Abstract
The aim of this study was to determine whether detection of β-HPV gene products, as defined in epidermodysplasia verruciformis skin cancer, could also be observed in lesions from kidney transplant recipients alongside the viral DNA. A total of 111 samples, corresponding to 79 skin lesions abscised from 17 kidney transplant recipients, have been analyzed. The initial PCR analysis demonstrated that β-HPV-DNA was highly present in our tumor series (85%). Using a combination of antibodies raised against the E4 and L1 proteins of the β-genotypes, we were able to visualize productive infection in 4 out of 19 actinic keratoses, and in the pathological borders of 1 out of 14 squamous cell carcinomas and 1 out of 31 basal cell carcinomas. Increased expression of the cellular proliferation marker minichromosome maintenance protein 7 (MCM7), that extended into the upper epithelial layers, was a common feature of all the E4-positive areas, indicating that cells were driven into the cell cycle in areas of productive viral infections. Although the present study does not directly demonstrate a causal role of these viruses, the detection of E4 and L1 positivity in actinic keratosis and the adjacent pathological epithelium of skin cancer, clearly shows that β-HPV are actively replicating in the intraepidermal precursor lesions of kidney transplant recipients and can therefore cooperate with other carcinogenic agents, such as UVB, favoring skin cancer promotion.
Similar content being viewed by others
Main
Solid organ transplantation is a treatment offered to an increasing number of patients with end-stage organ diseases. Although lifesaving, organ transplantation is associated with an overall three- to fivefold increased risk of malignancies.1, 2, 3, 4 Most of these cancers are caused by reactivated viruses whose oncogenic potential is suppressed by immunological reactions in healthy individuals, like Epstein–Barr virus-associated B-cell lymphomas, Kaposi’s sarcoma, caused by the reactivation of human herpesvirus type 8, and Merkel cell carcinoma of the skin, associated with Merkel cell polyomavirus.5, 6, 7, 8, 9
Of the cancers presenting in organ transplant recipients that have no established infectious etiology, skin cancer is the most frequent form (95%), including squamous and basal cell carcinomas.10, 11, 12, 13 The incidence of skin cancer, the most common cancer in fair-skinned populations, is at least 50-fold higher in organ transplant recipients.14, 15, 16 Large numbers of skin tumors (often more than 10) tend to develop over time in these at-risk subjects, thus presenting an enormous challenge for the patients and those responsible for their care.17, 18
Nearly all adults are persistently infected in the skin with many viruses belonging to the human papillomavirus (HPV) family.19, 20 Although they appear not to cause overt clinical symptoms in a great majority of infected individuals, they can cause cancer, either in skin or in genital sites, particularly in subjects with impaired immune function.21, 22, 23, 24, 25 To date, more than 150 HPV types have been completely sequenced and classified into five genera (and a series of intragenus species, indicated by Arabic numbers) based on DNA sequence analysis.26, 27 Of these, Alphapapillomaviruses (α-HPVs) are associated with genital cancer (eg, HPV16 and 18) and some genotypes with common skin warts.28 Skin-tropic Betapapillomaviruses (β-HPVs) (eg, HPV5 and 8) are evolutionarily distinct from the genus Alpha and appear to cause widespread unapparent or asymptomatic infections in the general population, but they have been associated with skin cancer in the immunocompromised host.29
The relationship between β-HPV infection and skin cancer has been clearly defined in patients suffering from the rare inherited disease epidermodysplasia verruciformis, an autosomal recessive disease characterized by a predisposition to infection by specific types of β-HPV.30, 31, 32 In these patients, HPV5 and 8 replicate very efficiently and reveal their full transforming potential, inducing multiple cutaneous neoplasia.33, 34
Emerging evidence also supports the role of β-HPV in skin cancer development in immunosuppressed individuals. Seroepidemiological studies have associated skin cancer in organ transplant recipients with the presence of anti-β-HPV antibodies, and PCR-based studies have identified β-HPV DNA in over 80% of skin tumors from these patients.22, 35, 36, 37, 38, 39, 40, 41, 42, 43 Despite these findings, a causal role of these viruses has been difficult to verify because of their ubiquitous prevalence in the general population and their absence in some cancers.25, 44 The major weakness of the available studies is that the proposed association is mostly based on the presence of viral DNA in tumor tissues or positive antibody responses. Very few studies have addressed whether the β-HPV detected in these cases are actually localized within the malignant cells or whether they are transcriptionally active, the confirmation of which would greatly strengthen the evidence for a carcinogenic role of these pathogens.
In a recent study, we examined the β-HPV life cycle in skin tumors obtained from epidermodysplasia verruciformis patients and found that, similar to what has been seen with other PV types, the onset of vegetative viral genome amplification coincides closely with the cytoplasmic expression of the viral protein E4 during productive infection.33 This pattern was observed in all areas of the tumors where there was still some morphological differentiation of the epithelium. In addition, we have also demonstrated, using fluorescent in situ hybridization (FISH), that the abundance of β-HPV seen in some lesions was a direct result of genome amplification within the carcinoma tissue.34 Overall, our results indicated that E4 staining could be exploited as a marker of viral expression during β-HPV-associated skin cancer progression as reported in the HPV8 transgenic mouse model and in cervical disease for the α-genotypes.33, 45, 46, 47
To extend the data obtained so far in epidermodysplasia verruciformis patients to other groups of patients at high risk of developing skin cancer, here we studied a series of skin lesions from kidney transplant recipients attending our University Hospital by systematically analyzing for the presence of β-HPV infection both at the DNA (PCR) and protein level. Using a combination of antibodies raised against the E4 and L1 proteins of the β-genotypes, we were able to visualize the completion of viral life cycle in some precancerous lesions such as actinic keratosis or at the periphery of more advanced disease. These data demonstrate that β-HPV transcription occurs at the site of skin transformation in the organ transplant recipient setting and also points to its possible involvement in the process of skin carcinogenesis.
Materials and methods
Sample Collection
Tissue sections were obtained from 111 formalin-fixed and paraffin-embedded blocks, previously collected from 79 skin lesions and stored in the University Hospital medical material archives. For some lesions, only a single block was available, denominated ‘whole lesion’ (WL), whereas for the others, two blocks existed, corresponding to the core (C) and edges (E) of the lesion. All lesions were excised from 17 kidney transplant recipients, while one among them had heart transplant twice (16 male and 1 female), receiving transplants between 1998 and 2009. Data on skin lesion development and characteristics were retrieved from pathology archives and clinical records. The mean length of patient follow-up following kidney transplantation was 15 years and 4 months±7 years and 8 months. A single formalin-fixed and paraffin-embedded block from a wart-like lesion of a patient with epidermodysplasia verruciformis was also analyzed in the present study as positive control.
Written informed consent was obtained by all subjects according to the Declaration of Helsinki and approval was obtained from the local ethic committee.
β-HPV DNA Detection and Genotyping with the PM-PCR Reverse Hybridization Assay
Two consecutive 10-μm-thick sections were retrieved from formalin-fixed and paraffin-embedded samples and used to extract DNA by means of the QIAamp Tissue Kit (Qiagen srl, Milan, Italy) according to the manufacturer’s instructions. To prevent cross-contamination, the microtome was thoroughly cleaned following the sectioning of each block and a new blade installed for the next. β-HPV detection and genotyping was carried out using the PM-PCR reverse hybridization assay (Skin β-HPV prototype research assay; Diassay BV, Rijswijk, The Netherlands), as described previously.48 The method was designed to identify the 25 established β-HPV types (ie, HPV genotypes 5, 8, 9, 12, 14, 15, 17, 19, 20, 21, 22, 23, 24, 25, 36, 37, 38, 47, 49, 75, 76, 80, 92, 93 and 96). The PM-PCR reverse hybridization assay, which generated a biotinylated amplimer of 117bp from the E1 region, was carried out following all the precautions indicated by the manufacturer to avoid recurrence of cross-contamination. Briefly, PM-PCR was performed in a final reaction volume of 50 μl, containing 10 μl of the isolated DNA, 2.5 mM MgCl2, 1 × GeneAmp PCR buffer II, 0.2 mM deoxynucleoside triphosphates, 1.5 U Amplitaq Gold DNA polymerase and 10 μl of the PM primer mix. The PCR was performed by a 9-min preheating step at 94 °C, followed by 35 cycles of amplification comprising 30 s at 94 °C, 45 s at 52 °C and 45 s at 72 °C. PCR was ended by a final elongation step of 5 min at 72 °C. As a positive PCR control, a β-HPV plasmid clone was included. Identification of the amplified HPV types was performed by reverse hybridization analysis of the amplimers on genotyping strips provided by the manufacturer. In each strip a probe line contains a mix of ‘universal’ HPV probes: in some cases, these probes are positive without a probe for specific β-HPV being positive, indicating the presence of an unspecified β-HPV. These cases are indicated as ‘unspecified β-papillomavirus genotype.’
Antibodies and Generation of Anti-L1 Antibodies
To generate antibodies that can broadly identify the L1 proteins of the β-genotypes, sequence alignments were first carried out, and the highly conserved region between amino acid 200 and 300 was chosen. This region of the HPV5 full-length protein (Ref. Seq.: NP_041372.1) was amplified by PCR from an HPV5 genomic clone recently isolated from an epidermodysplasia verruciformis patient. The primer sequences used were: L1 forward, 5′-CGCGGATCCCGTCTGTATCCAAAACCCTTG-3′; L1 reverse, 5′-CCGCTCGAGTTATCCTATAGTCTTTTGAGCTTG-3′. The forward primers included a BamHI site (underlined) upstream of the ATG initiation codon, whereas the reverse primers contained a XhoI sequence (underlined). Amplimers were cloned into the pGEX-4T-2 vector (GE Healthcare Europe GmbH, Milan, Italy), and then expressed in the Escherichia coli host BL21. GST-L1 fusion protein was dialyzed overnight at 4 °C in 50 mM Tris-HCl (pH 8.5), 0.5% β-mercaptoethanol and 3 M urea, and then redialyzed for 12 h at 4 °C in 50 mM Tris-HCl (pH 8.5) and protease inhibitors (Sigma). Antisera were raised by injecting rabbits with the dialyzed GST-L1 fusion protein. Animals were bled 1 week after the fourth immunization and serum immunoglobulins obtained by precipitation with 45% saturated ammonium sulfate. The precipitate was then resuspended in phosphate-buffered saline (PBS) and purified on a protein A affinity column (GE Healthcare) according to the supplier’s specifications. Preimmune serum was collected before the initiation of the immunization protocol and was used as a control in the immunostaining experiments.
The production of polyclonal antibodies to HPV5E4, which crossreact with many genotypes from species 1, including HPV8, 14, 20, 24, 25 and 36, has been described previously.33 Antibodies to minichromosome maintenance protein 7 (MCM7) were obtained from Neomarkers (Fremont, CA, USA) (MS-862-p1).
Immunofluorescent Detection
Consecutive 5-μm-thick sections obtained from formalin-fixed and paraffin-embedded tissues were processed for immunofluorescent detection of antigens coupled to DNA-FISH as described previously.49 For the other markers analyzed (E4, MCM7, L1), antigen unmasking was performed by heating the slides in a conventional decloaking chamber, where they were placed for 10 min at 121 °C in 10 mM citrate buffer at pH 6.0 (Vector Laboratories, Burlingame, CA, USA). The immunofluorescent protein–protein double detection (HPV5 E4-MCM7) was carried out by incubating the slides overnight at 4 °C with the primary antibody anti-MCM7 (1:200) diluted in 5% normal goat serum (NGS), followed by amplification with TSA (Tyramide Signal Amplification; Perkin-Elmer, Waltham MA, USA); then, slides were incubated with the primary antibody anti-HPV5 E4 (1:1000) for 3 h and subsequently with the appropriate fluorescent secondary antibody. The immunofluorescence (IF) for L1 detection was carried out by incubating the slides overnight at 4 °C with the primary antibody anti-L1 (1:1000) diluted in 5% NGS-PBS followed by incubation with the appropriate fluorescent secondary antibody. Images were acquired using a digital scanner (Pannoramic MIDI; 3D Histech Kft., Budapest, Hungary). For the assessment of histological features, the slides analyzed by HPV5 E4-MCM7 were disassembled and stained with hematoxylin and eosin (H&E).
Results
Patients and Skin Lesion Characteristics
The baseline characteristics of the study population and the histological features of the cutaneous lesions, alongside the relative number of lesions, the year in which they occurred following transplantation and their location at sun-exposed or unexposed sites are listed in Table 1. The median time of skin lesion occurrence was 7±5 years after transplantation. Patients are numbered in ascending order based on the number of tumors developed. Within 10 years from transplantation, 5 patients developed more than 5 lesions (patients 13–17), mostly in sun-exposed sites, confirming sun exposure to be a major contributor to epithelial transformation. The skin lesions included: squamous cell carcinoma (n=14) and basal cell carcinoma (n=31), followed by precancerous lesions such as actinic keratosis (n=19), Bowen’s disease (n=1) and keratoacanthoma (n=7), and benign lesions such as seborrheic keratosis (n=7). The proportion of lesions affecting sun-exposed skin areas (head, hands and forearms) was 59 out of 79 lesions (75%).
β-HPV-Type Determination
The results of β-HPV testing of the DNA extracted from the 79 lesions are shown in Table 2. In 28 cases, multiple biopsy blocks were available corresponding to either the core or edges of the lesions. Out of the 111 formalin-fixed and paraffin-embedded blocks analyzed, 94 were HPV positive (85%) and 86 samples (77%) could be genotyped as containing at least one of the 25 β-HPV genotypes available on the reverse hybridization assay (Table 2).
The spectrum of β-genotypes identified for each lesion from the 17 study patients is reported in Supplementary Table 1. In cases of multiple biopsies, the genotypes found in the core and edges of the tumors are combined. The most frequently observed genotypes are HPV5 and 8 (both belonging to species 1), which were found in 51 (65%) and 20 (25%) of the 79 lesions, respectively. HPV5 was detected as a single infection in 18 out of the 79 lesions (23%) and HPV8 was detected as a single infection in two lesions (3%). Multiple infections with two genotypes were found in 13 lesions (16%), while more than two genotypes were found in 28 lesions (35%). In the five patients exhibiting more than 5 tumors, HPV5 alone or in multiple infections was found in 38 (66%) of the 58 lesions present on these 5 patients. Considering just the genotypes belonging to species 1, including HPV5, 8, 12, 14, 19, 24, 25, 36 and 93, 61 tumors (77%) turned out to be positive for at least one genotype. For the lesions split into more formalin-fixed and paraffin-embedded blocks (n=36), at least one β1-genotype was consistently found in 15 (42%) of them (data not shown).
Visualization of Viral Protein Expression in Skin Lesions
Previous studies from our group have demonstrated that detection of the abundant viral E4 protein is helpful for the visualization of active β-HPV infection in skin tumors from epidermodysplasia verruciformis patients.33, 34 Figure 1 shows representative images of tissue sections from a benign wart-like lesion from an epidermodysplasia verruciformis patient displaying the unequivocal histological features associated with the infection, including acanthosis and the disorganization of the granular layers defined by an abrupt variation in keratoyaline granules. The E4-positive cells are enlarged and display prominent blue-gray pallor with occasional perinuclear halos. HPV8 DNA-FISH analysis confirmed that these cells are supporting viral genome amplification as visualized by many positive nuclei for overlapping cytoplasmic E4 staining. Completion of the viral life cycle was also defined by L1 staining performed using in-house polyclonal antibodies raised against a common region of the β-genus major capsid protein. As expected, L1-positive nuclei were detected in the more superficial layers of the E4-positive area.50 The cellular proliferation marker MCM7 was also strongly increased in the lesion compared with the adjacent normal epithelium being most apparent in the basal and suprabasal layers, indicating that cells were stimulated to enter the cell cycle.49, 51
Distribution of the viral and cellular markers E4, L1, human papillomavirus 8 (HPV8) DNA and minichromosome maintenance protein 7 (MCM7) in a wart-like lesion from an epidermodysplasia verruciformis patient (elbow). The top images show the scan of the hematoxylin and eosin (H&E) histological staining (left) and immunofluorescence (IF) staining (MCM7 in red; E4 in green) (right) of the same tissue section. The white dotted line indicates the basal layer. In the lower panel, the above-mentioned MCM7/E4 staining is reproduced (left picture) and serial sections were double stained for the presence of viral genome amplification by HPV8 DNA-fluorescent in situ hybridization (FISH) (red) and for E4 expression (green) (middle picture), and stained with antibodies to L1 (red) (right picture). The region shown corresponds to the red square highlighted in the H&E image. The white arrows indicate nuclear L1 staining. All sections were counterstained with 4′,6-diamidino-2-phenylindole (DAPI) (blue) to visualize cell nuclei. Scale bars: 100 μm.
To investigate whether similar images of productive infection could be visualized in organ transplant recipients skin lesions, tissue specimens from the available formalin-fixed and paraffin-embedded blocks were costained using IF analysis with anti-E4 and anti-L1 antibodies to detect viral antigen expression, and with MCM7, a marker of cellular proliferation.
Out of the 111 formalin-fixed and paraffin-embedded blocks analyzed, E4-positive cells were found in six blocks (for brevity, referred to as IF-positive), originating from patients 5, 8, 16 and 17, and corresponding to four actinic keratosis lesions, and the adjacent pathological area of one squamous cell carcinoma and one basal cell carcinoma. Patients 16 and 17 were transplanted in 1993 and 1999, respectively, and developed 14 skin lesions each in their post-transplant period. The other two patients received transplants in 2002 and 2005, respectively. Table 3 summarizes all the lesions developed by the IF-positive patients and reports the details of the genotyping results for each formalin-fixed and paraffin-embedded block available, distinguishing the different parts of the lesions (edges, core or WL). As expected from the spectrum of the polyclonal anti-E4 antibody used, all the IF-positive sections harbored genotypes belonging to species 1.
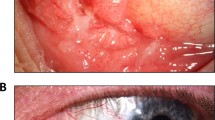
Having established the epidermodysplasia verruciformis staining pattern, we carefully went through all the E4-positive areas identified in our tumor series, looking for their major histological characteristics and staining patterns, and the most representative images are presented. Figure 2 shows one of the two E4-positive areas detected in the adjacent pathological epithelium from a basal cell carcinoma of the neck. The epithelium displays acanthosis and both the E4 and L1 staining patterns show great resemblance to those obtained from the epidermodysplasia verruciformis patient shown in Figure 1. Figure 3 summarizes the staining obtained from patient 8, focusing on the positive area found in the bowenoid actinic keratosis, located next to the squamous cell carcinoma. This area shows clear signs of β-HPV-related cytopathic effects, some cells display pleomorphism and nuclear atypia and again both early and late viral markers of β-HPV infection are present.
Distribution of the viral and cellular markers E4, L1 and minichromosome maintenance protein 7 (MCM7) in a basal cell carcinoma from a kidney transplant recipient (patient 5, neck). The top picture shows the scan of the tissue section using hematoxylin and eosin (H&E) staining (scale bar: 1000 μm). The blue circle shows the basal cell carcinoma and the red square indicates the area of interest in the adjacent epithelium. The region shown in the lower panels (scale bars: 100 μm) corresponds to the red square highlighted in the overall H&E image, magnified in the left-hand lower panel. In the middle picture, the same section was double stained using antibodies to E4 (green) and MCM7 (red), and a serial section was stained with antibodies to L1 (red) (right picture). The white arrows indicate nuclear L1 staining. All sections were counterstained with 4′,6-diamidino-2-phenylindole (DAPI) (blue) to visualize cell nuclei.
Distribution of the viral and cellular markers E4, L1 and minichromosome maintenance protein 7 (MCM7) in a bowenoid actinic keratosis from a kidney transplant recipient (patient 8, neck). The top pictures (scale bars: 1000 μm) show the scan of the tissue sections using hematoxylin and eosin (H&E) staining; the right-hand panel shows an actinic keratosis with the area of interest boxed in red and the left panel shows a nearby squamous cell carcinoma. The region shown in the lower panels corresponds to the red square highlighted in the H&E image, magnified in the left-hand lower picture. The same section was double stained using antibodies to E4 (green) and MCM7 (red) (middle picture) and a serial section was stained with antibodies to L1 (red) (right picture). The white arrows indicate nuclear L1 staining. All sections were counterstained with 4′,6-diamidino-2-phenylindole (DAPI) (blue) to visualize cell nuclei. Scale bars: 50 μm.
Three hypertrophic actinic keratosis, from the same patient (patient 16), are reported in Figure 4a–c. Figure 4a shows a clearcut area of positivity found in an epithelial crevice, where disruption of the granular layer was clearly evident alongside parakeratosis. In this case, it was also possible to perform FISH with the single genotype found, specifically HPV25; where FISH-positive nuclei neatly overlapped with some E4-positive cells in the cytoplasm, L1 positivity was confined to some parakeratotic nuclei. The positive area reported in Figure 4b was found in the pathological edge of an actinic keratosis and shows the typical staining pattern and cytopathic effects of productive β-HPV infection. The actinic keratosis of Figure 4c shows a positive area corresponding to a highly parakeratotic epithelium that abruptly changed to normal orthokeratosis on both sides. As expected from the high grade of parakeratosis, many L1-positive nuclei were found above the E4-positive cells. Consistent with the staining seen in the epidermodysplasia verruciformis lesion shown in Figure 1, MCM7 expression was increased in all the E4-positive areas, being present in the basal layer and above (see especially Figure 4b). This staining decreased following the onset of E4 expression, although a region of overlap was well apparent where E4-MCM7-double-positive cells were found.
Distribution of the viral and cellular markers E4, L1, human papillomavirus 25 (HPV25) DNA and minichromosome maintenance protein 7 (MCM7) in three cases of hypertrophic actinic keratosis from a kidney transplant recipient (patient 16, a. hand; b. face; c. hand). (a) The top picture (scale bar: 1000 μm) shows the scan of the tissue section of the first actinic keratosis using hematoxylin and eosin (H&E) staining. The region shown in the lower panels corresponds to the red square highlighted in the over H&E image, reproduced in the lower left-hand picture. The same section was double stained using antibodies to E4 (green) and MCM (red) (second picture); serial sections were double stained for the presence of viral genome amplification by HPV25 DNA-fluorescent in situ hybridization (FISH) (red) and for E4 expression (green) (third picture), and also stained with antibodies to L1 (red) (fourth picture). The white arrows indicate nuclear L1 staining. All sections were counterstained with 4′,6-diamidino-2-phenylindole (DAPI) (blue) to visualize cell nuclei. Scale bars: 50 μm. (b) The top pictures (scale bars: 1000 μm) show the scan of the tissue sections (using H&E staining) of the second actinic keratosis (left picture) and its edge (right picture). The right-handed middle panel shows the histology (H&E staining) of the area from the edge where viral markers were expressed (red square) and an overall picture of the immunofluorescence (IF) staining (E4 in green; MCM7 in red) of the same tissue section (scale bars: 200 μm). The white dotted line indicates the basal layer. In the lower panel, the above MCM7/E4 staining is reproduced (left picture) and serial sections were stained with antibodies to L1 (red) (right picture). The white arrows indicate nuclear L1 staining. Scale bars: 100 μm. All sections were counterstained with DAPI (blue) to visualize cell nuclei. (c) The top picture shows the scan of the tissue section of the third actinic keratosis using H&E staining (scale bar: 1000 μm). The black rectangle shows a magnification (scale bar: 400 μm) of the positive parakeratotic epithelium that abruptly changed to normal orthokeratosis on both sides. The region shown in the lower panels corresponds to the red square highlighted in the H&E image, reproduced in the lower left-hand picture. The same section was double stained using antibodies to E4 (green) and MCM7 (red) (middle picture) and a serial section was stained with antibodies to L1 (red) (right picture). Scale bars: 50 μm. All sections were counterstained with DAPI (blue) to visualize cell nuclei.
A clear area of positivity was also found in the adjacent pathological epithelium of a squamous cell carcinoma, as reported in Figure 5. Here, the cytopathic effect is remarkable and unequivocally similar to what is generally found in intraepidermal precursor lesions from epidermodysplasia verruciformis and HIV patients.33, 52 Many E4-positive cells are present, as well as superficial L1-positive nuclei. Unfortunately, although performed and present, we are not able to show FISH positivity with HPV24 because this slide turned out to be very fragile and got severely damaged during processing.
Distribution of the viral and cellular markers E4, L1 and minichromosome maintenance protein 7 (MCM7) in the adjacent epithelium of a squamous cell carcinoma from a kidney transplant recipient (patient 17, ear). The top pictures shows the scan of the tissue sections (hematoxylin and eosin (H&E) staining) of the squamous cell carcinoma (left picture; scale bar: 500 μm) and its edge (right picture; scale bar: 1000 μm). In the lower panel, the same sections were stained using antibodies to E4 (green) (middle picture) and serial sections were stained with antibodies to L1 (red) (right picture). The region shown corresponds to the red square highlighted in the H&E image. Scale bars: 50 μm. All sections were counterstained with 4′,6-diamidino-2-phenylindole (DAPI) (blue) to visualize cell nuclei. The inset in the lower left picture shows the cytopathic effects typical of a productive β-human papillomavirus (HPV) infection (scale bar: 20 μm).
In addition, the H&E staining of all the tissue sections that were negative for viral markers were carefully screened for the signs of any cytopathic effects, while none observed.
Discussion
To our knowledge, this is the first study in which the association between skin lesions and β-HPV infection has been assessed at both the DNA level by PCR and at the protein level by IF analysis. The main aim of this study was to determine whether detection of β-HPV gene products, as defined in skin tumors from epidermodysplasia verruciformis patients, could also be observed in lesions from kidney transplant recipients. We chose to compare the kidney transplant recipients setting with epidermodysplasia verruciformis because they share the following two main features: (i) a status of chronic immunosuppression, which may favor persistence or reactivation of latent skin-tropic viruses including β-HPV; and (ii) the high risk of developing multiple skin cancers.9, 10, 12 These commonalities are also valid for patients affected by primary immunodeficiencies in general.53 In addition, in this study the epidermodysplasia verruciformis model served as an important tool for optimizing the staining procedure with anti-E4 and L1 antibodies, and was used as a positive control when examining kidney transplant recipient tissue sections. A polyclonal antibody recognizing the E4 protein from species 1 was used alongside a newly generated polyclonal antibody raised against a highly conserved region of the L1 protein from the β genus. In addition, to increase the chances of success, the biopsy blocks containing the normal surrounding areas of the tumors were also processed for the viral markers for a total of 111 formalin-fixed and paraffin-embedded corresponding to 79 skin lesions abscised from 17 kidney transplant recipients.
The initial PCR analysis demonstrated that β-HPV-DNA was highly present in our specimens, with 94 blocks (85%) resulting positive. Multiple infections were observed in 41 lesions (52%), and at least one genotype belonging to the β1 species was found in 79 of the 111 blocks analyzed by PCR (71%).
When we analyzed the same specimens by IF, six blocks showed areas of positivity corresponding to four actinic keratosis, and the adjacent pathological epithelium of one basal cell carcinoma, and one squamous cell carcinoma. The E4-positive areas were found in the context of the disorganized epithelium in the actinic keratosis lesions, whereas in the more advanced tumors, such as squamous cell carcinoma and basal cell carcinoma, they were always localized to the adjacent pathological epithelium. In all the specimens, the viral E4 protein displayed the expected cytoplasmic localization in the middle-superficial layers of the epithelium accompanied by an increase of the cellular proliferation marker MCM7 in the basal and suprabasal layers. The disappearance of E4 positivity in the adjacent normal epithelium constantly overlapped with a reduction in MCM7 expression, which was restricted to the basal layer. These findings support the hypothesis that β-HPV replication drives the cells above the basal layer to enter the cell cycle to facilitate the amplification of its genome. Consistent with this observation, FISH-positive nuclei for the viral genome were found in some of the E4-positive cells. As further proof that the viral life cycle was being completed, all the E4-positive areas showed expression of the major coat protein (L1), which also occurred in a subset of E4-positive cells in the upper layers. This is fully consistent with what has been seen with other PV types, where the onset of vegetative viral genome amplification coincides closely with the expression of cytoplasmic E4 and nuclear L1 in some very superficial cells during productive infection.49, 50, 51 In one highly differentiated actinic keratosis, the number of L1-positive nuclei was very high and most of them were in the thick layers of parakeratosis.
A common trait of cancers with a well-documented viral etiology is their high incidence in immunosuppressed individuals.5, 6, 7, 8, 9 As skin cancer is the most prevalent tumor in the organ transplant recipient setting, one would expect that viruses may contribute to this well-documented increased susceptibility and incidence. The discovery and detection of β-HPV-DNA and its active infection in epidermodysplasia verruciformis patients provided an important new insight into the viral oncogenesis of skin cancer that might be extendable to other subsets of patients including other primary immunodeficiencies and particularly long-lasting iatrogenically immunosuppressed patients, such as organ transplant recipients. Despite many efforts, direct evidence of active β-HPV infection in tumors from non-epidermodysplasia verruciformis patients were still missing and the major criticism against a direct involvement of these viruses in skin cancer in the general population is that they do not seem to be maintained in high-grade tumors, such as squamous cell carcinoma. To date, the evidence suggesting a causal role of β-HPV in skin cancer has been tainted by: the finding that viral DNA is also found in normal skin, that discovery of the viral genome copy number is usually much less than one viral genome per tumor cell and the fact that viral transcripts have not been identified by high-throughput mRNA sequencing.19, 54, 55, 56, 57 Alongside the fact that ubiquitous β-HPV DNA carriage does not necessarily indicate active infection, these issues have created and so far maintained a state of uncertainty about the causative role of β-HPVs in non-epidermodysplasia verruciformis skin cancer. Although the present study does not directly demonstrate a causal role of these viruses, the detection of E4 and L1 positivity in (i) actinic keratosis, which are widely regarded to be squamous cell carcinoma precursors or in situ carcinoma, and (ii) the adjacent pathological epithelium of one squamous cell carcinoma and one basal cell carcinoma, clearly shows that β-HPV are actively replicating in the lesional skin of organ transplant recipients and can therefore cooperate with other carcinogenic agents, such as UVB, favoring skin cancer promotion and progression.
Our data are fully consistent with the model proposed by Weissenborn et al 55 in 2005, who demonstrated that the highest β-HPV loads are present in actinic keratosis, rather than in squamous cell carcinoma, suggesting that their persistence may not be necessary for the maintenance of the malignant phenotype. Instead, they may act as a cofactor that enhances the carcinogenic potential of UV damage, as shown by Wallace et al,58 who also demonstrated that β-HPV E6 expression can enhance the carcinogenic potential of UV exposure by promoting p300 degradation.
If β-HPV infections has a role in skin cancer, then they must do so transiently and very likely upon reactivation or persistence in the immunocompromised host. Our findings, showing active β-HPV infection in precancerous lesions and in the vicinity of malignant tumors, are fully compatible with a role of these viruses in the early steps of skin carcinogenesis in at least the immunosuppressed setting. These data are consistent with the ‘hit-and-run’ mechanisms of carcinogenesis, with cutaneous HPV being possibly important for tumor initiation and progression but not necessary for tumor maintenance.59, 60 Consistent with a causal role in the early stage of the disease, E4 positivity was clearly visualized in an actinic keratosis that was localized adjacent to a squamous cell carcinoma in the neck region. In addition, increased MCM7 expression that extended into the upper epithelial layers was a common feature of all the E4-positive areas, indicating that cells were driven into the cell cycle in areas of productive viral infections.23, 49, 50 The observed stimulation of basal cell proliferation may contribute, in association with other transforming agents, such as UVB irradiation, to the transformation process without necessarily being maintained in the more advanced disease.
Assuming that viral replication is more active at very early stages of carcinogenesis and perhaps when lesions are not yet even clinically evident, it is reasonable to propose that when lesions are removed, especially in more advance stages, only some residual areas are detectable that exhibit viral replication. It is also worth mentioning that the areas of positivity were usually found in lesions that were originally split in more than one formalin-fixed and paraffin-embedded blocks. This procedure is currently applied when the surgical specimen is quite big and the different areas of the lesion are macroscopically evident as it is occurring when the erythematosus area surrounding the tumor is also surgically removed. This can also be defined as field cancerization. These assumptions can explain the low percentage of positivity found in this kind of study and the need of more thorough investigation of the perilesional skin where the likelihood of finding active β−HPV infection should be higher.
In summary, our work shows that careful detection of β-HPV gene products at the single-cell level allows us to visualize their sites of replication, especially in intraepidermal precursor lesions and the marginal zones of more advanced disease. However, these findings require further research to improve our knowledge of β-HPV natural infection and reactivation, which will help to understand how it is influenced by the epithelial site, UVB exposure and the immune system.
References
Tessari G, Naldi L, Boschiero L et al. Incidence of primary and second cancers in renal transplant recipients: a multicenter cohort study. Am J Transplant 2013;13:214–221.
Stratta P, Morellini V, Musetti C et al. Malignancy after kidney transplantation: results of 400 patients from a single center. Clin Transplant 2008;22:424–427.
Hall EC, Pfeiffer RM, Segev DL et al. Cumulative incidence of cancer after solid organ transplantation. Cancer 2013;119:2300–2308.
Piselli P, Serraino D, Segoloni GP et alImmunosuppression and Cancer Study Group. Risk of de novo cancers after transplantation: results from a cohort of 7217 kidney transplant recipients, Italy 1997–2009. Eur J Cancer 2013;49:336–344.
Piselli P, Busnach G, Fratino L et al. De novo malignancies after organ transplantation: focus on viral infections. Curr Mol Med 2013;13:1217–1227.
Schulz TF . Cancer and viral infections in immunocompromised individuals. Int J Cancer 2009;125:1755–1763.
Piselli P, Busnach G, Citterio F et al. Risk of Kaposi sarcoma after solid-organ transplantation: multicenter study in 4,767 recipients in Italy, 1970–2006. Transplant Proc 2009;41:1227–1230.
Grulich AE, van Leeuwen MT, Falster MO et al. Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: a meta-analysis. Lancet 2007;370:59–67.
THE SCOPE Collaborative Group. Skin Cancer After Organ Transplantation. Springer: Berlin, 2009;502 pp.
Euvrard S, Kanitakis J, Claudy A . Skin cancers after organ transplantation. N Engl J Med 2003;348:1681–1691.
Villeneuve PJ, Schaubel DE, Fenton SS et al. Cancer incidence among Canadian kidney transplant recipients. Am J Transplant 2007;7:941–948.
Wisgerhof HC, Edelbroek JRJ, de Fijter JW et al. Subsequent squamous- and basal-cell carcinomas in kidney-transplant recipients after the first skin cancer: cumulative incidence and risk factors. Transplantation 2010;89:1231–1238.
Wisgerhof HC, van der Geest LGM, de Fijter JW et al. Incidence of cancer in kidney-transplant recipients: a long-term cohort study in a single center. Cancer Epidemiol 2011;35:105–111.
Kovach BT, Stasko T . Skin cancer after transplantation. Transplant Rev 2009;23:178–189.
Jensen AØ, Lamberg AL, Jacobsen JB et al. Non-melanoma skin cancer and ten-year all-cause mortality: a population-based cohort study. Acta Dermatol Venereol 2010;90:362–367.
Buell JF, Hanaway MJ, Thomas M et al. Skin cancer following transplantation: the Israel Penn International Transplant Tumor Registry experience. Transplant Proc 2005;37:962–963.
Hofbauer GFL, Bouwes Bavinck JN, Euvrard S . Organ transplantation and skin cancer: basic problems and new perspectives. Exp Dermatol 2010;19:473–482.
Rüegg CP, Graf N, Mühleisen B et al. Squamous cell carcinoma of the skin induces considerable sustained cost of care in organ transplant recipients. J Am Acad Dermatol 2012;67:1242–1249.
De Koning MNC, Struijk L, Bavinck JNB et al. Betapapillomaviruses frequently persist in the skin of healthy individuals. J Gen Virol 2007;88:1489–1495.
Foulongne V, Sauvage V, Hebert C et al. Human skin microbiota: high diversity of DNA viruses identified on the human skin by high throughput sequencing. PLoS One 2012;7:e38499.
Nindl I, Rösl F . Molecular concepts of virus infections causing skin cancer in organ transplant recipients. Am J Transplant 2008;8:2199–2204.
Bouwes Bavinck JN, Neale RE, Abeni D et al. Multicenter study of the association between betapapillomavirus infection and cutaneous squamous cell carcinoma. Cancer Res 2010;70:9777–9786.
Doorbar J, Quint W, Banks L et al. The biology and life-cycle of human papillomaviruses. Vaccine 2012;30 (Suppl 5):F55–F70.
Akgül B, Cooke JC, Storey A . HPV-associated skin disease. J Pathol 2006;208:165–175.
Arron ST, Jennings L, Nindl I et al. Viral oncogenesis and its role in nonmelanoma skin cancer. Br J Dermatol 2011;164:1201–1213.
De Villiers E-M . Cross-roads in the classification of papillomaviruses. Virology 2013;445:2–10.
Bernard H-U . Taxonomy and phylogeny of papillomaviruses: an overview and recent developments. Infect Genet Evol 2013;18:357–361.
McLaughlin-Drubin ME, Meyers J, Munger K . Cancer associated human papillomaviruses. Curr Opin Virol 2012;2:459–466.
Bravo IG, de Sanjosé S, Gottschling M . The clinical importance of understanding the evolution of papillomaviruses. Trends Microbiol 2010;18:432–438.
Lazarczyk M, Cassonnet P, Pons C et al. The EVER proteins as a natural barrier against papillomaviruses: a new insight into the pathogenesis of human papillomavirus infections. Microbiol Mol Biol Rev 2009;73:348–370.
Lazarczyk M, Pons C, Mendoza J-A et al. Regulation of cellular zinc balance as a potential mechanism of EVER-mediated protection against pathogenesis by cutaneous oncogenic human papillomaviruses. J Exp Med 2008;205:35–42.
Nindl I, Gottschling M, Stockfleth E . Human papillomaviruses and non-melanoma skin cancer: basic virology and clinical manifestations. Dis Markers 2007;23:247–259.
Borgogna C, Zavattaro E, De Andrea M et al. Characterization of beta papillomavirus E4 expression in tumours from epidermodysplasia verruciformis patients and in experimental models. Virology 2012;423:195–204.
Dell’Oste V, Azzimonti B, De Andrea M et al. High beta-HPV DNA loads and strong seroreactivity are present in epidermodysplasia verruciformis. J Invest Dermatol 2009;129:1026–1034.
Neale RE, Weissenborn S, Abeni D et al. Human papillomavirus load in eyebrow hair follicles and risk of cutaneous squamous cell carcinoma. Cancer Epidemiol Biomarkers Prev 2013;22:719–727.
Proby CM, Harwood CA, Neale RE et al. A case–control study of betapapillomavirus infection and cutaneous squamous cell carcinoma in organ transplant recipients. Am J Transplant 2011;11:1498–1508.
Madeleine MM, Johnson LG, Daling JR et al. Cohort profile: the skin cancer after organ transplant study. Int J Epidemiol 2012 doi:10.1093/ije/dys179(e-pub ahead of print).
Tessari G, Girolomoni G . Nonmelanoma skin cancer in solid organ transplant recipients: update on epidemiology, risk factors, and management. Dermatol Surg 2012;38:1622–1630.
Mackintosh LJ, de Koning MNC, Quint WGV et al. Presence of beta human papillomaviruses in nonmelanoma skin cancer from organ transplant recipients and immunocompetent patients in the West of Scotland. Br J Dermatol 2009;161:56–62.
Farzan SF, Waterboer T, Gui J et al. Cutaneous alpha, beta and gamma human papillomaviruses in relation to squamous cell carcinoma of the skin: a population-based study. Int J Cancer 2013;133:1713–1720.
Karagas MR, Waterboer T, Li Z et al. Genus beta human papillomaviruses and incidence of basal cell and squamous cell carcinomas of skin: population based case–control study. BMJ 2010;341:c2986.
Plasmeijer EI, Neale RE, de Koning MNC et al. Persistence of betapapillomavirus infections as a risk factor for actinic keratoses, precursor to cutaneous squamous cell carcinoma. Cancer Res 2009;69:8926–8931.
Antonsson A, Waterboer T, Bouwes Bavinck JN et al. Longitudinal study of seroprevalence and serostability of 34 human papillomavirus types in European organ transplant recipients. Virology 2013;436:91–99.
Purdie KJ, Surentheran T, Sterling JC et al. Human papillomavirus gene expression in cutaneous squamous cell carcinomas from immunosuppressed and immunocompetent individuals. J Invest Dermatol 2005;125:98–107.
Griffin H, Wu Z, Marnane R et al. E4 antibodies facilitate detection and type-assignment of active HPV infection in cervical disease. PLoS One 2012;7:e49974.
Schaper ID, Marcuzzi GP, Weissenborn SJ et al. Development of skin tumors in mice transgenic for early genes of human papillomavirus type 8. Cancer Res 2005;65:1394–1400.
De Andrea M, Rittà M, Landini MM et al. Keratinocyte-specific stat3 heterozygosity impairs development of skin tumors in human papillomavirus 8 transgenic mice. Cancer Res 2010;70:7938–7948.
De Koning M, Quint W, Struijk L et al. Evaluation of a novel highly sensitive, broad-spectrum PCR-reverse hybridization assay for detection and identification of beta-papillomavirus DNA. J Clin Microbiol 2006;44:1792–1800.
Peh WL, Doorbar J . Detection of papillomavirus proteins and DNA in paraffin-embedded tissue sections. Methods Mol Med 2005;119:49–59.
Doorbar J . The papillomavirus life cycle. J Clin Virol 2005;32 (Suppl 1):S7–S15.
Doorbar J . Papillomavirus life cycle organization and biomarker selection. Dis Markers 2007;23:297–313.
Ko CJ, Iftner T, Barr RJ et al. Changes of epidermodysplasia verruciformis in benign skin lesions: the EV acanthoma. J Cutan Pathol 2007;34:44–48.
Leiding JW, Holland SM . Warts and all: human papillomavirus in primary immunodeficiencies. J Allergy Clin Immunol 2012;130:1030–1048.
Feltkamp MCW, de Koning MNC, Bavinck JNB et al. Betapapillomaviruses: innocent bystanders or causes of skin cancer. J Clin Virol 2008;43:353–360.
Weissenborn SJ, Nindl I, Purdie K et al. Human papillomavirus-DNA loads in actinic keratoses exceed those in non-melanoma skin cancers. J Invest Dermatol 2005;125:93–97.
Ganzenmueller T, Yakushko Y, Kluba J et al. Next-generation sequencing fails to identify human virus sequences in cutaneous squamous cell carcinoma. Int J Cancer J Int Cancer 2012;131:E1173–E1179.
Arron ST, Ruby JG, Dybbro E et al. Transcriptome sequencing demonstrates that human papillomavirus is not active in cutaneous squamous cell carcinoma. J Invest Dermatol 2011;131:1745–1753.
Wallace NA, Robinson K, Howie HL et al. HPV 5 and 8 E6 abrogate ATR activity resulting in increased persistence of UVB induced DNA damage. PLoS Pathogen 2012;8:e1002807.
Pfister H . Chapter 8. Human papillomavirus and skin cancer. J Natl Cancer Inst Monogr 2003;52–56.
Schiller JT, Buck CB . Cutaneous squamous cell carcinoma: a smoking gun but still no suspects. J Invest Dermatol 2011;131:1595–1596.
Acknowledgements
We gratefully acknowledge ‘Fondazione Banca Popolare di Novara per il territorio’ for their contribution in purchasing the digital scanner Pannoramic MIDI, and ‘Stichting Pathologie Onderzoek en Ontwikkeling’ for supporting the HPV genotyping.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Modern Pathology website
Supplementary information
Rights and permissions
About this article
Cite this article
Borgogna, C., Lanfredini, S., Peretti, A. et al. Improved detection reveals active β-papillomavirus infection in skin lesions from kidney transplant recipients. Mod Pathol 27, 1101–1115 (2014). https://doi.org/10.1038/modpathol.2013.240
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2013.240