Abstract
The abundance of tumor-infiltrating lymphocytes has been associated with a favorable prognosis in estrogen receptor-negative breast cancer. However, a high degree of spatial heterogeneity in lymphocytic infiltration is often observed and its clinical implication remains unclear. Here we combine automated histological image processing with methods of spatial statistics used in ecological data analysis to quantify spatial heterogeneity in the distribution patterns of tumor-infiltrating lymphocytes. Hematoxylin and eosin-stained sections from two cohorts of estrogen receptor-negative breast cancer patients (discovery: n=120; validation: n=125) were processed with our automated cell classification algorithm to identify the location of lymphocytes and cancer cells. Subsequently, hotspot analysis (Getis–Ord Gi*) was applied to identify statistically significant hotspots of cancer and immune cells, defined as tumor regions with a significantly high number of cancer cells or immune cells, respectively. We found that the amount of co-localized cancer and immune hotspots weighted by tumor area, rather than number of cancer or immune hotspots, correlates with a better prognosis in estrogen receptor-negative breast cancer in univariate and multivariate analysis. Moreover, co-localization of cancer and immune hotspots further stratified patients with immune cell-rich tumors. Our study demonstrates the importance of quantifying not only the abundance of lymphocytes but also their spatial variation in the tumor specimen for which methods from other disciplines such as spatial statistics can be successfully applied.
Similar content being viewed by others
Main
Estrogen receptor (ER) status is one of the most important clinical parameters in breast cancer, with ER-negative patients generally having a poorer 10-year prognosis than ER-positive patients.1, 2, 3, 4 However, the considerable variation in clinical outcome of ER-negative patients has fuelled the quest for additional markers to better stratify this disease subset and eventually provide more effective personalized treatment.5 Tumor infiltration by various cells of the immune system has been associated with a favorable clinical outcome in ER-negative breast cancer.6 Methods to assess tumoral immune infiltration include traditional pathological examination and gene expression profiling.7, 8 Although the latter can indicate the immune cell type and their relative abundance, a more comprehensive analysis of their number, lineage and spatial distribution requires pathological assessment.9, 10, 11, 12
Spatial information on the tumor immune microenvironment is of clinical relevance, as not only the abundance and type but also the spatial locations of immune cells have been shown to be associated with clinical outcome in colorectal13 and breast cancer.10, 11, 14 In the former, a high density of CD3+ T-lymphocytes at the invasive margin was found to be significantly associated with disease-free survival in three independent cohorts of patients, whereas in breast tumors the total and distant stromal counts of CD8+ cytotoxic T-cells were independently capable of predicting breast cancer-specific survival.14 More recently, in ER-negative/HER2-negative10 and HER2-negative11 breast cancer patients, a high degree of stromal immune infiltration was found to be associated with increased disease-specific survival and pathological complete response rates, respectively.
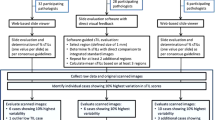
Although the intra-specimen location of lymphocytes is often accounted for on an individual basis during evaluation of immune infiltration,9, 10, 15 there has been no systematic investigation in larger cohorts of their spatial relation to one another and the degree of uniformity or clustering in the pattern of their distribution (Figure 1a). Given the occasionally marked spatial heterogeneity of immune cell distribution in breast cancer, we aimed to: (i) develop a robust methodology to elucidate the spatial heterogeneity of cancer and immune cells and their spatial relationship, and (ii) investigate whether this spatial heterogeneity is of clinical significance in ER-negative breast cancer patients.
Spatial heterogeneity in lymphocytic infiltration and the use of Getis–Ord hotspot analysis. (a) 3D landscape of lymphocyte and cancer cell density within a H&E-stained tumor section showing spatial heterogeneity in the pattern of lymphocytic infiltration. (b) Illustration of the concept of Getis–Ord hotspot analysis, which detects statistically significant cancer and immune hotspots tested for every square tumor region. An example tumor section with a grid overlay to divide the image into squares (top-left, not drawn to scale), exclusion of empty (grey) squares (top-right), construction of neighborhood for one grid square (bottom-right, first order consists of squares in yellow, second order includes also the green squares and fourth order includes yellow, green and blue squares) and detection of hotspots (bottom-left) are displayed as an example.
To achieve these aims, we developed a computational approach combining high-throughput pathological image analysis with spatial statistics. Objective assessment of a large number of pathological samples requires the use of automated methods to identify cells in their thousands. The emerging field of computational pathology utilizes the advanced processing capabilities of modern-day computers to aid in the pathological assessment of tissue samples by reducing subjectivity and improving reproducibility. Fully automated cell, vessel and tumor region classification algorithms have been published that use features such as object size and morphology to classify them with high accuracy.15, 16, 17, 18, 19, 20, 21, 22, 23 We have previously carried out a fully automated, quantitative assessment of immune infiltration in ER-negative breast cancer to report that a greater abundance of lymphocytes ascertained by image analysis is associated with a better prognosis.12
To understand the complexity in the resulting large amount of spatial data following image analysis, we can employ methods from other disciplines such as ecology, where the spatial interactions among species are routinely studied. Geographically mapped regions populated by different species correspond to the two-dimensional representation of tumor architecture in histological sections, infiltrated by different cell types. One method widely used on ecological and demographical data to analyze spatial interactions is the Getis–Ord hotspot analysis,24 which pinpoints the location of regions where there is a statistically significant spatial clustering of high magnitudes of a variable, independent of the number of observations. For example, de Souza et al25 used Getis–Ord hotspot analysis to identify zones of significantly high prevalence of malaria-carrying mosquitoes in Ghana. Setiadi et al26 carried out spatial analysis using the L-function statistic to study clustering differences in T- and B-lymphocytes in healthy and tumor draining lymph nodes, but we are thus far unaware of the use of such methods in a large-scale investigation that relates to clinical outcome.
Therefore, this paper is based on two key concepts: (i) the use of high-throughput image analysis to generate spatial data denoting locations of cancer and immune cells within tumors, and (ii) the introduction of spatial statistics to detect and quantify cancer/immune spatial clusters or hotspots, ie, spatial regions where the population of cancer cells or lymphocytes is significantly high.
Materials and methods
Sample Set
To investigate the clinical implications of immune hotspots, we chose a sample of 245 ER-negative breast cancer patients from the METABRIC consortium.27 METABRIC is a large-scale investigation of breast cancer heterogeneity, for which 1026 pretreatment primary breast tumors with hematoxylin and eosin (H&E)-stained frozen tumor sections, molecular profiles and 10-year disease-specific survival data are available for further analysis. The tumor sections were scanned using ScanScope TX Scanner from Aperio Technologies with × 20 magnification and digitized for image analysis as described in Yuan et al.12 We have previously reported the association between lymphocyte abundance (lym, calculated as the percentage of immune cells in the total sample cell count) and a good prognosis in 115 ER-negative breast cancers in METABRIC.12 For this study, we expanded our sample size to 245 ER-negative breast cancer patients for a larger investigation. The data were collected independently at three hospitals: A (120 patients), B (62 patients) and C (63 patients). We chose patients from A as our discovery cohort and patients from B and C collectively as our validation cohort, in order to have a similar population size in each set.
Pathological Image Analysis for Cell Classification
H&E-stained frozen tumor section images for 245 ER-negative breast cancer patients were analyzed using our automated cell classification pipeline CRImage.12 This tool first segmented cell nuclei and then analyzed morphological features, such as size and circularity, of each cell nucleus detected in the image. These quantitative features were input into a support vector machine for supervised classification into cancer, lymphocyte and stromal cell nuclei. Lymphocytes have a typical morphology of small, round and homogeneously basophilic nuclei, thus can be reliably differentiated from other cell types in breast cancer. The accuracy of classification was evaluated by cross-validation in the initial training set of 871 cells (90.1% accuracy), in comparison to pathological tumor scores, including tumor cellularity and lymphocytic infiltration, and gene expression data.12 In addition, visual scoring of 10 000 cells by a pathologist was compared with automated classification, and they were found to be highly correlated (R2=0.98). As a result of image analysis, we identified, on average, 77 200 cancer cells (s.d. 75 400) and 14 000 lymphocytes (s.d. 22 300) as well as their spatial locations in each tumor in our sample set.
Getis–Ord Spatial Statistics for Hotspot Identification
The cell classification and location data were used as input for Getis–Ord hotspot analysis to enable the automated detection of statistically significant spatial clusters. Hotspot mapping is carried out on spatial data to identify locations where a variable of interest is found to be clustered. This means that, in relation to the entire area of study, the frequency or magnitude of this variable at these locations is greater than expected and, importantly, that the difference between the actual and expected value (determined from the area mean) is statistically significant. Tumor section images contain areas devoid of tissue, which were excluded from our analysis using a binary tissue mask constructed by CRImage that classifies each pixel as tissue or non-tissue. Pixels corresponding to each region in the tumor were then summed up to determine the extent of tissue cover. Regions with <50% tissue cover were excluded from hotspot analysis. From the remaining regions, we also excluded those that contained no cancer cells, as our primary interest was to study tumor regions in close proximity to cancer.
To perform Getis–Ord hotspot analysis on pathological samples, a grid of square size s and neighborhood size NR needed to be determined, as input data are required in the form of spatial points with associated values and neighbors. In our exploratory analysis, three region and three neighborhood sizes were chosen for comparison. The region size s was defined as the side length of grid squares, with s=50, 100 or 250 μm. The neighborhood sizes NR were first, second and fourth order, where first order refers to the region being analyzed and the regions that share an edge or vertex with it, second order refers to first-order neighbors and regions that share an edge or vertex with first-order neighbors and so on. Figure 1b illustrates application of the grid and the different neighborhood arrangements. The combination of three region sizes and three neighborhood sizes were tested on the discovery cohort samples, with the exception that for s=250 μm only NR=first order was considered, as we wanted to keep the neighborhood radius in all cases to be no more than twice the cell–cell communication distance (250 μm) proposed by Francis et al.28
These parameter combinations allowed us to investigate clustering of a variable across small, medium and large spatial configurations in order to determine the extent to which they affect any potential correlation that hotspots may have with clinical outcome of the patient. The z score for every region i is computed as,

where S and U are two normalizing factors, given by:


where n is the total number of grid regions (excluding those with <50% tissue cover or no cancer cells); cj is the cancer or lymphocyte count for region j; C̄ is the mean value of c for all regions in the image and wi,j is element (i,j) of the matrix of weights, w, which indicates the influence of two regions on each other and is used to check whether or not the two regions are neighbors:

The P-value corresponding to each evaluated z score is determined using the thresholds specified in Getis and Ord.24 For each region i, we evaluated its potential as a hotspot of cancer or immune cells, ie, a region with statistically significant clustering of these cells, as determined by its associated pi <0.05. Distributions of cancer, immune and co-localized cancer–immune hotspots for an example tumor specimen are given in Figure 2.
Mapping cancer and lymphocyte hotspots. (a) A H&E-stained tumor sample consisting of three sections. (b) Image analysis result, classifying nuclei in the image into cancer and lymphocyte and displaying their distribution in the sample. (c) Cancer and (d) immune (lymphocyte) hotspot detection using Getis–Ord hotspot analysis. (e) Co-localized cancer and immune hotspots, ie, regions classified as both cancer and immune hotspots.
Parameter Selection and Validation
After applying hotspot analysis to our discovery cohort, we processed the results to select optimum values of the two spatial parameters, s and NR, and a threshold from one of our three proposed hotspot measures, fC, fI and fC–I, that best differentiated between good and poor clinical outcome (see Results section). This was achieved by recursively selecting every ten-thousandth value of each of our hotspot measures in the 15–85% quantiles to dichotomize these parameters in univariate survival analysis using the available 10-year disease-specific survival data. Following this, we constructed a multivariate Cox proportional hazards model for each of the cohorts, using the known clinical predictors node metastasis, tumor size and lym. Tumor grade was not found to be significant for survival in univariate analysis in the discovery (P=0.196) or validation (P=0.852) cohort and was therefore excluded in multivariate analysis.
Other Statistical Methods
Statistical tests were carried out in R. Survival curves were fitted using the Kaplan–Meier method, and univariate and multivariate analyses were performed using Cox proportional hazards models,29 with P-values obtained from the Wald test. Associations between continuous variables were tested by evaluation of Pearson’s correlation coefficient and between discrete and continuous variables using the Jonckheere–Terpstra (JT) trend test.30 Student’s t-test was used to determine if two group means are significantly different. In all cases, a P-value of <0.05 was taken to be a significant result.
Results
Statistical Assessment of Cancer and Immune Hotspots in Primary ER-Negative Breast Tumors
To identify cancer cells and lymphocytes in breast whole-tumor sections, the H&E-stained images were first analyzed with our previously validated image analysis pipeline12 for automated classification and detection of the spatial location of each cell nucleus (see Materials and methods section, Figures 2a and b). Subsequently, Getis–Ord spatial analysis was carried out to identify the precise location of the statistically significant clusters of cancer cells, ie, cancer hotspots, given a set of predefined parameters for spatial configuration (see Materials and methods section, Figure 2c). Specifically, Getis–Ord analysis computes a z-score for each region, which is a measure of the difference between observations in that region and the overall area being studied. Each z-score has an associated P-value, which can be used to determine statistical significance. Similarly, clusters or hotspots of lymphocytes in the same samples were identified (Figure 2d). To generate the summary statistics of spatial heterogeneity of immune infiltration for each tumor, we proposed three scores:
-
1
Cancer hotspot fractional: the fraction of cancer hotspots that are also immune hotspots (fC);
-
2
Immune hotspot fractional: the fraction of immune hotspots that are also cancer hotspots (fI); and
-
3
Cancer–immune hotspot co-localization: the fractional area of tumor where cancer and immune hotspots were co-localized (fC–I).
The rationale for choosing these measurements is to investigate how cancer and immune hotspots are spatially related to each other, as it is only meaningful to study immune cells within the spatial context of cancer cells, and how the scores should be normalized, ie, by the number of cancer cell clusters in the sample (fC), the number of immune cell clusters in the sample (fI) or the total area of tumor analyze d for hotspot detection (fC–I).
Histopathological review of representative scans yielding the highest co-localized hotspot scores confirmed the presence of a mixed population of mononuclear cells in close proximity to invasive tumor cells within the areas outlined by the program, as shown in an example in Figure 3.
Representative examples of co-localized hotspots. (a) A low-resolution image to show locations of cancer (red) and immune (blue) hotspots. (b) High-resolution images to show two examples of co-localized hotspots (outlined in green) in the corresponding regions of panel (a). (c) Example of an immune hotspot (left) and a cancer hotspot (right).
Co-localization of Cancer and Immune Hotspots Is an Independent Prognostic Marker
To test the association between hotspot analysis results and prognosis in ER-negative breast cancer, we carried out univariate survival analysis in our discovery cohort for each of the seven spatial configuration results sets (see Materials and methods section), using Cox regression with a single predictor: fC, fI or fC–I (Table 1). Three of the seven spatial configurations tested gave a significant result in differentiating between good and poor disease-specific survival rate, for one or more of the three predictors tested. The most significant result was obtained for a spatial configuration of s=50 μm and NR=fourth order, which, using a threshold in fC–I of 1.91% for dichotomization, was able to differentiate between good and poor clinical outcome (P=0.009, hazard ratio (HR)=3.204, 95% confidence interval=1.343–7.646, Figure 4a). This was further confirmed in the validation cohort (P=0.017, HR=2.207, HR 95% confidence interval=1.138–3.747, Table 2,Figure 4a). Thus, best results can be obtained using a spatial configuration of small regions (s=50 μm) and a large neighborhood (NR=fourth order, see Materials and methods section), suggesting that the analysis benefits from abundant data points with large neighborhood coverage. Taken together, we found that fC–I, the fractional tumor area where cancer and immune hotspots co-localized (co-localized hotspot score), is significantly associated with good disease-specific survival in ER-negative breast cancer.
Prognostic value of the co-localized hotspot score. (a) Kaplan–Meier curves displaying disease-specific survival rates over 10 years in the discovery and validation cohorts. Patients in both cohorts are stratified by the co-localized hotspot score using a selected threshold of 1.91%. The numbers and the numbers in brackets (bottom-right) indicate the numbers of patients and the numbers of breast cancer-specific deaths in each group, respectively. (b) Plots illustrating how the cancer–immune hotspot measure (y axis) relates to six factors known to be associated with clinical outcome in breast cancer, in both the discovery (left) and validation (right) cohorts. Jonckheere–Terpstra trend test P-value is given for lymph node metastasis, tumor size and HER2 expression and Pearson’s correlation coefficient r and its P-value are given for lymphocytic abundance (lym), tumor section area and patient age, at the top-right of each plot.
We proceeded to test our proposed co-localized hotspot measure in multivariate analysis with the clinical variables node metastasis, tumor size and lym to assess its potential as an independent prognostic indicator for ER-negative breast cancer. Tumor grade was found to be statistically insignificant for both cohorts in univariate analysis, hence it was excluded from the multivariate model. We constructed a Cox proportional hazards model and found that all three of the clinical variables as well as co-localized hotspots (P=0.019, HR=2.910, HR 95% confidence interval=1.189–7.118) could predict survival independently in our discovery cohort (Table 2). In our validation cohort, node metastasis and lym as a continuous variable failed to predict survival independently; however, our proposed hotspot index (P=0.036, HR=1.907, HR 95% confidence interval=1.042–3.489) remained independent of tumor size (Table 2).
We compared our proposed prognostic indicator with six clinical factors known to be associated with survival in ER-negative breast cancer: node metastasis, tumor size, HER2 status, tumor area, lym, and patient age (Figure 4b), using the JT trend test for the categorical variables and Pearson’s correlation test for the continuous parameters. The strongest correlation with the co-localized hotspot index found was lym, where a Pearson’s correlation coefficient r of 0.212 (P=0.017) and 0.237 (P=0.007) was obtained for the discovery and validation cohorts, respectively. The association between our measure and the remaining factors was found to be weak (−0.07<r<0.17) or insignificant (JT>0.05).
Cancer–Immune Hotspots are Associated with Organ-Specific Metastasis
We next investigated whether any significant differences were present between patients with low and high co-localized hotspot scores and time to local and distant metastasis. Excluding patients whose tumors did not metastasize in our records, we found for the remaining patients that the mean time in months to local metastasis was significantly lower in patients with a low co-localized hotspot score (<1.91%) (63.8 vs 91.0, P=0.021). Similarly, the mean time in months to distant metastasis was found to be significantly lower in patients with a low co-localized hotspot score (26.9 vs 38.9, P=0.030). Analysis of metastasis location showed a pronounced difference between patients with a low and high co-localized hotspot score for metastasis in the bone (16.4 and 8.5%, respectively), liver (15.1 and 8.5%, respectively) and, to a lesser extent, lung (8.2 and 11.3%, respectively) and brain (8.2 and 10.2%, respectively)(Figure 5).
Immune Spatial Heterogeneity Further Stratifies Patients with High Lymphocyte Abundance
As there is a significant correlation between lym and our proposed co-localized hotspot index, we further compared their performances as prognostic factors in ER-negative breast cancer. Low levels of co-localized hotspots and lym both identified a group of patients with a more aggressive form of ER-negative breast cancer (Figures 6a and b). Here we identified 8.52% as the optimal cutoff for lym in all 245 samples and used this cutoff for the purpose of comparison. This cutoff is slightly different to the 8% we previously reported,12 which also has borderline significance in this sample set (P=0.078, Supplementary Materials). We discovered, first, that patients with a high abundance of immune cells do not necessarily have a high number of cancer–immune hotspots, while patients with a high number of hotspots can have a low level of immune cell abundance in the tumor (Figure 6c). This is expected as our hotspot score measures spatial heterogeneity of cancer and immune cell distribution; thus, despite high abundance, more uniformly distributed immune cells will receive a lower immune hotspot score. Second, our proposed score can further stratify patients with high lym into good and poor prognosis groups (P=0.007, Figure 6d). Finally, the prognosis of patients with low co-localized hotspot scores does not differ according to their lym (P=0.555).
Comparison of cancer–immune hotspots with lymphocyte abundance (lym). (a, b) Kaplan–Meier curves illustrating disease-specific survival differences between patient groups stratified by co-localized hotspots and lym, respectively, using all 245 ER-negative breast tumor samples. (c) Scatter plot to show correlation (quantified using Pearson’s method, top-right) between these two parameters. Dashed lines marked the critical thresholds for the parameters. Colors of the points correspond to groupings in panel (d). (d) Kaplan–Meier curves showing patient stratification using both indices. Cancer–immune hotspot score was able to further stratify patients with high lym (cyan and orange groups, P=0.007) but not those with low lym (dark blue and green groups, P=0.155). Lym could not stratify patients with a low cancer–immune hotspot score (cyan and dark blue groups, P=0.555).
Discussion
This study has brought together spatial statistics, image processing and pathological and clinical data to analyze 245 H&E-stained tumor sections from ER-negative breast cancer patients in the search for new understanding of the spatial heterogeneity of lymphocytic infiltration. The use of Getis–Ord hotspot analysis has been reported in a wide range of ecological studies, but we are thus far unaware of any previous application of this powerful statistical tool to analyze pathological images of breast tumors. Here it was used to describe spatial clusters or hotspots of cancer and immune cells, defined as regions in the tumor with a significantly high number of these cells given the global cell distribution. The most important findings of this study are that: (i) there is a significant correlation between a high fractional tumor area where cancer and immune hotspots are co-localized (high fC–I or co-localized hotspot score) and a favorable clinical outcome, (ii) this score, as our proposed prognostic indicator, can predict patient survival independently from known clinical parameters, and (iii) there is no significant correlation between our prognostic indicator and the routinely used clinical parameters. Furthermore, among patients whose tumors metastasized, those with low co-localized hotspot scores had significantly less time to local and distant metastasis and presented a twofold increased occurrence of metastasis to the bone and liver compared with those with high co-localized hotspot scores. This observation raises the question of whether cancer–immune hotspot co-localization is a feature of the microenvironment that provides organ-specific niche for successful metastasis.31, 32, 33
Notably, a weak correlation was found between the degree of cancer and immune hotspot co-localization and immune abundance, a parameter of clinical significance reported by us and other groups7, 10, 12 who showed that a high immune abundance is correlated with better survival outcome in ER-negative breast cancer. We were able to demonstrate that our hotspot score can further stratify patients with high immune abundance. Remarkably, patients with low hotspot scores, regardless of their immune abundance, had a similar, poor prognosis. This highlights the need to study heterogeneity of spatial distribution in addition to measuring abundance of microenvironmental components.
Our proposed approach scores a type of immune feature in pathological samples that is different from published assessment of lymphocytic infiltration,10, 11, 14 where tumor nests and stromal areas were scored based on whether infiltration by mononuclear inflammatory cells is present, thus evaluating the amount of intraepithelial or stromal immune infiltrates. In these studies, the authors did not find evidence of association between the degree of intra-tumor lymphocytic infiltration and clinical outcome. In contrast, our focus is on spatial aggregation of cancer cells and lymphocytes, thereby capturing spatial heterogeneity instead of abundance and frequency. The amount of heterogeneity was summarized as a ratio of spatial aggregation to tissue area, the quantification of which required the use of automated whole-section analysis, as it is impractical to visually account for every lymphocyte present. In samples we inspected visually, the majority of cancer–immune hotspots were located adjacent to tumor nests. ER-negative breast tumors are known to have a pushing growth pattern,34 and a future systematic investigation on distribution of hotspots according to tumor growth patterns could further our understanding of these hotspots.
The main strength of Getis–Ord hotspot analysis is that the global distribution of cells in the whole tumor is accounted for when assigning a local P-value indicative of cell clustering. Thus the identified clusters are not merely regions of high cell density but regions of significantly high cell density, which indicates spatial heterogeneity. Frequency mapping would not suffice for studying this heterogeneity, as frequency measures would not indicate how different regions compare with each other in terms of statistical significance. Compared with other methods in spatial statistics such as Ripley’s K, which gives a global P-value to indicate the trend of clustering,35 the distinct advantage of Getis–Ord hotspot analysis lies in its ability to pinpoint local regions of cell clustering. These regions will be important targets for follow-up experimental investigation to understand the molecular aberrations underlying cancer–immune co-localization—a clinically important phenomenon reported here. In our subsequent studies, immunohistochemical staining can be used to determine whether particular types of immune cells dominate these hotspots and whether cancer cells in these areas have a common marker that can explain the greater immune infiltration in their surrounding tissue. DNA sequencing and gene expression analysis of these select areas can further shed light on the biochemical framework underpinning the cancer–immune relationship. In addition, whether these hotspots form a particular biological structure is an interesting question, albeit beyond the scope of our present study.
The limitations of analyzing a three-dimensional structure on a two-dimensional scale inherent in all pathological assessment cannot be ignored. Any current sampling procedure can only approximate the state of the entire tumor. We evaluated cancer and immune hotspots based on an average of three sections from different locations within a tumor, thereby effectively approximating three-dimensional and inter-section heterogeneity. Furthermore, the association of our cancer–immune hotspot measure with patient survival is a significant one, having been discovered and validated across two independent patient cohorts, and thus there is undoubtedly valuable information to be found in two-dimensional tumor sections despite the approximation. In addition, H&E-stained tumor samples with × 20 magnification that were used in our study do not allow further sub-classification of lymphocytes; we identified lymphocytes in our image processing algorithm as nuclei with a small, round and dark morphology. However, determining lymphocytic infiltration in breast cancer based on H&E-stained samples has produced significant results in previous studies,9, 10, 11, 12 suggesting that, for the purpose of developing a prognostic biomarker, H&E samples may be sufficient in specific breast cancer subtypes. To enhance the potential clinical utility of our approach, we believe that it should be further tested on much larger sample sets, as well as extended to other cancer types where immune infiltration is often observed. In particular, following guidelines presented by Salgado et al36 (unpublished results), recommending exclusion of DCIS foci in visual assessment of tumor-infiltrating lymphocytes, we are investigating suitable approaches for implementing this in our computational image analysis pipeline.
In conclusion, the application of multidisciplinary techniques to understand the complex interplay between different cell types in a tumor is an emerging and promising area. With many image processing algorithms developed for automated detection of different tissue types and constituents, including cancerous and stromal tissue, automation allows for high-throughput processing while avoiding observer bias; for example, our hotspot score for a slide remains unchanged upon re-evaluation. Our study presents an alternative yet complementary method for studying tumor immune infiltration to the one presented by Salgado et al36 (unpublished), which is a powerful collaborative effort to standardize tumor immune infiltration scoring in routine diagnosis via visual inspection. Fully automated cell classification algorithms are not in mainstream clinical use at present, but we believe that our study demonstrates clear advantages of implementing computational methods to complement visual assessment by pathologists. In particular, we have shown that detecting cell locations using image analysis can allow the application of spatial statistical tools from other disciplines to effectively account for spatial heterogeneity in the tumor and its microenvironment, which can add valuable prognostic information.
References
Knight WA, Livingston RB, Gregory EJ et al, Estrogen receptor as an independent prognostic factor for early recurrence in breast cancer. Cancer Res 1977;37:4669–4671.
Miglietta L, Morabito F, Provinciali N et al, A prognostic model based on combining estrogen receptor expression and Ki-67 value after neoadjuvant chemotherapy predicts clinical outcome in locally advanced breast cancer: extension and analysis of a previously reported cohort of patients. Eur J Surg Oncol 2013;39:1046–1052.
Hoefnagel LD, Moelans CB, Meijer SL et al, Prognostic value of estrogen receptor alpha and progesterone receptor conversion in distant breast cancer metastases. Cancer 2012;118:4929–4935.
Weigelt B, Reis-Filho JS . Back to the basis: breast cancer heterogeneity from an etiological perspective. J Natl Cancer Inst 2014;106:1.
Brenton JD, Carey LA, Ahmed AA et al, Molecular classification and molecular forecasting of breast cancer: ready for clinical application? J Clin Oncol 2005;23:7350–7360.
Teschendorff AE, Miremadi A, Pinder SE et al, An immune response gene expression module identifies a good prognosis subtype in estrogen receptor negative breast cancer. Genome Biol 2007;8:R157.
Calabro A, Beissbarth T, Kuner R et al, Effects of infiltrating lymphocytes and estrogen receptor on gene expression and prognosis in breast cancer. Breast Cancer Res Treat 2009;116:69–77.
Ascierto ML, Kmieciak M, Idowu MO et al, A signature of immune function genes associated with recurrence-free survival in breast cancer patients. Breast Cancer Res Treat 2012;131:871–880.
Denkert C, Loibl S, Noske A et al, Tumor-associated lymphocytes as an independent predictor of response to neoadjuvant chemotherapy in breast cancer. J Clin Oncol 2010;28:105–113.
Loi S, Sirtaine N, Piette F et al, Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02-98. J Clin Oncol 2013;31:860–867.
Issa-Nummer Y, Darb-Esfahani S, Loibl S et al, Prospective validation of immunological infiltrate for prediction of response to neoadjuvant chemotherapy in HER2-negative breast cancer—a substudy of the neoadjuvant GeparQuinto trial. PLoS One 2013;8:e79775.
Yuan Y, Failmezger H, Rueda OM et al, Quantitative image analysis of cellular heterogeneity in breast tumors complements genomic profiling. Sci Transl Med 2012;4 157ra43.
Galon J, Costes A, Sanchez-Cabo F et al, Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science 2006;313:1960–1964.
Mahmoud SMA, Paish EC, Powe DG et al, Tumor-infiltrating CD8+ lymphocytes predict clinical outcome in breast cancer. J Clin Oncol 2011;29:1949–1955.
Kruger JM, Wemmert C, Sternberger L et al, Combat or surveillance? Evaluation of the heterogeneous inflammatory breast cancer microenvironment. J Pathol 2013;229:569–578.
Balsat C, Blacher S, Signolle N et al, Whole slide quantification of stromal lymphatic vessel distribution and peritumoral lymphatic vessel density in early invasive cervical cancer: a method description. ISRN Obstet Gynecol 2011;2011:354861.
Balsat C, Signolle N, Goffin F et al, Improved computer-assisted analysis of the global lymphatic network in human cervical tissues. Mod Pathol 2014;27:887–898.
Singanamalli A, Sparks R, Rusu M et al, Identifying in vivo DCE MRI parameters correlated with ex vivo quantitative microvessel architecture: a radiohistomorphometric approach. Proc SPIE 8676 Medical Imaging 2013: Digital Pathology, 867604 (March 29, 2013); doi:10.1117/12.2008136.
Doyle S, Feldman M, Tomaszewski J et al, A boosted Bayesian multiresolution classifier for prostate cancer detection from digitized needle biopsies. IEEE Trans Biomed Eng 2012;59:1205–1218.
Janowczyk A, Chandran S, Madabhushi A . Quantifying local heterogeneity via morphologic scale: distinguishing tumoral from stromal regions. J Pathol Inform 2013;4:8.
Basavanhally AN, Ganesan S, Agner S et al, Computerized image-based detection and grading of lymphocytic infiltration in HER2+ breast cancer histopathology. IEEE Trans Biomed Eng 2010;57:642–653.
Beck AH, Sangoi AR, Leung S et al, Systematic analysis of breast cancer morphology uncovers stromal features associated with survival. Sci Transl Med 2011;3:108ra13.
Belien JA, Somi S, de Jong JS et al, Fully automated microvessel counting and hot spot selection by image processing of whole tumor sections in invasive breast cancer. J Clin Pathol 1999;52:184–192.
Getis A, Ord JK . The analysis of spatial association by use of distance statistics. Geogr Anal 1992;24:189–206.
de Souza D, Kelly-Hope L, Lawson B et al, Environmental factors associated with the distribution of Anopheles gambiae s.s in Ghana; an important vector of lymphatic filariasis and malaria. PLoS One 2010;5:e9927.
Setiadi AF, Ray NC, Kohrt HE et al, Quantitative, architectural analysis of immune cell subsets in tumor-draining lymph nodes from breast cancer patients and healthy lymph nodes. PLoS One 2010;5:e12420.
Curtis C, Shah SP, Chin SF et al, The genomic and transcriptomic architecture of 2,000 breast tumors reveals novel subgroups. Nature 2012;486:346–352.
Francis K, Palsson BO . Effective intercellular communication distances are determined by the relative time constants for cyto/chemokine secretion and diffusion. Proc Natl Acad Sci USA 1997;94:12258–12262.
Cox DR . Regression models and life-tables. J R Stat Soc Series B Stat Methodol 1972;34:187–220.
Jonckheere AR . A distribution-free k-sample test against ordered alternatives. Biometrika 1954;41:133–145.
Valastyan S, Weinberg RA . Tumor metastasis: molecular insights and evolving paradigms. Cell 2011;147:275–292.
Wels J, Kaplan RN, Rafii S et al, Migratory neighbors and distant invaders: tumor-associated niche cells. Genes Dev 2008;22:559–574.
Gupta GP, Massague J . Cancer metastasis: building a framework. Cell 2006;127:679–695.
Putti TC, El-Rehim DMA, Rakha EA et al, Estrogen receptor-negative breast carcinomas: a review of morphology and immunophenotypical analysis. Mod Pathol 2004;18:26–35.
Ripley BD . The second-order analysis of stationary point processes. J Appl Probab 1976;13:255–266.
Salgado R, Denkert C, Demaria S et al, The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann Oncol 2014;26:259–271.
Acknowledgements
SN is a recipient of an EPSRC doctoral scholarship. The authors acknowledge funding from the Institute of Cancer Research. This work was supported by the Wellcome Trust [105104/Z/14/Z].
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Modern Pathology website
Supplementary information
Rights and permissions
About this article
Cite this article
Nawaz, S., Heindl, A., Koelble, K. et al. Beyond immune density: critical role of spatial heterogeneity in estrogen receptor-negative breast cancer. Mod Pathol 28, 766–777 (2015). https://doi.org/10.1038/modpathol.2015.37
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2015.37
This article is cited by
-
Spatial interplay of lymphocytes and fibroblasts in estrogen receptor-positive HER2-negative breast cancer
npj Breast Cancer (2022)
-
Tumour immunotherapy: lessons from predator–prey theory
Nature Reviews Immunology (2022)
-
Spatial distribution of B cells and lymphocyte clusters as a predictor of triple-negative breast cancer outcome
npj Breast Cancer (2021)
-
Combining multiple spatial statistics enhances the description of immune cell localisation within tumours
Scientific Reports (2020)
-
Pan-cancer computational histopathology reveals mutations, tumor composition and prognosis
Nature Cancer (2020)