Abstract
Recently, several studies have reported that dysfunctions in protein phosphatase 2A (PP2A) caused by alterations in protein phosphatase 2 regulatory subunit A, alpha (PPP2R1A) are responsible for tumorigenesis and tumor progression in several types of cancers. The impact of PPP2R1A mutations remains unknown in gastrointestinal stromal tumors (GISTs), although mutations in KIT and PDGFRA, which result in constitutive activation of the receptor tyrosine kinase pathway, are important in GIST tumorigenesis. In this study, we performed mutation analysis of PPP2R1A to examine the frequency of PPP2R1A mutations and their clinicopathological correlation in 94 GIST cases. In addition, we performed an in vitro analysis to investigate the effects of PPP2R1A mutations on cell proliferation and kinase phosphorylation in GIST cells. Seventeen GIST cases (18%) harbored mutations in PPP2R1A. All but one of these 17 cases harbored a KIT, PDGFRA, HRAS, NRAS, or KRAS mutation as the oncogenic driver mutation, and the remaining case was immunohistochemically negative for succinate dehydrogenase B (SDHB). Multivariate analysis showed that larger tumor size, higher mitotic rate, and PPP2R1A mutation are independent prognostic factors for overall survival; however, PPP2R1A mutation was not an independent prognostic factor for disease-free survival. The transduction of GIST cells with mutant PPP2R1A induced an accelerated growth rate via increased phosphorylation of Akt1/2, ERK1/2, and WNK1, a kinase associated with angiogenesis. In addition, the transduction of GIST cells with mutant PPP2R1A caused increased c-kit phosphorylation, suggesting that c-kit is also a target of PP2A, reinforcing the tumorigenic capabilities of c-kit. Furthermore, the transducing GIST cells with wild-type PP2A dephosphorylated mutant c-kit. This study provides a new insight into the biology of GISTs and their phosphatase activity, and activated PP2A could be a therapeutic target in GISTs.
Similar content being viewed by others
Main
Gastrointestinal stromal tumors (GISTs) are the most common mesenchymal tumors in the gastrointestinal tract. Approximately 85–90% of GISTs harbor oncogenic mutations in either KIT or PDGFRA, leading to the downstream activation of the RAS-RAF-MAPK and PI3K-AKT-mTOR pathways.1, 2, 3, 4, 5, 6, 7 A subset of the remaining KIT and PDGFRA mutation-negative GISTs have inactivating mutations in genes encoding subunits of succinate dehydrogenase (SDH) or activating mutations in BRAF, HRAS, NRAS, KRAS, or PIK3CA.1, 8, 9 These mutations are also expected to cause constitutive downstream activation of the KIT/PDGFRA signaling pathway.
Many cellular processes depend on the phosphorylation or dephosphorylation of signal transduction pathways. However, relatively little attention has been paid to phosphatase. Protein phosphatase 2A (PP2A), a serine/threonine phosphatase, is a tumor suppressor that plays important roles in regulating the cell cycle, survival, and differentiation.10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20 The A subunit, encoded by protein phosphatase 2, regulatory subunit A, alpha (PPP2R1A) is a scaffolding unit containing 15 HEAT repeats.21 Mutations in PPP2R1A are responsible for tumorigenesis in several types of cancer.10, 13, 15, 22, 23 In addition, irreversible phosphorylation plays an important role in the progression of ovarian and uterine carcinomas.22 PP2A dysfunction could constitutively activate various signal transduction pathways, including downstream receptor tyrosine kinase pathways. Therefore, PPP2R1A mutations might substitute for driver mutations in KIT/PDGFRA mutation-negative GISTs. Although PP2A is a serine/threonine phosphatase, PP2A activation by FTY720 causes dephosphorylation of the mutant c-kit receptor and its downstream signaling targets pAkt, pSTAT5, and pERK1/2.24 Therefore, reactivation of PP2A might be a therapeutic strategy for patients with drug-resistant c-kit mutation-positive cancers.24 However, the effects of PPP2R1A mutations in GISTs have not yet been elucidated.
In this study, we performed mutation analysis of PPP2R1A in GISTs to elucidate the frequency and clinicopathological effects of mutations in this gene. We found that PPP2R1A mutations are associated with adverse clinical outcomes for GISTs. The transduction of GIST cells with mutant PPP2R1A cells induces accelerated growth via increased phosphorylation of Akt, ERK, and WNK1. These phenotypic changes might be associated with the activation of angiogenesis. Therefore, PPP2R1A mutations could be a novel biomarker for deciding whether to use second-line tyrosine kinase inhibitors in patients with GISTs.
Materials and methods
Patients
Ninety-four cases of GISTs with prognostic information were collected from the files of the Department of Human Pathology, Juntendo University Hospital, Tokyo, Japan. All patients were treated at the Juntendo University Hospital between 2000 and 2013. These cases were diagnosed by the WHO classification system25 for soft-tissue tumors and by classification using the modified risk classification.26 In addition, diagnoses were confirmed by immunohistochemical analysis of c-kit, DOG1, and succinate dehydrogenase B (SDHB) expression. Clinicopathologic data of the 94 patients are shown in Supplementary Table 1. The follow-up period ranged from 0.3 to 164 months (mean: 65 months). The patients were treated with surgical resection without a pre-adjuvant treatment such as imatinib. In 92 of the cases, the tumors were completely resected. In the remaining two cases (cases 25 and 29), incomplete resections were performed owing to large tumor size.
Mutation Analysis of PPP2R1A, KIT, PDGFRA, HRAS, NRAS, and KRAS
Genomic DNA was extracted from each of the 94 formalin-fixed and paraffin-embedded GIST samples. Genomic DNA was also extracted from corresponding non-tumor tissue to confirm that mutations found in the tumor-derived DNA were not found in normal tissue samples. Mutation analysis of PPP2R1A was performed from exon 5 to 6 by PCR and direct sequencing. PCR cycle conditions were as follows: 94 °C for 2 min followed by 40 cycles of 94 °C for 30 s, 55 °C for 30 s, and 72 °C for 30 s, and a final hold at 72 °C for 2 min. Cases with PPP2R1A mutations were also tested for mutations in KIT (exons 9, 11, 13, and 17), PDGFRA (exons 10, 12, 14, and 18), BRAF (V600E), NRAS (exon 2 and 3), and KRAS (exons 2, 3, and 4). The primer sequences used are listed in Supplementary Table 2.
Preparation of Retrovirus and Transduction of Cell Lines
For retrovirus production, the pCX427 and pGEM (Promega) vector systems were used. A plasmid encoding human PPP2R1A (Origene) was used to generate constructs, which were subcloned into pGEM. cDNA encoding the PPP2R1A Val201Ala (PPP2R1A-T602C) and Glu238Lys (PPP2R1A-G712A) mutants was generated using the QuickChange II Site-Directed Mutagenesis kit (Agilent Technologies), and these constructs were subcloned into pCX4bleo. These two mutants were selected from the mutations detected in our GIST samples, together with the control vectors (GFP and wild-type PPP2R1A (WT)). Retroviruses were generated using αφ cells as packaging cells and were used to infect the T1 cell line (kindly provided by Dr Taguchi). GIST T1 cells had wild-type sequences in exons 5 and 6 of PPP2R1A. Infected cells were selected in 500 μg/ml Zeocin (Invitrogen). We established four GIST cell lines and named them as T1-G712A, T1-T602C, T1-GFP, and T1-WT.
Human Phospho-Kinase Array Analysis
We performed a human phospho-kinase array analysis using our four cell lines. The relative phosphorylation levels of 39 selected proteins on the array were acquired by using the Proteome Profiler Human Phospho-Kinase Array Kit (R&D Systems, Minneapolis, MN, USA) according to the manufacturer’s instructions. The expression levels of phosphorylation proteins were quantified by the Fuji Film Multi Gauge software (Tokyo, Japan).
Cell Proliferation Assay
Cells (1 × 106) from each cell line were plated in 100-mm-diameter culture dishes with 8 ml of RPMI supplemented with 10% calf serum and antibiotics (SM and PC). Cells were counted in triplicate using a TC20 Automated Cell Counter (BIO-RAD) after 24, 72, and 120 h.
Western Blotting
Proteins were extracted from our four GIST cell lines (T1-G712A, T1-T602C, T1-GFP, and T1-WT) and were separated via SDS-PAGE and transferred to nitrocellulose membranes. The membranes were incubated with one of the following antibodies: rabbit polyclonal antibodies against c-kit (dilution 1:200, Santa Cruz, sc-168), phospho-c-kit (Tyr568/570, dilution 1:200, Santa Cruz, sc-18076), phospho-c-kit (Tyr721, dilution 1:200, Santa Cruz, sc-101659), or mouse monoclonal antibody against GAPDH (dilution 1:500, Santa Cruz, sc-32233). After incubation, membranes were washed three times with Tris-EDTA buffer and then reacted with the appropriate horseradish peroxidase-conjugated secondary antibody (1:1000 dilution, GE Healthcare Biosciences).
Statistical Analysis
The χ2-test and Mann–Whitney U-test were used to examine associations between PPP2R1A mutations and clinicopathological features. The impact of PPP2R1A mutation on disease-free survival rate and overall survival rate was calculated using Kaplan–Meier analysis with the log-rank test.
Results
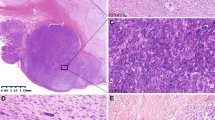
PPP2R1A Mutations
Of the 94 GIST cases, 17 (18%) harbored PPP2R1A mutations. (Table 1, Figure 1). In total, 27 PPP2R1A mutations were detected in the 17 cases, with some cases having multiple mutations in exons 5 and 6 of PPP2R1A. Besides a single point mutation, E238K, that was common between cases 10 and 15, all other PPP2R1A mutations were different between cases. In total, 26 types of mutations were detected in this study. We detected the W257STOP mutation in case 5, DNA derived from both tumor tissue and normal tissue; thus, we considered it a germline mutation or somatic mosaicism. This mutation was excluded from the following statistical analysis.
Examples of PPP2R1A mutations. The left two panels (a and c) show mutations detected in exon 5 of case #6, and the right two panels (b and d) show mutations detected in exon 6 of cases #10 and #15. These mutations were tumor-specific. (a and b) DNA derived from non-tumor tissue. (c) DNA derived from tumor tissue samples was examined and a PPP2R1A variant at codon 195 GTG>ATG (V195M) was detected. (d) DNA from tumor tissue was examined and a PPP2R1A variant at codon 238 GAG>AAG (E238K) was detected.
Mutation Analysis of KIT, PDGFRA, and KRAS
To evaluate the relationship with the driver mutations in GISTs, we examined the mutation status of KIT, PDGFRA, HRAS, NRAS, and KRAS in PPP2R1A mutation-positive tumors. Among the 17 cases with PPP2R1A mutations, 13 cases (77%) harbored KIT mutations and 2 cases (12%) harbored PDGFRA mutations in a mutually exclusive fashion. One case among the remaining two cases harbored a KRAS mutation. All KIT mutations were located in exon 11. The most common KIT mutation was a 57 base pair deletion from codons 560 to 578. Two PDGFRA mutations were located in exons 14 and 18. One of the 17 cases with mutated PPP2R1A was negative for KIT, PDGFRA, HRAS, NRAS, and KRAS mutations, although this case was negative for SDHB as determined by immunohistochemistry.
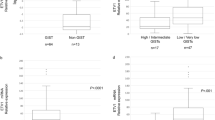
Impacts of PPP2R1A Mutations on GIST Clinicopathological Factors
We analyzed associations between PPP2R1A mutations and clinicopathological factors like age, gender, tumor site, tumor size, presence of necrosis, mitotic rates, and risk classification. We also examined the impact of recurrence and metastases on overall survival during follow-up periods. High-risk groups as determined by risk classification and higher mitotic rates had a statistically significant association with presence of a PPP2R1A mutation (mitotic rates P<0.05, risk classification P<0.05) (Table 2). Regarding the risk classification, 5 of the 45 cases (11%) in the very low- or low-risk group had a PPP2R1A mutation, none of the 14 cases (0%) in the intermediate-risk group had a PPP2R1A mutation, and 12 of the 35 cases (34%) in the high-risk group had a PPP2R1A mutation. In the very low/low-risk group, of the 5 cases harboring PPP2R1A mutations, only one was fatal. None of the remaining patients in the very low/low-risk group died. Regarding prognosis, univariate analysis revealed that patients with PPP2R1A mutations had significantly lower rates of both overall survival and disease-free survival compared to patients with wild-type PPP2R1A (Table 3: overall survival P<0.05, disease-free survival P<0.05) (Figure 2a and b). Furthermore, larger tumor size, presence of necrosis, higher mitotic rate, and higher risk classification (very low/low vs intermediate/high) were associated with shorter disease-free survival. Gastric location, larger tumor size, and higher mitotic rate were also associated with shorter overall survival. In addition, recurrence and metastasis during follow-up periods was significantly associated with shorter overall survival. Multivariate analysis showed that, larger tumor size, higher mitotic rate, and PPP2R1A mutation were independent prognostic factors for overall survival (Table 3). However, only larger tumor size and higher mitotic rate were independent prognostic factors for disease-free survival. Furthermore, regarding the 17 patients with PPP2R1A mutations, 6 of these patients received post-operative imatinib. Among these six patients, three died of disease, two have remained disease-free, and one is alive with recurrent disease. There was no difference in prognosis according to the post-operative imatinib status in patients with PPP2R1A mutation. In addition, there was no difference in prognosis in this series of cases according to post-operative imatinib status (data not shown).
Human Phospho-Kinase Array Analysis
To identify activated cellular signaling pathways associated with PPP2R1A mutations in GISTs, we performed a human phospho-kinase array analysis of 46 specific Ser/Thr or Tyr phosphorylation sites on 39 selected proteins, using T1-G712A, T1-T602C, T1-GFP, and T1-WT cell lines. The expression levels of the phosphorylated proteins in each GIST cell line transduced with a PPP2R1A mutation were compared with the protein expression levels in cells transduced with GFP to identify proteins with altered phosphorylation (Figure 3a).
(a) Human phospho-kinase array analysis. Levels of phospho-kinases were assessed using a horseradish peroxidase-conjugated phospho-kinase antibody, which was followed by chemiluminescence detection. In T1-WT cells, the levels of phosphorylated Akt1/2/3, ERK1/2, and WNK1 were significantly reduced. Both T1-T602C and T1-G712A cells had significantly higher levels of phosphorylated Akt1/2/3 and WNK1. The level of phosphorylated ERK1/2 increased in T1-G712A cells and decreased in T1-T602C cells. *P<0.05 compared with cells expressing PPP2R1A-WT. (b) Evaluation of in vitro cell growth. For each experiment, 1.0 × 106 cells were cultured in RPMI and counted at 24, 72, and 120 h. *P<0.05 compared with cells expressing GFP; NS, not significant compared with cells expressing GFP.
In T1-WT cells, the levels of phosphorylated Akt1/2/3, ERK1/2, and WNK1 were significantly reduced compared with those in the control as follows: Akt1/2/3 (0.66±0.02), ERK1/2 (0.56±0.02), and WNK1 (0.80±0.00). Both T1-T602C and T1-G712A cells had significantly higher Akt1/2/3 phosphorylation levels (PPP2R1A-T602C: 1.41±0.01, PPP2R1A-G712A: 1.22±0.03) and WNK1 phosphorylation levels (PPP2R1A-T602C: 1.32±0.00, PPP2R1A-G712A: 1.38±0.00). The level of phosphorylated ERK1/2 increased in T1-G712A cells (1.18±0.03) and decreased in T1-T602C cells (0.81±0.01).
Cell Proliferation Assay
To elucidate the impact of PPP2R1A mutations on the behavior of GISTs, we conducted a cell proliferation assay using T1-G712A, T1-T602C, T1-GFP, and T1-WT cell lines. Both T1 lines containing PPP2R1A mutations (T1-G712A and T1-T602C) had significantly higher growth rates compared with growth rates of T1-GFP and T1-WT cells (Figure 3b). There was no difference in proliferation rate between T1-GFP and T1-WT cells.
Western Blotting
The c-kit phosphorylation status in T1 cells expressing PPP2R1A mutations (T1-G712A and T1-T602C) was also evaluated. In T1 cells transduced with these PPP2R1A mutations, phosphorylation at Tyr721 of c-kit was increased compared with those transduced with wild-type PPP2R1A or GFP (Figure 4). The same phenomenon was observed regarding phosphorylation of Tyr568/570; however, this trend was not as strong as the trend for Tyr721 (Figure 4). This is probably due to the position of the KIT mutation in T1 cells having KIT del570–578. On the other hand, in wild-type transduced cells, phosphorylation was decreased compared with T1-GFP (Figure 4). These findings suggested that wild-type PP2A could dephosphorylate mutant c-kit in GIST.
c-kit phosphorylation status according to the transduction of mutant PPP2R1A in T1 cells. In T1 cells transduced with mutant PPP2R1A, phosphorylation at Tyr721 was increased compared with those transduced with wild-type PPP2R1A or GFP. The same phenomenon was observed regarding phosphorylation of Tyr568/570, however, this trend was weaker than Tyr721. On the other hand, in wild-type-transduced cells, phosphorylation was decreased compared with T1-GFP.
Discussion
Mutations in PPP2R1A have been reported in many cancers such as lung cancer, melanoma, and breast cancer,10 and are important in the pathogenesis of some uterine15, 22, 23 and ovarian cancers.13, 22, 23 In addition, reduced expression of subunit A of PP2A, which is encoded by PPP2R1A, has been reported in glioma.14 In this study, we detected PPP2R1A mutations in 18% of GISTs, which is relatively higher rate than is seen in other cancers.10, 13, 15, 22, 23 All PPP2R1A mutations except one were missense mutations and were heterozygous, consistent with previous findings.10, 22 Previously reported somatic PPP2R1A mutations are located in both HEAT5 and HEAT7 motifs near the interface of subunits A and B.22, 23 Most reported PPP2R1A missense mutations occur in recurrent hotspots.22, 23 However, most PPP2R1A mutations that we detected were not recurrent, although all were located in HEAT5 to HEAT7. The in vitro assay performed using a GIST cell line transduced with either of two PPP2R1A mutants selected from the mutations detected in this study showed drastic phenotypic changes. Thus, PPP2R1A mutations detected in this study are expected to reduce the enzymatic activity of PP2A.
Next, we asked whether mutations in PPP2R1A could be a driver oncogene in KIT/PDGFRA mutation-negative GISTs. Of the ~20% of GIST cases for which we detected PPP2R1A mutations, we also examined the mutation status of KIT, PDGFRA, BRAF, HRAS, NRAS, and KRAS. The frequencies of these mutations within GISTs with PPP2R1A mutations are consistent with previously reported values.1 These findings suggest that mutations in PPP2R1A and reported driver genes including KIT and PDGFRA are not mutually exclusive. Therefore, mutations in PPP2R1A are not another driver mutation of GISTs.
The prognostic impact of PPP2R1A mutations in malignant tumors has not been investigated, despite many reports describing the frequency of these mutations in various tumor types. PPP2R1A mutations might be one of many molecular genetic alterations that contribute to tumor progression in undifferentiated uterine and ovarian low-grade endometrioid carcinomas.28 Mutations in PPP2R1A can affect the binding of other subunits or substrate recognition and constitutively disrupt PP2A function.12, 29 Thus, PPP2R1A mutations could cause constitutive activation of various signal transduction pathways, including the receptor tyrosine kinase pathway.
In this study, the presence of PPP2R1A mutations was associated with higher risk classification and higher mitotic rate (>5/50 HPFs). Among the 17 GIST cases with PPP2R1A mutations, 5 cases were classified as very low or low risk. One of these five patients died despite the low-risk classification. Furthermore, PPP2R1A mutations were determined to be adverse prognostic factors for disease-free survival and overall survival by univariate analysis. PPP2R1A mutations, larger tumor size, and higher mitotic rate were independent prognostic factors for overall survival, as determined by multivariate analysis. In vitro analysis also supported these findings. Human phospho-kinase array analysis revealed that phosphorylation of Akt and ERK significantly increased in mutant PPP2R1A-transduced cell lines compared to the WT PPP2R1A-transduced cell line. PP2A is involved in signaling pathways, including Akt and ERK, as a dephosphorylation enzyme.10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20 These findings confirm that mutations in PPP2R1A disrupt PP2A function, leading to elevated phosphorylation of its substrates. In addition, the proliferation of mutation-expressing T1 cell lines was significantly accelerated compared with control cell lines. PP2A is a tumor suppressor and has an important role in regulating cell cycle progression, survival, and differentiation.10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20 Together with these findings, GISTs with loss of PP2A function would likely acquire a more aggressive phenotype, and PPP2R1A mutations could act in a dominant negative manner in GISTs. Alternatively, biallelic inactivation might be necessary for the functional reduction or loss of PP2A, because 7 out 17 cases with PPP2R1A mutations harbored multiple mutations. In addition, the acquisition of a more aggressive GIST phenotype upon PPP2R1A mutation could be attributed to the enhanced phosphorylation of mutant c-kit.
Angiogenesis is also essential for GIST growth, invasion, and metastasis.30, 31, 32 Among the phosphorylated proteins analyzed in our phosphorylation array, phosphorylation of WNK1, which is involved in regulating ion transport systems in the distal nephron,33 was significantly elevated. Recently WNK has been considered a causative gene of pseudohypoaldosteronism type II.33 In addition, WNK1 is involved in angiogenesis in gliomas34 and in in vivo examination of zebrafish.35, 36, 37
Emergence of a tyrosine kinase inhibitor that targets phosphorylated receptor tyrosine kinases would drastically improve the prognosis of GIST patients. However, advanced GISTs may acquire secondary resistance or even have primary resistance to tyrosine kinase inhibitors.38 Interestingly, our phospho-kinase array revealed that phosphorylation of Akt1/3, downstream kinases of vascular endothelial growth factor (VEGF) signaling, and WNK1, involved in angiogenesis, was increased in mutant PPP2R1A expressing GIST cells. These findings suggest that VEGF signaling could be activated in a ligand-independent manner and be involved in tumor progression in GIST cells with PPP2R1A mutation. VEGF signaling is a therapeutic target of sunitinib, which is currently used as a second-line therapy for patients with imatinib-resistant GISTs. Furthermore, increased microvessel density and angiogenesis by VEGF signaling affects GIST patients prognosis.32 Our findings suggest that as tyrosine kinase inhibitors targeting the VEGF signaling pathway, such as sunitinib, might be less effective for GISTs with PPP2R1A mutations, PPP2R1A mutations could be potential biomarkers and indicators for the application of second-line tyrosine kinase inhibitors.
Finally, drugs that directly activate PP2A do not exist. However, drugs that remove endogenous PP2A inhibitors, such as SET and CIP2A, already exist.39, 40, 41, 42 These drugs could be used for advanced GISTs with primary or secondary resistance to tyrosine kinase inhibitors as an adjuvant therapy.
In conclusion, PPP2R1A mutations occur in a subset of GISTs and are associated with a high malignant potential that leads to decreased disease-free survival and overall survival. The functional disorders of PP2A caused by PPP2R1A mutations promote phosphorylation of specific kinases, including those involved in angiogenesis, leading to the activation of signaling pathways that involve PP2A.
References
Yamamoto H, Oda Y . Gastrointestinal stromal tumor: recent advances in pathology and genetics. Pathol Int 2015;65:9–18.
Lasota J, Miettinen M . KIT and PDGFRA mutations in gastrointestinal stromal tumors (GISTs). Semin Diagn Pathol 2006;23:91–102.
Corless CL . Gastrointestinal stromal tumors: what do we know now? Mod Pathol 2014;27 Suppl 1:S1–S16.
Doyle LA, Hornick JL . Gastrointestinal stromal tumours: from KIT to succinate dehydrogenase. Histopathology 2014;64:53–67.
Miettinen M, Wang ZF, Sarlomo-Rikala M et al. Succinate dehydrogenase-deficient GISTs: a clinicopathologic, immunohistochemical, and molecular genetic study of 66 gastric GISTs with predilection to young age. Am J Surg Pathol 2011;35:1712–1721.
Gill AJ . Succinate dehydrogenase (SDH) and mitochondrial driven neoplasia. Pathology 2012;44:285–292.
Janeway KA, Kim SY, Lodish M et al. Defects in succinate dehydrogenase in gastrointestinal stromal tumors lacking KIT and PDGFRA mutations. Proc Natl Acad Sci USA 2011;108:314–318.
Daniels M, Lurkin I, Pauli R et al. Spectrum of KIT/PDGFRA/BRAF mutations and Phosphatidylinositol-3-Kinase pathway gene alterations in gastrointestinal stromal tumors (GIST). Cancer Lett 2011;312:43–54.
Miranda C, Nucifora M, Molinari F et al. KRAS and BRAF mutations predict primary resistance to imatinib in gastrointestinal stromal tumors. Clin Cancer Res 2012;18:1769–1776.
Calin GA, di Iasio MG, Caprini E et al. Low frequency of alterations of the alpha (PPP2R1A) and beta (PPP2R1B) isoforms of the subunit A of the serine-threonine phosphatase 2A in human neoplasms. Oncogene 2000;19:1191–1195.
Wang SS, Esplin ED, Li JL et al. Alterations of the PPP2R1B gene in human lung and colon cancer. Science 1998;282:284–287.
Ruediger R, Pham HT, Walter G . Disruption of protein phosphatase 2A subunit interaction in human cancers with mutations in the A alpha subunit gene. Oncogene 2001;20:10–15.
Jones S, Wang TL, Shih Ie M et al. Frequent mutations of chromatin remodeling gene ARID1A in ovarian clear cell carcinoma. Science 2010;330:228–231.
Colella S, Ohgaki H, Ruediger R et al. Reduced expression of the Aalpha subunit of protein phosphatase 2A in human gliomas in the absence of mutations in the Aalpha and Abeta subunit genes. Int J Cancer 2001;93:798–804.
Nagendra DC, Burke J 3rd, Maxwell GL et al. PPP2R1A mutations are common in the serous type of endometrial cancer. Mol Carcinog 2012;51:826–831.
Silverstein AM, Barrow CA, Davis AJ et al. Actions of PP2A on the MAP kinase pathway and apoptosis are mediated by distinct regulatory subunits. Proc Natl Acad Sci USA 2002;99:4221–4226.
Epie N, Ammosova T, Turner W et al. Inhibition of PP2A by LIS1 increases HIV-1 gene expression. Retrovirology 2006;3:65.
Guenin S, Schwartz L, Morvan D et al. PP2A activity is controlled by methylation and regulates oncoprotein expression in melanoma cells: a mechanism; which participates in growth inhibition induced by chloroethylnitrosourea treatment. Int J Oncol 2008;32:49–57.
Kolupaeva V, Laplantine E, Basilico C . PP2A-mediated dephosphorylation of p107 plays a critical role in chondrocyte cell cycle arrest by FGF. PLoS One 2008;3:e3447.
Lu J, Kovach JS, Johnson F et al. Inhibition of serine/threonine phosphatase PP2A enhances cancer chemotherapy by blocking DNA damage induced defense mechanisms. Proc Natl Acad Sci USA 2009;106:11697–11702.
Cho US, Xu W . Crystal structure of a protein phosphatase 2A heterotrimeric holoenzyme. Nature 2007;445:53–57.
Shih IeM, Panuganti PK, Kuo KT et al. Somatic mutations of PPP2R1A in ovarian and uterine carcinomas. Am J Pathol 2011;178:1442–1447.
McConechy MK, Anglesio MS, Kalloger SE et al. Subtype-specific mutation of PPP2R1A in endometrial and ovarian carcinomas. J Pathol 2011;223:567–573.
Roberts KG, Smith AM, McDougall F et al. Essential requirement for PP2A inhibition by the oncogenic receptor c-KIT suggests PP2A reactivation as a strategy to treat c-KIT+ cancers. Cancer Res 2010;70:5438–5447.
Fletcher CDM, Bridge JA, Hogendoorn PCW et al WHO Classification of Soft Tissue and Bone, 4th edn. 2013, pp 164–167.
Joensuu H . Risk stratification of patients diagnosed with gastrointestinal stromal tumor. Human Pathol 2008;39:1411–1419.
Akagi T, Sasai K, Hanafusa H . Refractory nature of normal human diploid fibroblasts with respect to oncogene-mediated transformation. Proc Natl Acad Sci USA 2003;100:13567–13572.
Kuhn E, Ayhan A, Bahadirli-Talbott A et al. Molecular characterization of undifferentiated carcinoma associated with endometrioid carcinoma. Am J Surg Pathol 2014;38:660–665.
Ruediger R, Hentz M, Fait J et al. Molecular model of the A subunit of protein phosphatase 2A: interaction with other subunits and tumor antigens. J Virol 1994;68:123–129.
Chen WT, Huang CJ, Wu MT et al. Hypoxia-inducible factor-1alpha is associated with risk of aggressive behavior and tumor angiogenesis in gastrointestinal stromal tumor. Jpn J Clin Oncol 2005;35:207–213.
Nakayama T, Cho YC, Mine Y et al. Expression of vascular endothelial growth factor and its receptors VEGFR-1 and 2 in gastrointestinal stromal tumors, leiomyomas and schwannomas. World J Gastroenterol 2006;12:6182–6187.
Imamura M, Yamamoto H, Nakamura N et al. Prognostic significance of angiogenesis in gastrointestinal stromal tumor. Mod Pathol 2007;20:529–537.
Arroyo JP, Gamba G . Advances in WNK signaling of salt and potassium metabolism: clinical implications. Am J Nephrol 2012;35:379–386.
Zhu W, Begum G, Pointer K et al. WNK1-OSR1 kinase-mediated phospho-activation of Na+-K+-2Cl- cotransporter facilitates glioma migration. Mol Cancer 2014;13:31.
Lai JG, Tsai SM, Tu HC et al. Zebrafish WNK lysine deficient protein kinase 1 (wnk1) affects angiogenesis associated with VEGF signaling. PLoS One 2014;9:e106129.
Xie J, Yoon J, Yang SS et al. WNK1 protein kinase regulates embryonic cardiovascular development through the OSR1 signaling cascade. J Biol Chem 2013;288:8566–8574.
Xie J, Wu T, Xu K et al. Endothelial-specific expression of WNK1 kinase is essential for angiogenesis and heart development in mice. Am J Pathol 2009;175:1315–1327.
Benjamin RS, Debiec-Rychter M, Le Cesne A et al. Gastrointestinal stromal tumors II: medical oncology and tumor response assessment. Semin Oncol 2009;36:302–311.
Oaks JJ, Santhanam R, Walker CJ et al. Antagonistic activities of the immunomodulator and PP2A-activating drug FTY720 (Fingolimod, Gilenya) in Jak2-driven hematologic malignancies. Blood 2013;122:1923–1934.
Chen KF, Liu CY, Lin YC et al. CIP2A mediates effects of bortezomib on phospho-Akt and apoptosis in hepatocellular carcinoma cells. Oncogene 2010;29:6257–6266.
Liu CY, Shiau CW, Kuo HY et al. Cancerous inhibitor of protein phosphatase 2A determines bortezomib-induced apoptosis in leukemia cells. Haematologica 2013;98:729–738.
Ding Y, Wang Y, Ju S et al. Role of CIP2A in the antitumor effect of bortezomib in colon cancer. Mol Med Rep 2014;10:387–392.
Acknowledgements
This work was supported in part by a Grant-in-Aid for General Scientific Research from the Ministry of Education, Science, Sports, and Culture (#26670286 to Tsuyoshi Saito and #15H04964 to Yoshiyuki Suehara), Tokyo, Japan.
Author contributions
TS, KM, and TY diagnosed and histologically evaluated GIST samples. MT-I, KA, and TO performed DNA extraction and sequencing analysis. MT-I, KM, DK, and SK performed in vitro experiments. MT-I, KA, KM, and TS contributed to data analysis. MT-I, YS, TT, KK, TY, and TS wrote the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Modern Pathology website
Supplementary information
Rights and permissions
About this article
Cite this article
Toda-Ishii, M., Akaike, K., Suehara, Y. et al. Clinicopathological effects of protein phosphatase 2, regulatory subunit A, alpha mutations in gastrointestinal stromal tumors. Mod Pathol 29, 1424–1432 (2016). https://doi.org/10.1038/modpathol.2016.138
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2016.138