Abstract
Interleukin (IL)-4 has critical roles in allergic disorders, including food hypersensitivity. The direct effects of the cytokine on the survival and function of mast cells, the key effectors of food anaphylaxis, have not been established. In this study, we demonstrate that IL-4 induces a marked intestinal mastocytosis in mice. This phenotype is reproduced in animals expressing Il4rαF709, an activating variant of the IL-4 receptor α-chain (IL-4Rα). Il4rαF709 mice exhibit enhanced anaphylactic reactions but unaltered physiological responses to vasoactive mediators. IL-4 induces Bcl-2 and Bcl-XL and enhances survival and stimulates proliferation in cultured bone marrow–derived mast cells (BMMC). These effects are STAT6 (signal transducer and activator of transcription factor 6)-dependent and are amplified in Il4rαF709 BMMC. In competitive bone marrow chimeras, Il4rαF709 mast cells display a substantial competitive advantage over wild-type mast cells, which, in turn, prevail over IL-4Rα−/− mast cells in populating the intestine, establishing a cell-intrinsic effect of IL-4 in intestinal mast cell homeostasis. Our results demonstrate that IL-4-signaling is a key determinant of mast cell expansion in food allergy.
Similar content being viewed by others
Introduction
Hospital visits for food anaphylaxis have doubled in the last decade.1, 2 Mast cells activated by allergen-specific immunoglobulin E (IgE) antibodies drive these reactions, releasing preformed and newly synthesized mediators of hypersensitivity.3, 4, 5, 6 These trigger a range of local physiological responses in the intestine, including mucus production, intestinal smooth muscle contraction, and solute secretion as well as systemic effects, including vasodilation and plasma extravasation, leading to hypovolemia, vascular collapse, and shock. In animal models, the density of intestinal mast cells correlates with severity of food allergen–induced anaphylaxis.5 There is considerable evidence that in addition to serving as effector cells of allergy, mast cells participate in the afferent limb of immune responses by facilitating activation of antigen-presenting cells and exerting a range of effects on regulatory T cells and integrity of mucosal barriers.7, 8, 9 Defining the factors that regulate intestinal mast cell expansion and effector functions in the intestine is of great importance and might guide the development of novel strategies for the regulation of immune responses to foods. In the current study, we focus on the direct cell-intrinsic effects of interleukin (IL)-4 receptor signals on intestinal mast cells.
IL-4, the hallmark cytokine of allergic responses, is produced primarily by CD4+ T helper type 2 (Th2) cells but can also come from mast cells and basophils. The cytokine has a wide range of immunological functions, including induction and maintenance of adaptive allergic immune responses by directing Th2 cell differentiation and triggering Ig class switching to IgE in B cells.10 IL-13, a cytokine with overlapping functions, is often considered to act primarily on tissues. In the context of food allergy, it has been shown to markedly perturb gut barrier function, disrupting the tight junctions between intestinal epithelial cells and stimulating mucus production.11, 12, 13 It is of particular interest for studies on food allergen–induced anaphylaxis that IL-4 and IL-13 have been shown to increase the sensitivity of target tissues to vasoactive mediators of anaphylaxis, leading to dramatically enhanced peripheral vasodilation and core body temperature decreases during anaphylaxis in IL-4-primed animals.14
In addition to stimulating adaptive immune responses to allergens, IL-4 drives innate effector mechanisms, enhancing the production of eosinophils and basophils.15, 16 It has long been known that the expansion of mucosal mast cells in parasite-infested mice is completely T cell dependent, suggesting a role for a Th2 cytokine in mast cell growth.17, 18, 19, 20, 21 When Arai and colleagues20 used expression cloning to identify mast cell–inducing activities in supernatants of a Con A-stimulated T-cell line, they found not only IL-3, the prototypical mast cell–inducing cytokine, but also IL-4. Subsequent investigations have revealed significant complexity with respect to determining physiological roles of IL-4 in mast cell homeostasis. Several investigators have approached the issue by testing the effects of exogenous IL-4 on cultured mast cells prepared from hematopoietic progenitors using stem cell factor (SCF) and IL-3. Although IL-4 has been shown to augment both mouse and human mast cell growth under such conditions,22, 23, 24 it can also have opposing effects, especially when added early on in these cultures.25, 26, 27 In addition, IL-4 has been shown to induce expression of FcɛRI, increase granule content, and accelerate growth of both mature mast cells and committed mast cell progenitors.18, 22, 28, 29, 30
The recent development of mice harboring activating mutations of the IL-4 receptor α-chain (IL-4Rα) has provided a very useful new tool for the evaluation of effects of increased IL-4 signaling at the level of the mast cell. We have previously shown that knock-in mice harboring such IL-4Rα signaling variants exhibit exacerbated allergic responses.31, 32, 33, 34 In Il4rαF709 mice, targeted disruption of the immunoreceptor tyrosine-based inhibitory motif (ITIM) of IL-4Rα by conversion of the tyrosine residue at amino acid 709 into phenylalanine (Y709→F709) enhances signaling in response to IL-4 and IL-13.3, 32 Oral tolerance is disrupted, and enteral exposure to allergen induces strong food-specific IgE responses, intestinal mastocytosis, and intense systemic anaphylaxis upon allergen challenge.3 This phenotype, particularly the fact that allergen sensitization can be achieved via the gut alone without a requirement for previous intraperitoneal priming with antigen and adjuvant, recapitulates key features of human food allergy. Given the strong correlation between mast cell expansion and anaphylactic food sensitivity in Il4rαF709 mice, we chose to test whether increased mast cell expansion is driven by IL-4 and whether mast cells themselves are critical for the expression of anaphylaxis. We considered the alternative hypothesis that increased end organ sensitivity to mediators of anaphylaxis might be to blame for the increased sensitivity of these mice. In addition, we took advantage of cultured mast cells derived from mice to ask whether enhanced IL-4 signaling affects growth and/or survival. The availability of mice with enhanced (Il4rαF709) or absent (IL-4Rα−/−) IL-4R function allowed us to construct mixed–bone marrow chimeras to directly analyze in an in vivo setting the cell-intrinsic advantages or disadvantages of IL-4 signals in mast cells. Taken together, our findings demonstrate that IL-4 acts on mast cells to drive their expansion and that this expansion is critical for the manifestations of anaphylaxis upon food allergen challenge.
Results
IL-4 receptor signaling tone regulates intestinal mast cell burden
Intestinal mast cell numbers correlate with symptom severity in several mouse models of food allergy,4, 5 and we previously observed that orally sensitized Il4rαF709 mice develop a robust expansion of mast cells, even extending into the villi.3 This suggested that IL-4R signaling might directly or indirectly promote mast cell growth in vivo. We therefore investigated whether either exogenous administration of IL-4 immune complexes or the mere presence of the Il4rαF709 variant itself would be sufficient to alter mast cell numbers. Examination of chloroacetate esterase–stained jejunal sections from wild-type mice treated with a week-long course of IL-4 immune complexes revealed a significant increment in mast cells (Figure 1a), consistent with the previous observations of Finkelman and colleagues.11 Similarly, Il4rαF709 mice had significantly increased mast cell numbers. The mast cell expansion in IL-4-treated wild-type and Il4rαF709 mice occurred predominantly in the lamina propria, although a few mast cells were also observed in the villi and intestinal epithelium. Flow cytometry was used to quantify mast cells (CD45+lin−c-Kit+IgE+) among intestinal leukocytes. Both relative frequencies and overall numbers of mast cells were increased more than threefold in Il4rαF709 mice relative to wild-type controls (Figure 1b). Again, administration of IL-4 to wild-type mice produced a similar mast cell expansion (Figure 1c). Enumeration of mast cells within the intestinal compartments corroborated our histological observations, with IL-4-treated and Il4rαF709 mice exhibiting the greatest increases in numbers of mast cells within the lamina propria fraction, with smaller but proportional increases in intra-epithelial mast cells (see Supplementary Figure S1 online). These findings provide evidence that IL-4-mediated signals lead to increased intestinal mast cell numbers in vivo. Additional analyses were performed to assess whether this IL-4 effect was exerted directly on the mast cells or via intermediate cellular or molecular inducers of mast cell expansion.
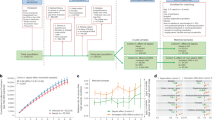
IL-4 drives intestinal mastocytosis. (a) Chloroacetate esterase staining for mast cells (red, examples highlighted by red arrows) in jejunal sections in wild-type, interleukin (IL)-4-treated, or Il4rαF709 mice. (b) Representative flow cytometry diagrams and summary data of small intestinal mast cells (c-Kit+IgE+lin−CD45+) from wild-type and Il4rαF709 mice, gating on live lin−CD45+ cells (n=5). (c) IL-4 treatment dramatically expands intestinal mast cells in wild-type mice. IL-4 was injected as a cytokine-antibody complex with 2 μg IL-4 and 10 μg anti-IL-4 intraperitoneally on days −1, −4, and −7. Statistical analysis by unpaired t test, two-tailed. Data are representative of at least three experiments. Mast cell frequencies are expressed as the fraction out of lin−CD45+ cells. Ig, immunoglobulin.
Enhanced IL-4 receptor signaling exacerbates passive systemic anaphylaxis in Il4rαF709 mice
Enterally sensitized Il4rαF709 mice, unlike their wild-type counterparts, develop intense and often lethal IgE-mediated systemic anaphylaxis upon allergen challenge.3 IL-4 receptors are expressed on many cell types, and the cytokine has pleiotropic effects, so we considered several alternative hypotheses for the strong responses of Il4rαF709 mice: (1) enhanced immune sensitization (Th2 responses and IgE production), (2) expansion of mast cells with an associated increase in the pool of mediators, or (3) increased sensitivity of target tissues to the effector molecules of anaphylaxis. With respect to the first hypothesis, we have previously shown that allergen-sensitized Il4rαF709 mice indeed exhibit stronger Th2 responses and higher IgE levels than wild-type controls, suggesting a contribution of enhanced immune sensitization to the anaphylaxis phenotype.3, 32 In order to determine whether additional factors independently contribute to the anaphylactic phenotype of these mice, we assessed their responses under controlled conditions of IgE sensitization using the model of passive systemic anaphylaxis. IgE−/− mice were used in these studies, providing us with host animals with no background IgE, permitting complete control over the level of sensitization, and eliminating any potential alterations in FcɛRI expression induced by differences in baseline IgE levels.3, 35 IgE−/− and Il4rαF709-IgE−/− were given anti-DNP (anti-2,4-dinitrophenol) IgE (SPE-7) and then challenged with DNP-BSA (bovine serum albumin; Figure 2). Core body temperature was measured as an indicator of vasodilation and shock. Passively sensitized Il4rαF709 mice exhibited significantly more intense reactions upon challenge than wild-type IgE−/− control mice. This was evidenced by a more than twofold greater loss of core body temperature and a markedly delayed recovery (Figure 2a). Every one of the Il4rαF709 mice rapidly developed diarrhea, a symptom that never occurred in wild-type mice (Figure 2b). Responding Il4rαF709 mice also exhibited greater release of the mouse mast cell protease (MMCP)-1 and IL-4 into the serum (Figure 2c,d). These findings demonstrate that, given identical levels of allergen-specific IgE, Il4rαF709 mice exhibit more intense responses than their wild-type counterparts, an observation which implicates mast cells and/or target tissue sensitivity to their mediators in the anaphylaxis phenotype of these animals.
Interleukin (IL)-4Rα-driven effects exacerbate anaphylaxis. (a) Il4rαF709 mice show an increased loss of temperature and limited recovery from anaphylaxis. Wild-type and Il4rαF709 mice lacking endogenous immunoglobulin E (IgE; IgE−/−) were subjected to IgE-mediated passive anaphylaxis, and core body temperatures were recorded to assess the severity of the response. Statistical analysis by two-way analysis of variance (ANOVA). (b) Il4rαF709 mice uniquely exhibit rapid-onset diarrhea during IgE-mediated passive anaphylaxis. P=0.0084 by log-rank test of Kaplan–Meier survival curves. (c) Serum release of mouse mast cell protease (MMCP-1) is greatly enhanced in Il4rαF709 mice following passive anaphylaxis. Statistical analysis by one-way ANOVA. (d) IL-4 release in Il4rαF709 mice is also enhanced following passive anaphylaxis. Statistical analysis by unpaired t test. Mice were injected retro-orbital (RO) with 20 μg IgE anti-DNP (anti-2,4-dinitrophenol; clone SPE-7) and challenged 16 h later with 0.5 mg DNP-BSA (bovine serum albumin) RO Data shown are from 4–7 mice per group and are representative of three experiments. *P<0.05, **P<0.01, ***P<0.0001 by Bonferroni post-test where indicated. Enhanced anaphylaxis in Il4rαF709 mice is not the result of altered vascular responsiveness. Wild-type and Il4rαF709 mice were injected RO with (e) histamine (1.25 mg), (f) serotonin (1 mg), or (g) leukotriene C4 (LTC4, 1 μg), and core body temperatures were recorded to assess the severity of the response. Data shown are from 3–5 mice per group.
Finkelman and colleagues14 have demonstrated that IL-4 alters vascular tissue sensitivity to the vasoactive mediators (e.g., histamine) that drive anaphylaxis, lowering the threshold for the induction of anaphylactic symptoms. We hypothesized, therefore, that Il4rαF709 mice might be more sensitive to mediators of anaphylaxis. Direct treatment of mice with histamine, however, induced comparable decreases of core body temperature in wild-type and Il4rαF709 mice (Figure 2e). Similarly, comparable responses were elicited by exogenous serotonin (Figure 2f) and leukotriene C4 (Figure 2g). Symptoms were also similar between mediator-treated wild-type and Il4rαF709 mice (data not shown). These results suggest that at physiological levels, IL-4 and IL-13 signaling do not significantly affect vascular sensitivity to these mediators and that target tissue sensitivity is not the key determinant of enhanced IgE-mediated anaphylaxis in Il4rαF709 mice. Taken together, our observations of increased mast cell numbers and enhanced physiological responses and elevated mast cell protease release in passive systemic anaphylaxis along with the absence of differences in responses to injected mast cell mediators strongly indicate that IL-4-driven mast cell expansion underlies the sensitivity of Il4rαF709 mice to systemic anaphylaxis.
IL-4 signals enhance growth, survival, FcɛRI levels, and anti-apoptotic gene expression in cultured mast cells.
The IL-4R α-chain triggers two major activating signaling cascades, one through phosphorylation and nuclear translocation of the transcription factor STAT6 and the other through Akt-PI3K (protein kinase B–phosphatidylinositol-3-kinase).31 The STAT6 pathway is initiated upon action of Jak (Janus kinase) kinases on the cytosolic immunoreceptor tyrosine-based activating motifs (ITAMs) of the IL-4Rα chain. IL-4Rα also exerts regulatory effects via its ITIM through recruitment of inhibitory phosphatases, including Src homology phosphatase-1. We previously demonstrated that disruption of the ITIM enhances signaling through both of these activating arms in T and B lymphocytes.32 In order to determine whether the mutation enhances IL-4Rα signaling in mast cells, we analyzed the responses of IL-4-stimulated wild-type or Il4rαF709 bone marrow–derived mast cells (BMMC). In these experiments, the responses of wild-type and Il4rαF709 BMMC, labeled with two different fluorophores (CFSE (carboxyfluorescein succinimidyl ester) or eFluor 670), were determined simultaneously in mixed co-cultures, ensuring that each individual cell was exposed to the identical cytokine milieu and culture conditions. As expected, IL-4 triggered the phosphorylation of STAT6 in BMMC, an effect that was enhanced in Il4rαF709 cells at all doses of IL-4 tested (Figure 3a). No response was observed following stimulation with IL-13 consistent with flow cytometric data showing a complete absence of the IL-13Rα1 chain on BMMC (data not shown). As Il4rαF709 BMMC exhibited enhanced IL-4-mediated activation of STAT6, we investigated whether another marker of IL-4 signaling in mast cells, namely upregulation of the high affinity IgE receptor α-chain (FcɛRIα), was also enhanced by disruption of the ITIM. FcɛRIα levels displayed a dose-dependent increase in expression upon IL-4 stimulation of BMMC, which was amplified in Il4rαF709 BMMC (Figure 3b).
Interleukin (IL)-4 drives mast cell activation, growth, and survival, and the IL-4Rα immunoreceptor tyrosine-based inhibitory motif limits these effects. (a) Il4rαF709 bone marrow mast cells (BMMC) exhibit enhanced phosphorylation of STAT6 (signal transducer and activator of transcription factor 6) in response to IL-4 stimulation. (b) Immunoglobulin E receptor (FcɛRIα) upregulation by IL-4 is enhanced in Il4rαF709 BMMC at 24 h. (c) IL-4 (2 ng ml−1), but not IL-13 (10 ng ml−1), enhances mast cell growth in combination with IL-3 and stem cell factor (SCF), particularly for Il4rαF709 BMMC. (d) Mast cell death in the absence of IL-3 and SCF is prevented by IL-4 but not IL-13, and the effect is more evident in Il4rαF709 BMMC. (e) IL-4 induces greater Bcl-2 and Bcl-XL expression in Il4rαF709 than wild-type BMMC. Statistical analysis by two-way analysis of variance ANOVA).*P<0.05, **P<0.01, and ***P<0.0001 by Bonferroni post-test where indicated. Data are representative of at least three experiments. MFI, mean fluorescent intensity.
The findings of IL-4-mediated induction of STAT6 phosphorylation and FcɛRI in BMMC along with the enhancement of both effects by the Il4rαF709 variant of IL-4Rα provided good evidence that IL-4 exerts direct activating effects on mast cells. In order to determine whether such IL-4 signals might also impact cell survival and growth, we examined IL-4 effects on the growth kinetics of BMMC in culture, both in the presence and absence of their physiological growth factors. BMMC normally proliferate when exposed to IL-3 and SCF. Their growth velocity was further increased by IL-4 (Figure 3c), an effect that was amplified in Il4rαF709 BMMC, which almost doubled over 4 days in the presence of IL-4 compared with a roughly 60% increase in wild-type BMMC. IL-13 had no effect. Normally, BMMC rapidly die off in the absence of IL-3 and SCF. We observed that IL-4, but not IL-13, could be protective in this setting with a fourfold improvement in the survival of wild-type cells and greater than sixfold in Il4rαF709 BMMC (Figure 3d). In keeping with our findings that IL-4 rescued BMMC from cytokine withdrawal, we found a dose-dependent induction of anti-apoptotic Bcl-2 and Bcl-XL proteins in growth factor–derived cells by the addition of IL-4 (Figure 3e). This effect was enhanced in Il4rαF709 BMMC and was evident at even low concentrations of IL-4 (1–2 ng ml−1).
STAT6 is required for IL-4-enhanced mast cell survival in vitro
The enhanced STAT6 phosphorylation exhibited by F709 mast cells suggested that the ITAM-driven STAT6 pathway might dominate in mediating many of the effects of IL-4 we had observed in BMMC. We therefore compared the responses of STAT6−/− and wild-type BMMC to IL-4. STAT6−/− BMMC displayed impaired upregulation of FcɛRIα (Figure 4a) and failed to proliferate when stimulated with IL-4 (Figure 4b). In addition, IL-4 was completely unable to rescue cytokine-starved STAT6−/− BMMC from death, which correlated with poor induction of Bcl protein expression (Figure 4c–e). These data demonstrate that the anti-apoptotic and activating effects of IL-4 on BMMC require STAT6 signal transduction.
Interleukin (IL)-4 drives mast cell activation, growth, and survival largely via STAT6 (signal transducer and activator of transcription factor 6). (a) immunoglobulin E (IgE) receptor (FcɛRIα) upregulation by IL-4 in mast cells is STAT6-dependent. Wild-type and STAT6−/− bone marrow–derived mast cells (BMMC) were fluorescently tagged and co-cultured in the presence of increasing amounts of IL-4. After 24 h, cells were stained for FcɛRIα and analyzed by flow cytometry. (b) IL-4 enhances mast cell growth in combination with IL-3 and stem cell factor (SCF) only when STAT6 is expressed. BMMC were co-cultured as in a for 5 days. (c) Mast cell death in the absence of IL-3 and SCF is prevented by IL-4 via STAT6. Data for day 5 of culture are shown. IL-4 induces (d) Bcl-2 and (e) Bcl-XL expression in wild-type but not STAT6−/− BMMC. Statistical analysis by two-way analysis of variance (ANOVA).*P<0.05, and ***P<0.0001 by Bonferroni post-test where indicated. Data are representative of at least three experiments. MFI, mean fluorescent intensity.
IL-4 receptor signals determine the extent of mast cell expansion in a mouse model of food allergy
Our demonstration of intestinal mast cell expansion in IL-4-treated and Il4rαF709 mice confirms an IL-4 effect on mast cell homeostasis. However, the in vivo system involves a complex interplay of cell types regulating mast cell growth. We therefore considered the possibility that the observed mast cell expansion in settings of enhanced IL-4 signaling might arise not from IL-4 effects directly on mast cells but rather indirectly by the induction of mast cell growth factors such as IL-3, IL-9 or SCF in neighboring cells residing in the intestinal mucosa. The BMMC results, however, provided strong support for cell-intrinsic effects of IL-4 on mast cells. In order to evaluate the physiological relevance of this direct effect in vivo in the context of an allergic response, we developed an adoptive transfer and competitive bone marrow chimera model of an allergic response in the intestine. This allowed us to compare the growth of both wild-type and Il4rαF709 mast cells in a single animal in the context of a robust food allergy response conferred by primed Il4rαF709 lymphocytes.
Cells from the mesenteric lymph node (MLN) of enterally allergen-sensitized F709 mice were used as a source of OVA-specific lymphocytes and were transferred into naive wild-type mice (Figure 5a). After repeated oral administration of the allergen OVA (three times over 10 days), intestinal mast cell numbers were readily expanded in the wild-type recipients, as assessed by flow cytometric analysis (data not shown). In order to address the direct contributions of IL-4R signaling to mast cell expansion in this setting, we performed such adoptive OVA-sensitized Il4rαF709 MLN transfers into bone marrow chimeras, which had previously been reconstituted with a 50:50 mixture of CD45 allotype-marked wild-type and IL-4Rα-deficient mast cells. In chimeras receiving OVA-sensitized MLN, OVA challenge lead to greater mast cell numbers than were observed in chimeras that received mock-sensitized MLN or did not receive MLN cells. Wild-type mast cells had a strong (over twofold) competitive advantage over IL-4Rα−/− cells as evidenced by the increase in their number over the mutant mast cells (Figure 5b). Similar transfers into mixed chimeras constructed using wild-type and Il4rαF709 bone marrow corroborated this finding, revealing a significant IL-4 signaling advantage in Il4rαF709 mast cells, which exhibited a 20% enhancement over wild-type cells in populating the OVA-challenged intestine (Figure 5c). Taken together, these chimera experiments demonstrate that the IL-4R α-chain directly promotes mast cell expansion in a cell-intrinsic manner under conditions mimicking food allergy and that the IL-4Rα ITIM provides an important brake on this expansion that is lost in Il4rαF709 mice.
Interleukin (IL)-4Rα signaling directly promotes mast cell expansion during food allergy in vivo. (a) Experimental design: mesenteric lymph node (MLN) cells from ovalbumin (OVA)-sensitized Il4rαF709 mice were adoptively transferred into naive recipient mice. The recipients were radiation bone marrow chimeras, previously reconstituted with a mixture (50:50) of bone marrow from wild-type and either Il4rαF709 or IL-4Rα−/− animals. They were then fed OVA over 10 days to drive mast cell expansion. Cells from saline-treated Il4rαF709 mice were separately transferred into control recipients. Intestinal mast cells were analyzed using flow cytometry. (b) IL-4Rα is required for maximal mast cell expansion. Adoptive transfer of OVA-allergic cells into wild-type/IL-4Rα−/− mixed bone marrow chimeras (n=4–5 per group) favors the outgrowth of IL-4Rα-sufficient mast cells. (c) Expression of an activated IL-4Rα variant promotes mast cell expansion in a cell-intrinsic manner in wild-type/Il4rαF709 mixed bone marrow chimera recipients (n=6 per group). Statistical analysis by repeated measures two-way analysis of variance with Bonferroni post-tests for b and c, *P<0.05, ***P<0.0001.
Discussion
Mast cells are critical effectors and regulators of food allergy. In addition to instigating potentially life-threatening anaphylactic reactions, they are thought to enhance immune sensitization and suppress regulatory T-cell responses following allergen exposure in the intestinal mucosa. Developing a complete understanding of the factors regulating their homeostasis in the intestine is a high priority in investigation of food hypersensitivity. In the current study, we have focused on the contributions of IL-4. Taking advantage of IL-4 receptor mutants with uninhibited signaling, we provide strong evidence that IL-4 enhances mast cell growth and survival in the gastrointestinal mucosa. We demonstrate that mast cell expansion occurring in response to IL-4 signals confers increased sensitivity to IgE-mediated systemic anaphylaxis. Our findings establish that both the addition of exogenous IL-4 and a cell-intrinsic increase in sensitivity to the cytokine are sufficient to enhance the growth of BMMC culture in SCF and IL-3, the survival of factor-deprived BMMC, the expression of FcɛRI, and the induction of anti-apoptotic gene expression (Figures 3 and 4). Using a competitive bone marrow chimera assay, we demonstrate that IL-4Rα expression provides a marked advantage to mast cells expanding in the intestine following food allergen exposure in vivo and that an additional incremental benefit is conferred by the presence of the uninhibited receptor variant, Il4rαF709. Taken together, these observations implicate IL-4 as a critical cytokine in the regulation of mast cell homeostasis and anaphylactic sensitivity in food allergy.
Our experimental approaches were optimized to address some of the complexities and inconsistencies raised in previous reports regarding IL-4 effects on mast cells. Several investigators have observed that addition of IL-4 enhances the growth of cultured mast cells derived from bone marrow or tissues.11, 18, 19, 22, 24, 28, 29, 30, 36, 37 Our results corroborate these findings and extend them by showing that not only exogenous IL-4 but also enhanced sensitivity to the cytokine conferred by the Il4rαF709 receptor at the mast cell level promotes growth in such cultures. The availability of IL-4R mutants further allowed us to assess the relative growth and survival advantages conferred by enhanced IL-4 sensitivity by performing mixed competition cultures seeded with equal numbers of normal and mutant mast cells, marked with different dyes, which could then be tracked concurrently in single wells. We found that under these conditions, IL-4 enhanced cell growth, IgE receptor expression, and survival in the absence of other growth factors in a cell-intrinsic manner.
We also evaluated whether the growth and survival involved the STAT6 vs. the AKT pathway downstream of IL-4Rα signaling. The results demonstrated that the IL-4 effects on growth, upregulation of FcɛRI, and on survival in the absence of other growth factors are all STAT6-dependent. We have previously reported that the same IL-4Rα variant drives increased STAT6 activation in T and B cells32 and now demonstrate that Il4rαF709 mast cells exhibit enhanced STAT6 phosphorylation. We are aware that Brown and colleagues38, 39 have shown that under some culture conditions IL-4 can trigger proteolytic degradation of STAT6, the key transducer of IL-4Rα signaling and that this mediates the induction of a unique transcriptome, but STAT6 phosphorylation nevertheless appears to be required for the induction of mast cell growth, survival, anti-apoptotic gene expression, and FcɛRI induction in our hands. Furthermore, these findings suggest that the AKT pathway may not contribute substantially to these downstream effects of IL-4 receptor engagement in BMMC.
In contrast to the mast cell–activating effects observed in our study and reported by others, a series of carefully performed analyses by Ryan and colleagues27 suggested that the addition of IL-4 to bone marrow cultures at the initiation of BMMC derivation delays mast cell development, drives mast cell apoptosis, and inhibits IgE receptor expression. These early cultures contain a heterogeneous mixture of immature and mature hematopoietic cell types many of which express IL-4 receptors. It is a challenge in that setting to discriminate between direct IL-4 effects on relatively rare mast cells and indirect effects in which IL-4 action on another intermediate cell type might trigger the production of cytokines or engagement of cell:cell interactions that could impair mast cell growth. Indeed, when these investigators added IL-4 to pure cultures of mature BMMC, they observed an augmentation rather than suppression of cell growth,29 and this is consistent with the findings of Rennick et al.30 who evaluated lymph node mast cell progenitor growth and differentiation ex vivo. We believe that the aggregate data support the conclusion that IL-4 signals support the growth and survival of differentiated mast cells in culture.
Although such culture analyses lend support to the idea that IL-4 regulates mast cell homeostasis, they do not establish that IL-4 signals impact mast cell growth under physiological conditions mimicking food allergy in vivo. We wanted to know whether the proliferative boost conferred by IL-4 signals mattered in a real allergic response. Previous studies by Finkelman and others4, 11, 40, 41 have examined the effect of exogenous IL-4 on intestinal mast cell numbers in naive, parasitized, or allergen-treated mice, but the experimental design in these studies did not discriminate between direct effects of IL-4 on mast cells and indirect ones mediated by other cell types, including epithelial cells or T cells residing in the intestinal mucosa (which might, in turn, produce IL-3, SCF, IL-9, or other mast cell growth factors). Taking advantage of the fact that adoptively transferred OVA-sensitized Il4rαF709 T cells confer enteral allergen responses to naive hosts, we developed a competitive bone marrow chimera strategy, which allowed us to establish that IL-4 is a physiologically relevant driver of mast cell expansion in response to allergen ingestion. In fact, IL-4Rα−/− mast cells showed absolutely no increase in this model, indicating that IL-4 not only provides a growth advantage but also is, in fact, required for allergen-induced mastocytosis. An additional incremental advantage was provided by the variant, indicating that increased IL-4 signals further augment mast cell growth in the intestine. We believe that these competition experiments not only corroborate the results obtained with BMMC but also establish the importance of IL-4 in regulating mast cell homeostasis in a physiological setting.
Our findings suggest that several cardinal features of food allergy, namely Th2 sensitization to allergen, mast cell expansion, and IgE-dependent mast cell activation and anaphylaxis, can all result from enhanced signaling through the IL-4Rα chain. These results provide additional rationale for targeting the IL-4–IL-4Rα axis in food allergy.40 In light of the emerging evidence implicating intestinal mast cells in regulation of DC phenotype,42, 43 Th2 induction, and regulatory T-cell suppression as well as their effector functions in immediate hypersensitivity, targeting the key growth factors that sustain them is likely to paralyze the allergic response to food allergens at multiple levels.
Methods
Mice. Animal procedures were performed under protocols approved by the Boston Children’s Hospital Institutional Animal Care and Use Committee. C.129 × 1-Il4ratm3.1Tch/J (Il4rαF709), IgE−/−, and Il4rαF709-IgE−/− mice on the BALB/c background are described previously.32 CBy.SJL(B6)-Ptprca/J (CD45.1), C.129S2-Stat6tm1Gru/J (STAT6−/−), BALB/c-Il4ratm1Sz/J (IL-4Rα−/−), C57BL/6j, and KitW-sh/HNihrJaeBsmJ (KitW-sh) mice were purchased from the Jackson Laboratory (Bar Harbor, ME). Wild-type BALB/cAnNTac mice were purchased from Taconic Farms (Germantown, NY). All mice were bred and maintained under barrier conditions.
Adoptive transfers, mixed bone marrow chimeras, and IL-4 treatment. We developed an adoptive transfer model of food allergen–induced mast cell expansion in the intestine in order to study the requirements for mast cell expansion independently of food allergen sensitization. Cells from the MLNs of OVA-sensitized Il4rαF709 donors were used as a source of OVA-specific lymphocytes and were transferred into naive wild-type recipients to drive mast cell expansion in the recipient intestine. Il4rαF709 mice were sensitized by oral gavage with 5 mg OVA in phosphate-buffered saline (PBS) once a week for 9 weeks or were mock sensitized with saline. MLN cells (5 × 106) were injected intraperitoneally into wild-type or chimeric (see below) recipients, which were then gavaged with 5 mg OVA on days 1, 4, and 7. The small intestine was examined for mastocytosis on days 10–11.
We have previously established that sublethal irradiation eliminates endogenous mast cell progenitors and that these cells can be reconstituted by bone marrow cell transfer.44 This procedure also effectively ablates and replaces the intestinal mucosal mast cells. Wild-type (CD45.2) mice were sub-lethally gamma-irradiated (500 rads) and reconstituted by retro-orbital intravenous injection of a 50:50 mix of CD45.1 (wild-type) and CD45.2 (IL-4Rα−/− or Il4rαF709) congenic bone marrow cells (107 cells total). Control chimeras were simultaneously reconstituted with only CD45.1 bone marrow to assess reconstitution efficiency and to check for any remaining host mast cell contamination. After allowing a week for mast cell progenitor reconstitution to occur, chimeras served as recipients of MLN cells in adoptive transfer experiments. Chimeras were maintained in autoclaved cages and treated with co-trimoxazole in the drinking water throughout the experiment.
IL-4 treatment of mice was performed using IL-4-anti-IL-4 complexes. Mice were injected intraperitoneally with 2 μg IL-4 (supernatant from IL-4-transfected ICL6 cells) and 10 μg anti-IL-4 (supernatant from hybridoma 11B11) on days 0, 3, and 6 and were killed for analysis on day 7. Similar results were obtained in preliminary experiments following a week-long treatment with daily injections of uncomplexed IL-4 or with purified recombinant IL-4 (Peprotech, Rocky Hill, NJ) and purified anti-IL-4 (Biolegend, San Diego, CA).
Mast cell culture. Cell culture was performed in RPMI-1640 medium supplemented with 10% fetal calf serum (FCS, Atlanta Biologicals, Lawrenceville, GA), 100U ml−1 penicillin (Gibco/Invitrogen, Grand Island, NY), 100 μg ml−1 streptomycin (Gibco), 2 mM L-glutamine (Sigma, St Louis, MO), 1% Minimum Essential Medium non-essential amino acids (Gibco), 10 mM HEPES (4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid) buffer (Gibco), 55 μM 2-mercaptoethanol (Gibco), and 10 μg ml−1 gentamicin (Life Technologies, Carlsbad, CA). BMMC were grown in vitro from bone marrow precursors in the presence of 10 ng ml−1 IL-3 (derived from supernatants of the WEHI-3b cell line) and 20 ng ml−1 SCF (as supernatant from SCF-transfected BHK-mKL cells). The experiments shown in this paper were performed using BMMC grown with supernatants from the aforementioned cell lines; however, similar results were obtained using BMMC grown with recombinant IL-3 and SCF (Peprotech). BMMC were used for experiments from week 5 through week 16 of culture. To assess in vitro response to IL-4, BMMC were fluorescently labeled according to the manufacturer’s instructions with either CellTrace CFSE (Life Technologies) or the far red cell proliferation dye eFluor 670 (eBioscience, San Diego, CA), e.g., wild-type-CFSE and Il4rαF709-e670, and were co-cultured in round bottom 96-well plates at 2 × 105 cells per well. The labeling was alternated from one experiment to the next to eliminate any bias that might be conferred by dye effects. Experiments addressing mast cell survival, Bcl protein expression, and STAT6 phosphorylation were performed in the absence of SCF and IL-3; for all other experiments, BMMC were cultured with IL-3 and SCF as above. Recombinant IL-4 from Peprotech was used exclusively for in vitro experiments.
Intestinal cell isolation. Intestinal leukocyte isolation procedures were adapted from Lefrançois and Lycke.45 Briefly, distinct cell preparations were isolated from the Peyer’s Patches, the intraepithelial layer, and the lamina propria. The small intestine was removed, flushed extensively with saline, and the Peyer’s Patches excised. The intestine was opened longitudinally, chopped crudely, and subjected to repeated 20 min incubations in Hank’s Balanced Salt Solution with 5% FCS, 2 mM EDTA, and 1 mM dithioerythreitol at 37 °C to remove the epithelial layer. The remaining tissue was digested with 300 U ml−1 collagenase IV (Worthington Biochemical, Lakewood, NJ), 50 U ml−1 hyaluronidase (Worthington), and 5 μg ml−1 DNase I (Applichem, St Louis, MO) in complete RPMI for three 20 min cycles at 37 °C to release lamina propria cells. The Peyer’s Patches were separately digested with the same enzyme cocktail for 30 min at 37 °C and then forced through 70 μM sieves (BD Pharmingen, Franklin Lakes, NJ). All cell fractions were suspended in 44% Percoll (GE Healthcare, Pittsburg, PA) and centrifuged at 500 g for 20 min to enrich for the denser leukocyte populations. The vast majority of mast cells was derived from the lamina propria fraction.
Flow cytometry. Cells were washed and stained in FACS (fluorescence-activated cell sorter) buffer (PBS with 2.5% FCS and 0.05% sodium azide). Non-specific binding to Fc receptors was blocking using anti-CD16/32 (clone 93, Biolegend) and non-viable cells were permanently marked using fixable viability dye eFluor 780 (eBioscience). Acquisition was performed on a custom order FACSCanto I (Becton Dickenson, Franklin Lakes, NJ) and FCS files were analyzed using FlowJo 8.8.7 (TreeStar, Ashland, OR) operating on Apple OS 10.4.11 (Apple, Cupertino, CA). Intestinal cell suspensions in unmanipulated mice were stained with a combination of FITC (fluorescein isothiocyanate)-conjugated lineage markers (B220 (RA3-6B2), CD3ɛ (145-2C11), CD4 (RM4-5), CD8α (53-6.7), CD11b (M1/70), CD11c (N418), Gr-1 (RB6-8C5)), anti-IgE-PE (phycoerythrin; 23G3, eBioscience) or anti-FcɛRIα-PE (MAR-1), anti-CD45-PE-Cy7 (30-F11), and anti-CD117/c-Kit-APC (allophycocyanin; 2B8) all from Biolegend unless otherwise specified. For mixed bone marrow chimeras, cells were stained with the combination of anti-CD45.1-FITC (A20, eBioscience), anti-CD45.2-PE (104, eBioscience), anti-FcɛRIα-PE-Cy7 (MAR-1), lineage cocktail-APC, and anti-CD117 (2B8)-Alexa Fluor 700. Expression of anti-apoptotic Bcl proteins was determined using the BD Cytofix/Cytoperm fixation and permeabilization kit in combination with anti-Bcl-2-PE (BCL/10C4, Biolegend) and anti-Bcl-XL-Alexa Fluor 488 (54H6, Cell Signaling Technology, Danvers, MA). Detection of phosphorylated STAT6 using anti-STAT6(pY641)-Alexa Fluor 647 (J71-773.58.11, BD Pharmingen) was performed according to procedures established by Krutzik et al.46 BMMC were stimulated for 15 min with IL-4 or IL-13, centrifuged for 3 min at 300 g, and fixed in ice cold methanol for 15 min.
Passive anaphylaxis. Mice were passively sensitized by retro-orbital injection of 10 μg IgE anti-DNP (clone SPE-7, Sigma-Aldrich, St Louis, MO) in normal saline. After 16 h, mice were challenged retro-orbitally with 500 μg DNP-BSA in normal saline. Core body temperature was measured using sub-dermally implanted transponders as previously described.3
Histamine and serotonin were purchased from Sigma-Aldrich and leukotriene C4 from Cayman Chemical (Ann Arbor, MI) and were injected at doses that were previously shown to produce dramatically different effects in control and IL-4-treated mice.14
Enzyme-linked immunosorbent assays. MMCP-1 (MCPT-1) was measured in serum samples using the ELISA kit from eBioscience according to the manufacturer’s instructions. In vivo capture of IL-4 was performed according to procedures outlined by Finkelman et al.47 Biotinylated anti-IL-4 (BVD6-24G2, Biolegend) was injected along with the IgE for passive anaphylaxis, and IL-4-anti-IL-4 biotin was captured out of serum samples using plate-bound anti-IL-4 (BVD4-1D11, BD Pharmingen).
Histology. Sections of jejunum were fixed in 4% paraformaldehyde or formalin for 16–72 h and then transferred into PBS with 0.05% sodium azide. Paraffin embedding and sectioning were performed by the Beth Israel Histology Core (Beth Israel Deaconess Medical Center, Boston, MA). Sections were deparaffinized using xylene, rehydrated in graded alcohols and stained with 0.04% pararosaniline, 0.04% sodium nitrite, and 0.04% naphthol AS-D chloroacetate (all Sigma) in PBS for 30 min at room temperature to detect mast cells. Sections were counterstained with Shandon Instant Hematoxylin (Fisher Scientific, Cambridge, MA) and mounted in Immunohistomount (Sigma). Images were captured on a Nikon E800 microscope (Nikon, Melville, NY).
Statistics. Data were routinely analyzed using the GraphPad Prism (version 5.01, GraphPad, La Jolla, CA) software statistics package. The specific tests applied to each data set and the two-tailed P values obtained are indicated in the figure legends.
References
Branum, A.M. & Lukacs, S.L. Food allergy among U.S. children: trends in prevalence and hospitalizations. NCHS Data Brief 10, 1–8 (2008).
Rudders, S.A., Banerji, A., Vassallo, M.F., Clark, S. & Camargo, C.A. Trends in pediatric emergency department visits for food-induced anaphylaxis. J. Allergy Clin. Immunol. 126, 385–388 (2010).
Mathias, C.B. et al. IgE-mediated systemic anaphylaxis and impaired tolerance to food antigens in mice with enhanced IL-4 receptor signaling. J. Allergy Clin. Immunol. 127, 795–805 e791-796 (2011).
Brandt, E.B. et al. Mast cells are required for experimental oral allergen-induced diarrhea. J. Clin. Invest. 112, 1666–1677 (2003).
Ahrens, R. et al. Intestinal mast cell levels control severity of oral antigen-induced anaphylaxis in mice. Am. J. Pathol. 180, 1535–1546 (2012).
Lin, R.Y. et al. Histamine and tryptase levels in patients with acute allergic reactions: An emergency department-based study. J. Allergy Clin. Immunol. 106 (1 Part 1), 65–71 (2000).
Piconese, S. et al. Mast cells counteract regulatory T-cell suppression through interleukin-6 and OX40/OX40L axis toward Th17-cell differentiation. Blood 114, 2639–2648 (2009).
Groschwitz, K.R. et al. Mast cells regulate homeostatic intestinal epithelial migration and barrier function by a chymase/Mcpt4-dependent mechanism. Proc. Natl. Acad. Sci. USA 106, 22381–22386 (2009).
Bryce, P.J. & Oettgen, H.C. Antigen-independent effects of immunoglobulin E. Curr. Allergy Asthma Rep. 5, 186–190 (2005).
Nelms, K., Keegan, A.D., Zamorano, J., Ryan, J.J. & Paul, W.E. The IL-4 receptor: signaling mechanisms and biologic functions. Annu. Rev. Immunol. 17, 701–738 (1999).
Madden, K.B. et al. Role of STAT6 and mast cells in IL-4- and IL-13-induced alterations in murine intestinal epithelial cell function. J. Immunol. 169, 4417–4422 (2002).
Ceponis, P.J., Botelho, F., Richards, C.D. & McKay, D.M. Interleukins 4 and 13 increase intestinal epithelial permeability by a phosphatidylinositol 3-kinase pathway. Lack of evidence for STAT 6 involvement. J. Biol. Chem. 275, 29132–29137 (2000).
Dabbagh, K., Takeyama, K., Lee, H.M., Ueki, I.F., Lausier, J.A. & Nadel, J.A. IL-4 induces mucin gene expression and goblet cell metaplasia in vitro and in vivo. J. Immunol. 162, 6233–6237 (1999).
Strait, R.T., Morris, S.C., Smiley, K., Urban, J.F. & Finkelman, F.D. IL-4 exacerbates anaphylaxis. J. Immunol. 170, 3835–3842 (2003).
Khodoun, M.V., Orekhova, T., Potter, C., Morris, S. & Finkelman, F.D. Basophils initiate IL-4 production during a memory T-dependent response. J. Exp. Med. 200, 857–870 (2004).
Chen, L. et al. IL-4 induces differentiation and expansion of Th2 cytokine-producing eosinophils. J. Immunol. 172, 2059–2066 (2004).
Mosmann, T.R., Bond, M.W., Coffman, R.L., Ohara, J. & Paul, W.E. T-cell and mast cell lines respond to B-cell stimulatory factor 1. Proc. Natl. Acad. Sci. USA 83, 5654–5658 (1986).
Hamaguchi, Y. et al. Interleukin 4 as an essential factor for in vitro clonal growth of murine connective tissue-type mast cells. J. Exp. Med. 165, 268–273 (1987).
Smith, C.A. & Rennick, D.M. Characterization of a murine lymphokine distinct from interleukin 2 and interleukin 3 (IL-3) possessing a T-cell growth factor activity and a mast-cell growth factor activity that synergizes with IL-3. Proc. Natl. Acad. Sci. USA 83, 1857–1861 (1986).
Lee, F. et al. Isolation and characterization of a mouse interleukin cDNA clone that expresses B-cell stimulatory factor 1 activities and T-cell- and mast-cell-stimulating activities. Proc. Natl. Acad. Sci. USA 83, 2061–2065 (1986).
Garside, P., Kennedy, M.W., Wakelin, D. & Lawrence, C.E. Immunopathology of intestinal helminth infection. Parasite Immunol. 22, 605–612 (2000).
Suzuki, K. et al. Role of common cytokine receptor gamma chain (gamma(c))- and Jak3-dependent signaling in the proliferation and survival of murine mast cells. Blood 96, 2172–2180 (2000).
Shelburne, C.P. & Ryan, J.J. The role of Th2 cytokines in mast cell homeostasis. Immunol. Rev. 179, 82–93 (2001).
Lorentz, A. & Bischoff, S.C. Regulation of human intestinal mast cells by stem cell factor and IL-4. Immunol. Rev. 179, 57–60 (2001).
Yeatman, C.F. et al. Combined stimulation with the T helper cell type 2 cytokines interleukin (IL)-4 and IL-10 induces mouse mast cell apoptosis. J. Exp. Med. 192, 1093–1103 (2000).
Bailey, D.P. et al. Interleukin-4 elicits apoptosis of developing mast cells via a Stat6-dependent mitochondrial pathway. Exp. Hematol. 32, 52–59 (2004).
Speiran, K. et al. Endogenous suppression of mast cell development and survival by IL-4 and IL-10. J. Leukoc. Biol. 85, 826–836 (2009).
Lorentz, A. et al. IL-4-induced priming of human intestinal mast cells for enhanced survival and Th2 cytokine generation is reversible and associated with increased activity of ERK1/2 and c-Fos. J. Immunol. 174, 6751–6756 (2005).
Macey, M.R. et al. IL-4 and TGF-beta 1 counterbalance one another while regulating mast cell homeostasis. J. Immunol. 184, 4688–4695 (2010).
Rennick, D., Hunte, B., Holland, G. & Thompson-Snipes, L. Cofactors are essential for stem cell factor-dependent growth and maturation of mast cell progenitors: comparative effects of interleukin-3 (IL-3), IL-4, IL-10, and fibroblasts. Blood 85, 57–65 (1995).
Chatila, T.A. Interleukin-4 receptor signaling pathways in asthma pathogenesis. Trends Mol. Med. 10, 493–499 (2004).
Tachdjian, R. et al. In vivo regulation of the allergic response by the IL-4 receptor alpha chain immunoreceptor tyrosine-based inhibitory motif. J. Allergy Clin. Immunol. 125, 1128–1136 e1128 (2010).
Tachdjian, R. et al. Pathogenicity of a disease-associated human IL-4 receptor allele in experimental asthma. J. Exp. Med. 206, 2191–2204 (2009).
Blaeser, F. et al. Targeted inactivation of the IL-4 receptor alpha chain I4R motif promotes allergic airway inflammation. J. Exp. Med. 198, 1189–1200 (2003).
Yamaguchi, M. et al. IgE enhances mouse mast cell Fc(epsilon)RI expression in vitro and in vivo: evidence for a novel amplification mechanism in IgE-dependent reactions. J. Exp. Med. 185, 663–672 (1997).
Yokota, T. et al. Isolation and characterization of a human interleukin cDNA clone, homologous to mouse B-cell stimulatory factor 1, that expresses B-cell- and T-cell-stimulating activities. Proc. Natl. Acad. Sci. USA 83, 5894–5898 (1986).
Lawrence, C.E., Paterson, J.C., Higgins, L.M., MacDonald, T.T., Kennedy, M.W. & Garside, P. IL-4-regulated enteropathy in an intestinal nematode infection. Eur. J. Immunol. 28, 2672–2684 (1998).
Sherman, M.A., Powell, D.R. & Brown, M.A. IL-4 induces the proteolytic processing of mast cell STAT6. J. Immunol. 169, 3811–3818 (2002).
Suzuki, K. et al. Proteolytic processing of Stat6 signaling in mast cells as a negative regulatory mechanism. J. Exp. Med. 196, 27–38 (2002).
Brandt, E.B. et al. Targeting IL-4/IL-13 signaling to alleviate oral allergen-induced diarrhea. J. Allergy. Clin. Immunol. 123, 53–58 (2009).
Finkelman, F.D. et al. Interleukin-4- and interleukin-13-mediated host protection against intestinal nematode parasites. Immunol. Rev. 201, 139–155 (2004).
Bryce, P.J., Miller, M.L., Miyajima, I., Tsai, M., Galli, S.J. & Oettgen, H.C. Immune sensitization in the skin is enhanced by antigen-independent effects of IgE. Immunity 20, 381–392 (2004).
Hepworth, M.R. et al. Mast cells orchestrate type 2 immunity to helminths through regulation of tissue-derived cytokines. Proc. Natl. Acad. Sci. USA 109, 6644–6649 (2012).
Gurish, M.F. et al. Intestinal mast cell progenitors require CD49dbeta7 (alpha4beta7 integrin) for tissue-specific homing. J. Exp. Med. 194, 1243–1252 (2001).
Lefrancois, L. & Lycke, N. Isolation of mouse small intestinal intraepithelial lymphocytes, Peyer’s patch, and lamina propria cells. Curr. Protoc. Immunol. (2001) Chapter 3: Unit 3,19.
Krutzik, P.O., Clutter, M.R. & Nolan, G.P. Coordinate analysis of murine immune cell surface markers and intracellular phosphoproteins by flow cytometry. J. Immunol. 175, 2357–2365 (2005).
Finkelman, F., Morris, S., Orekhova, T. & Sehy, D. The in vivo cytokine capture assay for measurement of cytokine production in the mouse. Curr. Protoc. Immunol. (2003) ; Chapter 6: Unit 6, 28.
Acknowledgements
Research reported in this publication was supported by NIH/NIAID Grants R21AI087666 and R56AI100889 (H.C.O.), T32AI007512 (O.T.B. and J.S.Z.), R01AI083516 (M.F.G.), Department of Defense FA100085 (T.A.C.), and by EPA Grant 83482501 (H.C.O.). We thank Dr Rosemary DeKruyff for the WEHI-3b and 11B11 cell lines and Dr Clinton Mathias for discussion.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declared no conflict of interest.
Additional information
SUPPLEMENTARY MATERIAL is linked to the online version of the paper
Supplementary information
Rights and permissions
About this article
Cite this article
Burton, O., Darling, A., Zhou, J. et al. Direct effects of IL-4 on mast cells drive their intestinal expansion and increase susceptibility to anaphylaxis in a murine model of food allergy. Mucosal Immunol 6, 740–750 (2013). https://doi.org/10.1038/mi.2012.112
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/mi.2012.112
This article is cited by
-
Interleukin 4 Reduces Brain Hyperexcitability after Traumatic Injury by Downregulating TNF-α, Upregulating IL-10/TGF-β, and Potential Directing Macrophage/Microglia to the M2 Anti-inflammatory Phenotype
Inflammation (2023)
-
The Role of Innate Immune Cells in Allergen Immunotherapy
Current Treatment Options in Allergy (2023)
-
Reduction of allergy effects of peanut sprout extract in a systemic anaphylaxis food allergy mouse model
Horticulture, Environment, and Biotechnology (2021)
-
IL-4 enhances survival of in vitro-differentiated mouse basophils through transcription-independent signaling downstream of PI3K
Cell Death & Disease (2018)
-
Short-term in vitro culture of purity and highly functional rat bone marrow-derived mast cells
In Vitro Cellular & Developmental Biology - Animal (2018)