Health and Medical Research Council of Australia (NHMRC) Project Grant APP1062532 and Development Grant APP1075117; Defence Health Foundation, Australia (Booster Grant); Defence Science Institute, Australia, grant; Brain Foundation, Australia, research gift; and the Victorian Government's Operational Infrastructure Support Program. T.J.O. acknowledges the support of the Royal Melbourne Hospital Neuroscience Foundation for the Warren Haynes Fellowship, as well as the Faculty of Medicine, University of Melbourne for the Leslie Eric Paddle Scholarship in Neurology. We thank Covidien (Medtronic) for provision of 30 Solitaire stentriever devices as a product research grant, K. Wilson and S. Cudennec for MRI data acquisition; C. Hall, A. Stevenson and A. Maksimenko for synchrotron acquisition; G. Sharma and S. Salinas for imaging analysis; H. Lau and T. Vale for surgical assistance; and L. Warne for anesthetic assistance. We acknowledge the facilities, and the scientific and technical assistance of the Australian National Imaging Facility at the Melbourne Brain Centre Imaging Unit, as well as the Imaging and Medical beamline at the Australian Synchrotron, Victoria, Australia.
Author information
Authors and Affiliations
Contributions
T.J.O., N.L.O., S.E.J., G.S.R., S.M.R., T.L.W., J.W.J., E.H.L., S.H.B, P.P., C.R.F., P.M.D., M.K.H., S.P., A.N.B., D.B.G., C.N.M. and T.J.O'B. designed the experiments. T.J.O., N.L.O., S.E.J., G.S.R., S.M.R., A.J.M., A.D., T.J.H.L., C.S., D.J.G., B.A.M., E.H.L., N.Y., B.C.V.C., Y.T.W., K.E.F., E.S.N., I.E.B., S.H.B., K.A.L., N.R.v.d.N., A.A., K.P.G., B.Y., L.C., L.K., A.N.B., P.J.M., D.B.G., C.N.M. and T.J.O'B. performed the experiments and analysis. T.J.O., N.L.O., S.E.J., G.S.R., S.M.R., T.L.W., L.C., S.M.D., A.N.B., P.J.M., D.B.G. and C.N.M. wrote the paper.
Corresponding author
Ethics declarations
Competing interests
T.J.O. and N.L.O. hold stock in SmartStent. Patent application US20140288667A1 filed by T.J.O. applies to the method described in the paper.
Integrated supplementary information
Supplementary Figure 1 Human cerebral vein characterization
a, Superficial venous structures were identified and reconstructed using post-contrast brain MRI images (n=50). Scale bar, 3 cm. b-c, Vein diameters were manually measured using multi-planar image reconstructions at each 5 mm fiducial point along the course of the vein. Scale bar, 5 mm. d, Pial surfaces were reconstructed and segmented for primary motor (red, Brodmann Area, BA4) and sensory (yellow, BA1) areas. Scale bar, 3 cm. e-f, The shortest distance from each venous fiducial point to the pial surface of BA4 and BA1 was measured using multi-planar reconstructions. Scale bar, 3 mm. g, 3-dimensional reconstructed venous structures and motor and sensory surfaces were superimposed to position within sulci. Scale bar, 10 mm. h, Coronal view demonstrating superior sagittal sinus. Circle of best fit within triangular measurement was recorded as diameter at each fiducial point. Scale bar, 10 mm.
Supplementary Figure 2 Human superficial cortical veins
a, Post-central sulcal vein (PostCSV, dotted line) reconstructed in relation to sensory cortex (yellow, Brodmann Area 1, BA1), with representative tributary feeding angle into superior sagittal sinus (SSS, dashed line). Scale bar, 2 cm. b, PostCSV lumen diameters at 5 mm increments, commencing proximally at SSS (median, IQR, range, n = 41). c, PostCSV distances to BA1 at 5 mm increments (median, IQR, range, n = 41). d, Central sulcal vein (CSV) route in relation to motor (red, BA4) and sensory (yellow, BA1) cortex. Scale bar, 2 cm. e, Angles of all veins entering SSS. PostCSV (mean 66.3° [95%CI 57.1 - 75.4], n = 30); CSV (mean 78.7° [95%CI 73.7 - 83.8], n = 49); PreCSV (mean 83.7° [95%CI 75.1 - 92.4], n = 25). f-h, Pre-central sulcal vein (PreCSV) diameters and distances in relation to motor cortex (red, BA4)(median, IQR, range). Scale bar, 2 cm.
Supplementary Figure 3 Human vein diameter measurement reliability
a, Overall inter-observer reliability between two observers for superficial cortical vein diameter measurements were in almost perfect agreement (ICC = 0.84; Lin’s CCC = 0.84 [95%CI 0.82 - 0.87]; reduced major axis slope = 0.97, intercept = 0.02). b, Proximal vein diameters demonstrated moderate-to-substantial agreement (ICC = 0.63; Lin’s CCC = 0.63 [95%CI 0.53 - 0.75]; reduced major axis slope = 1.09, intercept = -0.63) with identifiable proportional bias. c, Overall intra-observer repeat diameter measurements were also in almost perfect agreement (ICC = 0.89; Lin’s CCC = 0.89 [95%CI 0.88 - 0.9]; reduced major axis slope = 1.04, intercept = -0.11). d, Proximal vein region intra-observer diameters also demonstrated mildly lower values of agreement (ICC = 0.7; Lin’s CCC = 0.7 [95%CI 0.64 - 0.76]; reduced major axis slope = 1.1, intercept = -0.3), indicative of substantial agreement.
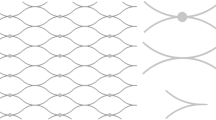
Supplementary Figure 4 Benchtop stentrode testing
a, Ovine vasculature mechanical model of major stress points along venous pathway indicating the jugular foramen (b) and the confluence of sinuses (c), scale bar, 1 cm. b, Internal catheter frictional force measured as stentrodes were deployed through catheters with varying internal diameters. Electrode detachment occurred only with attempts via 0.89 mm catheter (n = 3; all other catheter trials n = 9). c, Repeated measures (n = 3) compression test indicating superelasticity of stent is maintained with wire wrapping and attached electrodes. Average compression force comparison between d, long stentrodes with seven (n = 4) and eight (n = 4) electrodes, e, short stentrodes with six (n = 3) and seven (n = 4) electrodes and f, short and long stentrodes with seven electrodes each (n = 4).
Supplementary Figure 5 Coaxial catheter technique
a, Coaxial system including 6F sheath, 6F, 4F, 2F and microwire, all preloaded into one another. Commencing with microwire, entire system is telescoped over itself to negotiate the venous pathway toward the superior sagittal sinus (SSS). Scale bar, 5 mm. b, Plain x-ray demonstrating microwire (blue arrow) with a J shape to assist with negotiation of complex venous channels and bifurcations. 2F catheter (yellow arrow) is advanced over microwire to support entry into the SSS. Scale bar, 1 cm. c, Lateral projection digital subtraction angiography of SSS following access with 4F and prior to stentrode deployment. Scale bar, 1 cm.
Supplementary Figure 6 Identification of viable stent-mounted electrodes using electrochemical impedance spectroscopy
a, Impedance magnitude and b, phase angle of stentrode electrodes (blue) and bare metal stent (grey) immersed in saline [mean ± SD]. Dashed lines represent peak-resistance-frequency and access resistances for the stentrode electrodes (blue, 200 kHz and 816 ± 15 Ω [mean ± SD], n = 39 electrodes) and bare stent (grey, 16 kHz and 625 ± 27 Ω, n = 12 stents) immersed in saline. In saline, 10 kHz measurements are comparable with peak-resistance-frequency measured access resistance. c, Bar graph showing 10 kHz impedance of stentrode electrodes in saline (blue, 979 ± 20 Ω [mean ± SD], n = 39 electrodes), bare metal stents in saline (grey, 625 ± 27 Ω, n = 12 stents), stentrode in vivo immediately following implantation (green, 2662 ± 486 Ω, n = 28 electrodes) and stentrode in vivo with electrodes shorted to the stent (red, 659 ± 113 Ω, n = 7 electrodes). Dashed black line at 1 kΩ indicates in vivo electrode exclusion criteria for viability.
Supplementary Figure 7 Equivalent circuit model of electrode-tissue interface in comparison to saline bath and in vivo measurements
a, Simple equivalent circuit model showing solution resistance (RS), electrode-tissue interface charge transfer resistance (RE) and double-layer capacitance constant phase element (CPEE), and the tissue resistance (RT) and capacitance (CT). b, Comparison between equivalent circuit model impedance (dashed black line) and phase (dotted black line) and electrochemical impedance spectroscopy measurements [mean ± 95%CI] of average impedance (red) and phase angle (blue) of stentrodes immersed in saline (n = 39 electrodes) and in vivo at c, Day 0 (n = 28 electrodes) and d, Day 28 (n=33 electrodes). e, Change in α (black trace) and capacitive magnitude (F, blue trace) of the constant phase element as a function of implant duration, suggestive of incorporation and adherence of proteins to the electrode-tissue interface.
Supplementary Figure 8 Schematic of experimental set up
a, Endovascular stent-electrode array (stentrode) is shown implanted within the superior sagittal sinus within the brain. b, The electrode lead wire is shown to exit the brain within the internal jugular vein. c, The lead wire protrudes through the wall of the common jugular vein in the neck, and tunnels subcutaneously to (d) a custom-made hermetic connector secured to a muscle, and exiting the skin in a percutaneous micro circular plug (Omnetics, Minneapolis MN, USA). e,f, Two ground electrodes implanted subcutaneously: a large, stainless steel ground electrode implanted in the back of the sheep (e), and a platinum c-shaped ground electrode under the scalp in close proximity to the stentrode (f). Electrode lead wires and ground electrodes are connected to omnetics connectors (g) that are connected to a data acquisition system (TMSi Porti, Twente Medical Systems International, Oldenzaal, Netherlands) (h) and computer (i) to record neural information.
Supplementary Figure 9 Somatosensory evoked potential latencies
a, Histogram of all rectified peak latencies (n = 703 peaks, n = 5 animals, n= 57 [40-70] trials/session [median, interquartile range]) demonstrating occurrence of physiological peaks at 20 ms, 28 ms, 38 ms and 51 ms. b-d, Representative SSEP morphologies from individual subjects by individual electrode (b, S4; c, S2; d, S3; e, S1). Insert image displays the distribution of electrodes per subject within the superior sagittal sinus (blue circles, functional and represented electrodes). Blue dashed line represents phase reversal and dipole between peaks. Scale bar, 40 μV, 20 ms.
Supplementary Figure 10 Stentrode electrode correlation coefficients
a, Image plot of the correlation coefficients between electrodes for an example subject. Electrodes (n = 6) on the rostral end of the electrode were positively correlated with each other (yellow, > 0.5), with signals on the caudal end of the array exhibiting a phase shift reflected in the negative correlation coefficients (blue, < 0). b, Correlation coefficients of electrodes (n = 6) from an example subject (mean, SEM) showing a positive to negative change in correlation coefficient indicative of electrode location and phase shift of the acquired signal. c, Population average [mean] image plot of the correlation coefficients (n = 31 electrodes in 5 animals) showing electrodes with high correlation (yellow, >0.2) and low correlation (blue, < 0). The maximum of the color scale has been reduced to 0.45 to allow for easier comparisons, however coefficients for all electrodes against themselves (diagonal values) are 1.
Supplementary Figure 11 Validation ECoG recordings from stentrode and epidural array
Representative example demonstrating x-ray of co-implanted stentrode (yellow arrow) and epidural array (green arrow) for validation recording acute experiments. Scale bar, 5 mm.
Supplementary Figure 12 Chewing artifact comparison between recording arrays
Individual raw ECoG recordings from a, epidural (ED, orange), b, endovascular stentrode (ST, green) and c, subdural (SD, blue) electrode arrays. Red boxes indicate the identified chewing artifacts and the brown boxes indicate the baseline period. Scale bar, 50 µV, 500 ms. d, Artifact-to-baseline ratio for the epidural arrays (2.2 ± 0.1, n = 29 electrodes in 3 sheep), stentrode arrays (2 ± 0.1 [mean ± SE] n = 49 electrodes in 11 sheep) and subdural arrays (1.8 ± 0.1, n = 30 electrodes in 6 sheep). A Tukey-corrected one-way ANOVA showed that there was no statistically significant difference between the subdural, epidural, or stentrode arrays (p=0.109).
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–12 (PDF 1788 kb)
Supplemental Material
Supplementary Tables 1–6 and Supplementary Notes 1–6 (PDF 888 kb)
Rights and permissions
About this article
Cite this article
Oxley, T., Opie, N., John, S. et al. Minimally invasive endovascular stent-electrode array for high-fidelity, chronic recordings of cortical neural activity. Nat Biotechnol 34, 320–327 (2016). https://doi.org/10.1038/nbt.3428
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nbt.3428
This article is cited by
-
Haemodynamics of stent-mounted neural interfaces in tapered and deformed blood vessels
Scientific Reports (2024)
-
Boosting brain–computer interfaces with functional electrical stimulation: potential applications in people with locked-in syndrome
Journal of NeuroEngineering and Rehabilitation (2023)
-
The Fifth Bioelectronic Medicine Summit: today’s tools, tomorrow’s therapies
Bioelectronic Medicine (2023)
-
Implantable intracortical microelectrodes: reviewing the present with a focus on the future
Microsystems & Nanoengineering (2023)
-
Towards clinical application of implantable brain–computer interfaces for people with late-stage ALS: medical and ethical considerations
Journal of Neurology (2023)