Abstract
Extracapsular extension in squamous cell carcinoma nodal metastases usually predicts worse outcome. However, there are no standard histologic grading criteria for extracapsular extension, and there have been few studies on oropharyngeal squamous cell carcinoma alone. We studied the extent of extracapsular extension utilizing a novel grading system and correlated grades with outcomes while controlling for p16 status. A cohort of surgically treated oropharyngeal squamous cell carcinoma cases were reviewed and metastases graded as 0 (within substance of node), 1 (filling subcapsular sinus with thickened capsule/pseudocapsule, but no irregular peripheral extension), 2 (≤1 mm beyond capsule), 3 (>1 mm beyond capsule), or 4 (no residual nodal tissue or architecture; ‘soft tissue metastasis’). There were 101 cases, for which p16 was positive in 90 (89%). Extracapsular extension grades did not correlate with nodal size (P=0.28) or p16 status (P=0.8). In follow up, 10 patients (10%) had disease recurrence with only 3 of 64 (5%) grade 0–3 cases and 7 of 37 (19%) with grade 4 recurring (P=0.04). Grade 4 extracapsular extension was associated with poorer survival (P<0.01). However, grade 4 extracapsular extension correlated with higher T-stage (P=0.02), and in multivariate analysis, was not significantly associated with poorer overall (P=0.14) disease-free (P=0.2), or disease-specific survival (P=0.09). The impact of extracapsular extension in nodal metastases is limited in oropharyngeal squamous cell carcinoma. Only extracapsular extension grade 4 associates with poorer outcomes, but not independently of T-stage and other variables.
Similar content being viewed by others
Main
In head and neck squamous cell carcinoma, extracapsular extension in nodal metastases is widely regarded as a poor prognostic indicator. However, the literature on this subject has some problems including heterogeneity of primary head and neck anatomic subsites studied, frequent lack of clear macroscopic or histologic criteria for what actually constitutes extracapsular extension,1, 2, 3, 4 and no accounting for newer prognostic biomarkers such as human papillomavirus (HPV). In addition, while there is agreement that extracapsular extension is important, there is no consensus on exactly what degree is most critical in terms of prognosis,2 and no standardization for what to report regarding extracapsular extension.
The association of extracapsular extension with poorer outcomes in head and neck squamous cell carcinoma was first recognized in the 1970's,5, 6 and numerous subsequent studies further confirmed this association.7, 8, 9, 10, 11, 12 Most studies analyzed numerous different anatomic subsites simply grouped together,10, 13, 14, 15, 16 whereas some were limited to a single subsite.1, 4, 5, 8, 12, 17, 18 These latter studies have been primarily of the larynx (and/or hypopharynx)1, 5, 8, 12 or oral cavity,4, 17, 18, 19 with very few of oropharyngeal squamous cell carcinoma alone.14, 20, 21 These latter studies largely have not controlled for tumor HPV status.
The presence or absence of extracapsular extension in these studies has been predominantly listed as ‘yes’ or ‘no’, with no (or little more than a minimal) description and without any quantitation.4, 14, 21, 22, 23, 24 Most studies have utilized microscopy/histology, but most simply in a binary fashion as yes or no.4, 5 Still fewer have actually described their histologic criteria, and further, just a handful of studies have quantified or graded the extracapsular extension.1, 16, 17, 20 These studies have primarily found that the extent of extracapsular extension is of little or no importance, but rather that binary classification as ‘present’ or ‘absent’ is best. However, a few studies have separated out the so-called ‘soft tissue metastases’ or ‘soft tissue deposits’, these being masses of carcinoma in the neck soft tissue without obvious residual lymph node. When large, these are thought to be completely obliterated lymph nodes where tumor has simply overgrown them, making them essentially the most extreme manifestation of tumor extracapsular extension. When small, they may be lymphatic emboli of tumor that then grow out of the vessel into the surrounding tissue.25 Some studies have correlated their presence with worse outcomes, even beyond those with simple extracapsular extension.3, 15
Oropharyngeal squamous cell carcinoma is increasingly recognized as distinct among head and neck squamous cell carcinomas because of the association with high risk HPV. It has different demographics, a characteristic molecular profile, and a distinctly better prognosis.26, 27, 28, 29 At the molecular level, HPV-positive squamous cell carcinomas almost always overexpress p16, which is uncommon in HPV-negative squamous cell carcinomas.27, 30 These tumors are associated with better patient survival, despite a tendency to present with lymph node metastases.26, 27, 30, 31, 32, 33
Oropharyngeal squamous cell carcinoma has extremely high rates of cervical nodal metastasis.24, 34 As few studies have addressed extracapsular extension in just oropharyngeal squamous cell carcinoma, and these have also not clearly defined what constitutes extracapsular extension,21, 22, 23 we sought to do so utilizing a novel extracapsular extension grading system applied to a cohort of surgically treated patients for whom HPV status (via p16 immunohistochemistry) was known. We correlated extracapsular extension grades with clinical and pathological features and patient outcomes.
Materials and methods
After approval was obtained from the Washington University Human Research Protection Office (HRPO), cases of oropharyngeal squamous cell carcinoma treated from 1997–2007 were identified from HRPO-approved clinical databases from the divisions of Radiation Oncology and Otolaryngology Head and Neck Surgery, and a large study database was created.30 The slides from all cases had been reviewed by a single study pathologist (JSL), and the diagnosis of squamous cell carcinoma confirmed. Patients who underwent primary surgical management with tumor resection and neck dissections, and for whom nodal metastases were present, were selected. None of the cases were recurrences and none received any preoperative radiation or chemotherapy. Over this time period, the gross examination and sectioning of neck dissection specimens consisted of submitting one section per lymph node. This entailed only partial sampling the nodes, without necessarily submitting the entire lymph node (except for small ones, for example, 1 cm or less). For large masses, only one section was taken, this being targeted to show the grossly most concerning area for extracapsular extension at the periphery of the mass. Because their clinical behavior and survival are somewhat variable (as is their relationship with HPV), the uncommon histologic variants of squamous cell carcinoma such as undifferentiated, basaloid, spindle cell, papillary, and adenosquamous carcinoma were excluded from this study.
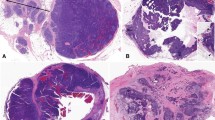
Nodal metastases for the oropharyngeal squamous cell carcinoma cases were reviewed by both study pathologists (JSL and DHC) without knowledge of the clinical outcomes and were graded for the highest degree of extracapsular extension using the following novel grading system (Figures 1 and 2: grade 0—tumor within substance of lymph node so surrounded by a rim of lymphoid tissue or tumor in subcapsular sinus without associated thickening of the capsul), grade 1—tumor filling sub-capsular sinus with thickened capsule, but no irregular edge or obvious extension of tumor beyond the capsule, grade 2—tumor extending less than or equal to 1 mm beyond the capsule, grade 3—tumor extending more than 1 mm beyond the capsule, and grade 4—masses of tumor with no residual nodal tissue or architecture such as discrete lymphoid tissue with germinal centers or a subcapsular sinus. For grades 2 and 3, the distance beyond the capsule was measured visually, or with use of a dotting pen and ruler for cases that were very near the 1 mm cutoff. The outer border of the capsule was used for measurement when clear, and in occasional cases, this had to be visually estimated. For grade 4, we included any size of deposit, large or small, that was discrete and without residual nodal architecture. Disagreements in classification between the two reviewers were resolved by consensus review.
Extracapsular extension histologic features. (a) Grade 1 with tumor expanding the lymph node but confined by a thick capsule/pseudocapsule (designated by *), with which it has a smooth interface. (b) Grade 4 (or ‘soft tissue metastasis’) with tumor growing extensively and irregularly into adipose tissue without residual lymph node identifiable. (Hematoxylin and eosin staining; a=40 × magnification; b=20 × magnification).
Cases were only included if all nodal metastasis slides could be reviewed, and cases where there was prior neck surgical intervention (prior incisional or excisional biopsy) were included only if all of the slides were available for review and could be clearly classified. Sizes of the largest lymph nodes were assessed utilizing the gross examination or, if not clear, or if not large enough for gross detection, were measured from the glass slides.
This study was performed completely independently of the clinical management of the patients. Results of this review were not available to or known by the treating clinicians at the time of their treatment of the patients or any time during the patients' course.
Immunohistochemistry
Immunohistochemistry was previously performed for p16 on the oropharyngeal squamous cell carcinoma cases on representative 4 μm sections cut from formalin-fixed, paraffin-embedded tissue blocks using a monoclonal antibody to p16 (MTM Laboratories; monoclonal; 1:1 dilution) on a Ventana Benchmark automated immunostainer (Ventana Medical Systems, Tucson, AZ, USA) according to standard protocols, with appropriate positive controls. Antigen retrieval, standard on the machine, utilized the Ventana CC1, EDTA-Tris, pH 8.0 solution. Staining was graded in a quartile manner: 0=negative; 1+=1 to 25% of cells positive; 2+=26 to 50%; 3+=51 to 75%; 4+=76 to 100%. For analysis, however, cases were divided into positive (1+ to 4+) or negative (0).
Statistics
Clinical follow-up information was obtained from detailed clinician databases (WLT and BHH). For statistical analysis, the date of surgery was considered the start of survival time. Overall survival ended either when a patient was dead due to any cause or at the date of the last known follow-up. Either the date of first recurrence, death, or last known disease-free status was considered the end of disease free survival. If patients died with evidence of persistent or recurrent squamous cell carcinoma, the date of death was used to determine disease-specific survival. All of the survival times and proportions were determined based on Kaplan–Meier estimates. Log-rank tests were used to compare survival intervals upon covariates' effects. Multivariate analysis, eg, proportional hazard regression model, was also employed to study multiple variables of interest and their adjusted influences. To examine hypothetical associations in categorical data, χ2-tests or Fisher's tests were used when appropriate. For continuous variables, student's t-tests or non-parametric rank tests were used, based on distribution normality. We did not make adjustments for multiple comparisons, as the study hypotheses were specifically indicated. All of the tests were two-sided, and results were considered significant if P-values were less than 0.05. SAS 9.1 was used for all major statistical calculations (SAS Institute, Cary, NC, USA).
Results
In total, there were 101 cases. Patient demographics are presented in Table 1. There were 13 extracapsular extension grade 0 cases, 25 grade 1, 7 grade 2, 19 grade 3, and 37 grade 4 cases. p16 was positive in 90 (89%) and negative in 11 (11%) cases, making this essentially a p16-positive cohort. Although we considered any degree of p16 staining positive, almost all (88/90 or 98%) of the p16 positive cases were 4+ (75% or more cells positive). The size of the largest metastasis ranged from 0.1 to 6.8 cm (average 3.3). Grade of extracapsular extension did not correlate with size of the largest metastasis (Table 2 and Figure 3) nor with tumor p16 status. Specifically, for extracapsular extension 0 versus 1–4, extracapsular extension 0 or 1 versus 2–4, and extracapsular extension 0–3 versus 4, there were no statistically significant correlations with p16 status (P=0.53, P=1.0, and P=0.20, respectively). T-stage, as T1 or T2 versus T3 or T4, correlated with extracapsular extension grade 4 (P=0.025).
Postoperative intensity-modulated radiation therapy was given to 100 of the 101 patients (99%), and 44 patients (47.8%) received postoperative chemotherapy (Table 3). Chemotherapy was given more frequently in patients with grade 4 extracapsular extension than for patients with other extracapsular extension grades (Table 3), although this was of borderline statistical significance (P=0.052). Chemotherapy was given more frequently in the extracapsular extension grade 2–4 group than for extracapsular extension grade 0–1, but again, this was just statistically significant (P=0.05). However, while chemotherapy was given in slightly more patients with extracapsular extension grade 4 than for extracapsular extension grades 2 and 3 combined, this difference was not statistically significant (P=0.43).
Average follow-up was 38.8 months (range 1.8–102). Twenty-five of the 101 patients (24%) died in the follow-up period. Ten of the 101 patients (10%) suffered disease recurrence of any form (Table 4). For extracapsular extension grade 0, one patient (8%) recurred, for grade 1, 0 recurred (0%), for grade 2, one recurred (14%), for grade 3, one recurred (5%), and for grade 4, seven recurred (19%). The difference, when considered as extracapsular extension grades 0–1 versus grades 2–4, was not statistically significant (P=0.096), but, when considered as extracapsular extension grade 0–3 versus grade 4, it was statistically significant (P=0.035). Of the seven patients with grade 4 extracapsular extension that recurred, six (86%) had distant metastasis, and six of these seven (86%) were p16 positive. Considered in the opposite manner, eight patients developed distant metastases, and six of them (75%) had grade 4 extracapsular extension. There was no difference in recurrence rates between grades 0, 1, 2, or 3 (P=0.45). Considering extracapsular extension grades 2, 3, and 4 as ‘true’ extracapsular extension, 63 of 101 patients (62%) had this, but only nine of them (14%) suffered disease recurrence.
Univariate Survival Analysis
Univariate survival analysis results are presented in Table 5. Grade 4 extracapsular extension correlated strongly with poorer overall, disease-free, and disease-specific survival (Figure 4; P=0.001, P=0.0025, and P=0.0013, respectively). The overall 3-year survival rate for patients with extracapsular extension grades 0 through 3 was 97% (95% CI 82.8–99.6), whereas for those with extracapsular extension grade 4, it was 61.0% (95% CI 39.0–77.2). There was no difference in survival between patients with extracapsular extension grades 0 and 1, nor between those with grades 0 and 1–3. Among the other variables, negative p16 status correlated with poorer overall, disease-free, and disease-specific survival (P=0.024, P=0.039, and P=0.068, respectively). T-stage (considered as T1 or T2 versus T3 or T4) also correlated with poorer overall, disease-free, and disease-specific survival (P=0.001, P=0.003, and P=0.001, respectively). The remaining variables, including patient age, gender, largest lymph node size, N-stage (as N1 versus N2/N3 and N1/N2a versus N2b/N2c/N3), chemotherapy treatment, and resection margin status showed no statistically significant correlation with worse survival.
Multivariate Survival Analysis
Controlling for p16 status, T-stage, and overall stage, grade 4 extracapsular extension showed a trend towards poorer disease-specific survival, but this was not statistically significant (P=0.09). Grade 4 extracapsular extension did not correlate with poorer overall or disease-free survival (P=0.14 and P=0.2, respectively), whereas in multivariate analysis, T-stage still correlated with worse survival, being statistically significantly correlated with disease-free survival (P=0.044), and showing trends towards worse overall and disease-free survival (P=0.099 and P=0.16, respectively).
Discussion
Extracapsular extension in head and neck squamous cell carcinoma nodal metastases is very well established as an adverse prognostic factor. However, it is used somewhat dogmatically, and this hides many of the problems with the existing literature on the subject, including poor definitions of what histologically constitutes extracapsular extension and lack of many studies focusing on single anatomic subsites. This latter problem potentially masks differences for those tumor types with a unique biology within the larger umbrella of head and neck squamous cell carcinoma.
Most studies on extracapsular extension have either not included oropharynx cases or have included them combined with other anatomic subsites. The studies that have been limited to oropharynx have had conflicting results. Some have shown a significant adverse prognosis for patients with extracapsular extension in their lymph node metastases,21 but interestingly, some have shown no difference.22, 23 Very few have controlled for HPV status, even though we know that most squamous cell carcinoma of the oropharynx are HPV-related. We studied a sizeable cohort of surgically treated oropharyngeal squamous cell carcinoma patients to specifically ask the question ‘what is the significance of extracapsular extension’, while controlling for HPV (via p16 immunohistochemistry) and by applying a novel, clearly defined grading system.
A number of our findings for this oropharyngeal cohort run contrary to the general thinking on extracapsular extension. First, the size of the lymph node metastases did not correlate with presence or absence of extracapsular extension. Oropharyngeal squamous cell carcinoma has frequent and early metastasis, very often with large, rounded, and pushing metastases. The metastases were frequently grade 1, which in our grading system is where tumor expands the lymph node and induces a thick, peripheral capsule or pseudocapsule, but without tumor actually growing beyond the smooth periphery. We found that this type of nodal metastasis is clinically equivalent to nodal metastases where tumor is completely surrounded by lymphoid tissue and/or involves the subcapsular sinus without a thickened capsule. We also found that even some forms of bonafide extracapsular extension (grades 2 and 3 in our system) had no adverse effect on outcomes. Only one patient (out of seven) with grade 2 extracapsular extension and one (out of 19) with grade 3 extracapsular extension developed recurrent disease.
We did find that grade 4 extracapsular extension, where there is total obliteration of the node, with no remaining lymphoid tissue/germinal centers, and no obvious residual capsule or subcapsular sinus, correlates with disease recurrence, but not very strongly. Seven of the 37 patients (19%) with grade 4 extracapsular extension recurred, whereas only three of the remaining 64 patients (5%) had recurrence. It is important to note, though, that grade 4 extracapsular extension correlated strongly with higher T-stage (P=0.025), and T-stage has repeatedly been shown to one of the few major variables that strongly predict for worse outcome in HPV-related/p16 positive oropharyngeal squamous cell carcinoma.22, 26, 30, 34 It may be that grade 4 extracapsular extension is simply correlated with larger primary tumors, but not independently correlated with poorer outcome. Whether or not this is the explanation, our data does show that grade 4 extracapsular extension puts patients in a group who are more likely to develop recurrent disease, but this rate only increases from 10% (rate of the entire cohort) to 19% (rate for just the grade 4 extracapsular extension cohort). What may be more significant is what the lack of (or negative predictive value of) grade 4 extracapsular extension says about patients' clinical outcomes. The patients that had either no extracapsular extension (grades 0 or 1) or even bonafide extracapsular extension, but still with residual nodal architecture present (grades 2 or 3), had a very low rate of recurrent disease in our study (3/64 or 5%).
A limitation of our study is that it was retrospective. Patients were treated with partial regard to extracapsular extension based on pathology results for the patients in ‘real time’, which, although not systematic or specific criterion-based, would still be expected to correlate with our extracapsular extension grades. One could argue that the lack of prediction of poorer patient outcome for extracapsular extension in this cohort is because patients who had it were treated more aggressively. With regard to radiation therapy, as 99% of our study patients received it, this could not explain our findings. Chemotherapy rates, however, were different by extracapsular extension grade (Table 3), being used in approximately 50% of our patients, and being more commonly used in extracapsular extension grades 2, 3, and 4 than 0 or 1. However, the efficacy of postoperative chemotherapy in addition to radiation for oropharyngeal squamous cell carcinoma is somewhat controversial, having not been evaluated adequately in the HPV/p16 era. Our study also was a mixture of p16 positive and negative cases. Ideally, we would have either limited to p16 positive only or had a better distribution of p16 positive and negative cases. But as the group was 90% p16 positive tumors, one can reasonably argue that it is essentially equivalent to a p16 positive cohort.
Patients with oropharyngeal squamous cell carcinoma who are treated either by primary surgery or primary radiochemotherapy have been shown to have excellent disease-specific outcomes, and cohort certainly demonstrates this as well, despite it consisting only of patients with nodal metastasis at presentation, and despite more than 50% of patients showing extracapsular extension, at least by any current definition of it. Our data strongly suggests that assuming extracapsular extension is a negative prognosticator for decisions on postoperative radiation and/or chemotherapy in oropharyngeal squamous cell carcinoma in the traditional manner done for other head and neck squamous cell carcinoma is possibly resulting in overtreatment. Some of these patients may not actually need postoperative therapy. As primary surgical management for oropharyngeal squamous cell carcinoma is becoming more prevalent with the advent of transoral laser microsurgery and transoral robotic surgery, there is real need for further study of predictive parameters in these tumors, so that they are not simply considered equivalent to traditional squamous cell carcinoma.
In summary, extracapsular extension in surgically treated oropharyngeal squamous cell carcinoma is independent of the size of the metastasis and is a poor predictor of disease recurrence. Only extracapsular extension grade 4, regardless of p16 status, put patients at higher risk of recurrence. However, this correlation was not statistically significant when controlling for tumor T-stage. Given the excellent prognosis of surgically treated oropharyngeal squamous cell carcinoma even in the face of nodal metastases with extracapsular extension (by any current definition of it), this latter feature should perhaps be reconsidered as a strong indication for the use of postoperative radiation and/or chemotherapy in such patients.
References
Brasilino de Carvalho M . Quantitative analysis of the extent of extracapsular invasion and its prognostic significance: a prospective study of 170 cases of carcinoma of the larynx and hypopharynx. Head Neck 1998;20:16–21.
Ferlito A, Rinaldo A, Devaney KO, et al. Prognostic significance of microscopic and macroscopic extracapsular spread from metastatic tumor in the cervical lymph nodes. Oral Oncol 2002;38:747–751.
Jose J, Coatesworth AP, Johnston C, et al. Cervical node metastases in squamous cell carcinoma of the upper aerodigestive tract: the significance of extracapsular spread and soft tissue deposits. Head Neck 2003;25:451–456.
Myers JN, Greenberg JS, Mo V, et al. Extracapsular spread. A significant predictor of treatment failure in patients with squamous cell carcinoma of the tongue. Cancer 2001;92:3030–3036.
Bennett SH, Futrell JW, Roth JA, et al. Prognostic significance of histologic host response in cancer of the larynx or hypopharynx. Cancer 1971;28:1255–1265.
Zoller M, Goodman ML, Cummings CW . Guidelines for prognosis in head and neck cancer with nodal metastasis. Laryngoscope 1978;88:135–140.
Vaidya AM, Petruzzelli GJ, Clark J, et al. Patterns of spread in recurrent head and neck squamous cell carcinoma. Otolaryngol Head Neck Surg 2001;125:393–396.
Hirabayashi H, Koshii K, Uno K, et al. Extracapsular spread of squamous cell carcinoma in neck lymph nodes: prognostic factor of laryngeal cancer. Laryngoscope 1991;10:502–506.
Johnson JT, Barnes EL, Myers EN, et al. The extracapsular spread of tumors in cervical node metastasis. Arch Otolaryngol 1981;107:725–729.
Johnson JT, Myers EN, Bedetti CD, et al. Cervical lymph node metastases. Incidence and implications of extracapsular carcinoma. Arch Otolaryngol 1985;111:534–537.
Snow GB, Annyas AA, van Slooten EA, et al. Prognostic factors of neck node metastasis. Clin Otolaryngol Allied Sci 1982;7:185–192.
Snyderman NL, Johnson JT, Schramm Jr VL, et al. Extracapsular spread of carcinoma in cervical lymph nodes. Impact upon survival in patients with carcinoma of the supraglottic larynx. Cancer 1985;56:1597–1599.
Moor JW, Jose J, Johnston C, et al. Upper aerodigestive tract squamous cell carcinoma: distribution of extracapsular spread and soft tissue deposits in the neck. Acta Otolaryngol 2004;124:97–101.
Klozar J, Kratochvil V, Salakova M, et al. HPV status and regional metastasis in the prognosis of oral and oropharyngeal cancer. Eur Arch Otorhinolaryngol 2008;265:S75–S82.
Jose J, Moor JW, Coatesworth AP, et al. Soft tissue deposits in neck dissections of patients with head and neck squamous cell carcinoma: prospective analysis of prevalence, survival, and its implications. Arch Otolaryngol Head Neck Surg 2004;130:157–160.
Ghadjar P, Schreiber-Facklam H, Grater R, et al. Quantitative analysis of extracapsular extension of metastatic lymph nodes and its significance in radiotherapy planning in head and neck squamous cell carcinoma. Int J Radiat Oncol Biol Phys 2010;76:1127–1132.
Greenberg JS, Fowler R, Gomez J, et al. Extent of extracapsular spread: a critical prognosticator in oral tongue cancer. Cancer 2003;97:1464–1470.
Woolgar JA, Rogers SN, Lowe D, et al. Cervical lymph node metastasis in oral cancer: the importance of even microscopic extracapsular spread. Oral Oncol 2003;39:130–137.
Shaw RJ, Lowe D, Woolgar JA, et al. Extracapsular spread in oral squamous cell carcinoma. Head Neck 2010;32:714–722.
Wenzel S, Sagowski C, Kehrl W, et al. The prognostic impact of metastatic pattern of lymph nodes in patients with oral and oropharyngeal squamous cell carcinomas. Eur Arch Otorhinolaryngol 2004;261:270–275.
Shimizu K, Inoue H, Saitoh M, et al. Distribution and impact of lymph node metastases in oropharyngeal cancer. Acta Otolaryngol 2006;126:872–877.
Rich JT, Milov S, Lewis Jr JS, et al. Transoral laser microsurgery (TLM) +/− adjuvant therapy for advanced stage oropharyngeal cancer: outcomes and prognostic factors. Laryngoscope 2009;119:1709–1719.
Preuss SF, Dinh V, Klussmann JP, et al. Outcome of multimodal treatment for oropharyngeal carcinoma: a single institution experience. Oral Oncol 2007;43:402–407.
Woolgar JA . The topography of cervical lymph node metastases revisited: the histological findings in 526 sides of neck dissection from 439 previously untreated patients. Int J Oral Maxillofac Surg 2007;36:219–225.
Coatesworth AP, MacLennan K . Squamous cell carcinoma of the upper aerodigestive tract: the prevalence of microscopic extracapsular spread and soft tissue deposits in the clinically N0 neck. Head Neck 2002;24:258–261.
Chernock RD, El-Mofty SK, Thorstad WL, et al. HPV-related nonkeratinizing squamous cell carcinoma of the oropharynx: utility of microscopic features in predicting patient outcome. Head Neck Pathol 2009;3:186–194.
Adelstein DJ, Ridge JA, Gillison ML, et al. Head and neck squamous cell cancer and the human papillomavirus: summary of a National Cancer Institute State of the Science Meeting, November 9-10, 2008, Washington, D.C.. Head Neck 2009;31:1393–1422.
Fakhry C, Westra WH, Li S, et al. Improved survival of patients with human papillomavirus-positive head and neck squamous cell carcinoma in a prospective clinical trial. J Natl Cancer Inst 2008;100:261–269.
Ragin CC, Taioli E . Survival of squamous cell carcinoma of the head and neck in relation to human papillomavirus infection: review and meta-analysis. Int J Cancer 2007;121:1813–1820.
Lewis Jr JS, Thorstad WL, Chernock RD, et al. p16 positive oropharyngeal squamous cell carcinoma: an entity with a favorable prognosis regardless of tumor HPV status. Am J Surg Pathol 2010;34:1088–1096.
Klussmann JP, Gultekin E, Weissenborn SJ, et al. Expression of p16 protein identifies a distinct entity of tonsillar carcinomas associated with human papillomavirus. Am J Pathol 2003;162:747–753.
Nichols AC, Faquin WC, Westra WH, et al. HPV-16 infection predicts treatment outcome in oropharyngeal squamous cell carcinoma. Otolaryngol Head Neck Surg 2009;140:228–234.
Weinberger PM, Yu Z, Haffty BG, et al. Prognostic significance of p16 protein levels in oropharyngeal squamous cell cancer. Clin Cancer Res 2004;10:5684–5691.
Fischer CA, Zlobec I, Green E, et al. Is the improved prognosis of p16 positive oropharyngeal squamous cell carcinoma dependent of the treatment modality? Int J Cancer 2010;126:1256–1262.
Acknowledgements
Special thanks to Mary Madden and Sue Pagano for their help in managing the slides and blocks on these cases and for help with data entry. We also acknowledge the support of the Biostatistics Core, Siteman Comprehensive Cancer Center and NCI Cancer Center Support Grant P30 CA091842.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Lewis, J., Carpenter, D., Thorstad, W. et al. Extracapsular extension is a poor predictor of disease recurrence in surgically treated oropharyngeal squamous cell carcinoma. Mod Pathol 24, 1413–1420 (2011). https://doi.org/10.1038/modpathol.2011.105
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2011.105
Keywords
This article is cited by
-
Relationship Between Worst Pattern of Invasion and Extranodal Extension in Oral Tongue Squamous Cell Carcinomas
Head and Neck Pathology (2023)
-
Prognostic impact of extranodal extension (ENE) in surgically managed treatment-naive HPV-positive oropharyngeal squamous cell carcinoma with nodal metastasis
Modern Pathology (2022)
-
Inter- and Intrarater Reliability and Agreement Among Danish Head and Neck Pathologists Assessing Extranodal Extension in Lymph Node Metastases from Oropharyngeal Squamous Cell Carcinomas
Head and Neck Pathology (2022)
-
Risk Stratification of HPV-Associated Oropharyngeal Squamous Cell Carcinoma: Are All Tumors Created Equally?
Current Otorhinolaryngology Reports (2022)
-
Tumour Cell Anaplasia and Multinucleation as Prognosticators in Oropharyngeal Squamous Cell Carcinoma
Head and Neck Pathology (2020)