Abstract
Excessive production of connective tissue growth factor (CTGF, CCN2) and increased motor ability of the activated fibroblast phenotype contribute to the pathogenesis of idiopathic pulmonary fibrosis (IPF). However, molecules and signal pathways regulating CCN2 expression and migration of lung fibroblasts are still elusive. We hypothesize that rapamycin, via binding and blocking mammalian target of rapamycin (mTOR) complex (mTORC), affects CCN2 expression and migration of lung fibroblasts in vitro. Primary normal and fibrotic human lung fibroblasts were isolated from lung tissues of three patients with primary spontaneous pneumothorax and three with IPF. Cells were incubated with regular medium, or medium containing rapamycin, human recombinant transforming growth factor (TGF)-β1, or both. CCN2 and tissue inhibitor of metalloproteinase (TIMP)-1 expression in cells or supernatant was detected. Wound healing and migration assay was used to measure the migratory potential. TGF-β type I receptor (TβRI)/Smad inhibitor, SB431542 and phosphoinositide 3-kinase (PI3K) inhibitor, LY294002 were used to determine rapamycin’s mechanism of action. We demonstrated that rapamycin amplified basal or TGF-β1-induced CCN2 mRNA and protein expression in normal or fibrotic fibroblasts by Smad-independent but PI3K-dependent pathway. Additionally, rapamycin also enhanced TIMP-1 expression as indicated by ELISA. However, wound healing and migrating assay showed rapamycin did not affect the mobility of fibroblasts. Collectively, this study implies a significant fibrogenic induction activity of rapamycin by activating AKT and inducing CCN2 expression in vitro and provides the possible mechanisms for the in vivo findings which previously showed no antifibrotic effect of rapamycin on lung fibrosis.
Similar content being viewed by others
Main
Idiopathic pulmonary fibrosis (IPF) is the most common and severe form of idiopathic interstitial pneumonia (IIP) that is usually fatal with a median survival time of 2.5–3.5 years.1 Although the etiology and pathogenesis of IPF still remains elusive, it is now suggested that epithelial cell injury-induced abnormal wound healing process has a critical role in the initiation and progression of IPF.2 Lung fibroblasts are the major effector cells involved in the dysregulated wound healing process, because overactivation and migration of them and their transition into myofibroblasts mainly contribute to the fibrous intercellular matrix production.3 One of the aberrant features of fibroblasts is that they produce excessive autocrine profibrotic mediators, including connective tissue growth factor (CTGF, CCN2).4 CCN2 is a multifunctional mediator that dysregulated expression of it is seen in many fibroproliferative diseases.5 Fibroblasts in the fibrotic lung also have an enhanced motile ability, which is reminiscent that IPF may be a neoproliferative, cancer-like disorder of the lung.6
However, factors as well as the underlying signaling pathways that regulate CCN2 expression and migration of fibroblasts have not been fully elucidated. Rapamycin (sirolimus) has profound immunosuppressive effects and is currently used for the prevention of graft rejection in organ transplant recipients.7 Rapamycin exerts its function through inactivating the mammalian target of rapamycin (mTOR) complex 1 (mTORC1).8 Prolonged exposure to or much higher concentration of rapamycin also blocks the assembly of new mTOR complex 2 (mTORC2) and inhibits its activity.9, 10 The primary downstream targets of mTORC1 are the p70S6 kinase 1 (p70S6K1) and the eukaryotic initiation factor 4E binding protein 1 (4E-BP1).8 In addition to immunosuppressive effects, rapamycin also showed to be effective in preventing fibrogenesis in animal models.11, 12, 13 However, the exact molecular mechanisms underlying the effects of rapamycin on preventing organ fibrosis remain poorly understood. Furthermore, the antifibrotic effect of rapamycin was seriously challenged by other studies, which showed that rapamycin had no significant improvements on fibrotic process.14, 15, 16 So, we aim to investigate the possible mechanisms that may explain the controversial findings by showing that whether rapamycin modulates CCN2 expression and migration of lung fibroblasts in vitro.
MATERIALS AND METHODS
Subjects and Lung Tissue Procurement
Lung tissue was obtained from three IPF patients with histological evidence of usual interstitial pneumonia at the time of surgical lung biopsy. The diagnosis of IPF was arrived at by standard accepted American Thoracic Society/European Respiratory Society recommendations.1 Histological normal lung tissue as controls was obtained from three patients with primary spontaneous pneumothorax at the time of thoracoscopy with stapling of any air leak. All experiments were done by using the three fibrotic and normal primary cell lines of human lung fibroblast (HLF). This study was approved by the Ethics Committee of Beijing Chao-Yang Hospital of Capital Medical University and written informed consent was obtained according to institutional guidelines from all investigated subjects.
Isolation, Primary Cultures, and Identification of HLFs
Tissue pieces anchoring culture method was used for primary fibroblast culture as previously described.17 Detailed culture conditions were described in the Supplementary Information. The identification and purity of the cultured primary lung fibroblasts were shown in our previous papers.18, 19
Cell Stimulation and Pharmacological Treatments
To investigate modulatory effects of rapamycin (Sigma, San Francisco, CA, USA) on cell behavior, normal or fibrotic HLFs (N-/F-HLFs) were incubated for different periods of time (1, 6, 12, 24, and 48 h) with rapamycin (5 ng/ml) in the absence or presence of transforming growth factor (TGF)-β1 (10 ng/ml, BD, San Diego, CA, USA). To study the modulatory mechanisms of rapamycin on HLFs, TGF-β type I receptor (TβRI)- and phosphoinositide 3-kinase (PI3K)-specific antagonist (SB431542 and LY294002; 5 and15 μM; Biotrend, Cologne, Germany) was used. After treatments, culture supernatants were harvested and fibroblasts were processed for protein and RNA extraction.
RNA Purification and Real-Time RT-PCR
Total RNA was isolated from HLFs using RNAeasy Miniprep kit (Tiangen, Beijing, China) and real-time PCR was performed using an ABI PRISM 7500 Instrument (Applied Biosystems, Foster City, CA, USA) with SYBRGreen PCR reagents (Tiangen) as described in the Supplementary Information. The fold change of the target genes was calculated as 2−ΔΔCT method.20
Protein Extraction, SDS-PAGE, and Indirect Immunoblot Analysis
The expression or activation of mTOR, S6K1, 4EBP1, AKT, Smad, and CCN2 in cell lysates was determined by western blot assay. Quantitative data were derived by densitometry measured with ImageJ software. Details on these methods are provided in the Supplementary Information.
ELISA of CCN2/TIMP-1 in Cell-Culture Supernatant
The levels of CCN2 and tissue inhibitor of metalloproteinase (TIMP)-1 in cell conditioned media were measured with commercial human ELISA kits (Invitrogen, Carlsbad, CA, USA). Detailed information on the method is available in the Supplementary Information.
Indirect Immunofluorescence Staining and Confocal Microscopy
Stainings were done with FITC-conjugated goat anti-rabbit secondary antibodies to detect p-Smad2/3 and Smad2/3 expression and distribution. Cell images were captured by confocal laser scanning microscope (Olympus, Tokyo, Japan). Assays were performed as described in the Supplementary Information.
Wound Healing and Migration Assays
Wound healing and migration assays were done as described earlier.21, 22 For detailed information, please go to see the Supplementary Information.
Statistics
SPSS 13.0 (SPSS, Chicago, IL, USA) software was used for analyses. Data are reported as means±s.e.m. Statistical analysis was performed by using the analysis of variance (ANOVA) test for significance. P-values <0.05 were considered as significant.
RESULTS
Rapamycin Attenuates the Activity of mTOR/p70S6K/4EBP1 Signaling Pathway in HLFs
We initially aimed to determine whether the mTOR/p70S6K/4EBP1 pathway phosphorylation/activation in F-HLFs is regulated by rapamycin. We found rapamycin (0.01–10 ng/ml) significantly decreased basal or TGF-β1 induced phospho-mTOR/p70S6K/4EBP1 expression in HLFs (Figure 1). Previously, we also showed rapamycin downregulates activity of mTOR signal in N-HLFs.18
Effect of rapamycin on the activity of mTOR/p70S6K/4EBP1 signal cascade in human fibrotic lung fibroblast. (a) Left panel: HLFs were incubated with different doses of rapamycin from 0.01 to 10 ng/ml for 24 h. Western blot was performed to determine total or phosphorylated (activated) form of mTOR/p70S6K/4EBP-1. The gel is a representative for three independent experiments (each with duplicates) from three different cell lines giving similar results. Right panel: Densitometric analysis of phospho-mTOR/S6K/4EBP relative to total mTOR/S6K/4EBP levels. Data are shown as means±s.e.m. (n=3) **P<0.01 vs. control group in terms of p-mTOR/mTOR; #P<0.05, ##P<0.01, ###P<0.001 vs. control group in terms of p-S6K/S6K; $$P<0.01 vs. control group in terms of p-4EBP/4EBP. (b) Left panel: HLFs were incubated with different doses of rapamycin (0.01–10 ng/ml) for 24 h in the presence of 10 ng/ml TGF-β1. Western blot was performed to determine total or phosphorylated (activated) form of mTOR/p70 S6K/4E-BP1. The gel is a representative for three independent experiments (each with duplicates) from three different cell lines giving similar results. Right panel: Densitometric analysis of phospho-mTOR/S6K/4EBP relative to total mTOR/S6K/4EBP levels. Data shown are means±s.e.m. (n=3). *P<0.05, **P<0.01, ***P<0.001 vs. TGF-β group. Molecular weights: p-mTOR/mTOR, 289 KDa; p-S6K/S6K, 70 KDa; p-4EBP/4EBP, 15 KDa.
Rapamycin Promotes Basal and TGF-β1 Induced CCN2 mRNA and Protein Expression
We next want to investigate whether rapamycin modulates CCN2 expression in both N-HLFs and F-HLFs. As shown in Figures 2a and b, mRNA steady-state level of CCN2 was significantly induced by rapamycin in a dose-dependent manner in both N-HLFs and F-HLFs. We then used 5 ng/ml (more effective dose) rapamycin (with or without 10 ng/ml TGF-β1) to further illustrate its modulatory effect on CCN2 mRNA expression in a time-dependent manner. As shown in Figures 2c and d, 5 ng/ml rapamycin remarkably promoted CCN2 mRNA expression from 1 to 48 h, especially when co-stimulation with 10 ng/ml TGF-β1. Western blot and ELISA further showed that 5 ng/ml rapamycin alone or with combination of 10 ng/ml TGF-β1 upregulated CCN2 protein expression in whole cell lysate (Figure 3) and culture media (Figure 4) in both N-HLFs and F-HLFs.
Rapamycin increases CCN2 mRNA expression in normal and fibrotic fibroblast. (a, b) Serum-starved subconfluent N-/F-HLFs were treated with varying doses of rapamycin (0.01–10 ng/ml) for 24 h. After incubations, total cellular RNA was extracted and CCN2 mRNA steady-state levels were determined by real-time RT-PCR and normalized with β-actin mRNA. Values shown are means±s.e.m. (n=3 different cell lines, each with experimental duplicates, *P<0.05 vs. vehicle control group). (c, d) Serum-starved subconfluent N-/F-HLFs were divided into four groups: control group, rapamycin (5 ng/ml) group, TGF-β1 (10 ng/ml) group, and rapamycin+TGF-β1 co-incubation group. At 1, 6, 12, 24, and 48 h, total cellular RNA was extracted and CCN2 mRNA steady-state levels were determined by real-time RT-PCR. Values represent means±s.e.m. (n=3 different cell lines, each with experimental duplicates, **P<0.01, ***P<0.001 vs. control group).
Protein expression of CCN2 in normal and fibrotic fibroblast induced by rapamycin, TGF-β1, or both. Serum-starved subconfluent N-/F-HLFs were divided into four groups: control group, rapamycin (5 ng/ml) incubation group, TGF-β1 (10 ng/ml) group, and rapamycin+TGF-β1 co-incubation group. Whole-cell lysates were harvested in RIPA buffer and 30 μg of cell extracts was subjected to SDS-PAGE. CCN2 and β-actin protein band of N-HLFs (a) and F-HLFs (b) was examined by ChemiDoc XRS at 1, 6, 12, 24, and 48 h. Left panel: Typical western blot bands represent three independent experiments (each with duplicates) from three different cell lines giving similar results. Right panel: Densitometric results as the ratio of CCN2 to β-actin and shown as means±s.e.m. (n=3, *P<0.05, **P<0.01, ***P<0.001 vs. control group). Molecular weights: CCN2, 38 KDa; β-actin, 42 KDa.
Rapamycin increases CCN2 protein expression in culture media of normal and fibrotic fibroblast. Quiescent N-HLFs (a) and F-HLFs (b) were divided into four groups: control group, rapamycin (5 ng/ml) incubation group, TGF-β1 (10 ng/ml) group, and rapamycin+TGF-β1 co-incubation group. Cell supernatants were harvested at indicated time points and secretory CCN2 protein was determined by ELISA. Bars represent the average of three independent experiments from different cell lines with standard error, each with duplicate samples. *P<0.05, **P<0.01, ***P<0.001 vs. control group.
PI3K, Not Smad, Is Involved in Rapamycin’s Effects on CCN2 Expression in HLFs
We hypothesize that whether TβR1/Smad is also involved in rapamycin’s positive effect on CCN2 expression in HLFs. As shown in Figures 5a and b and Figures 6a and b, rapamycin (5 ng/ml) failed to induce a rapid or persistent phosphorylation of Smad2/3 from 1 to 48 h both in F-HLFs and in N-HLFs. Conversely, TGF-β1 (10 ng/ml) caused a remarkable and consistent activation of Smad2/3 as expected. However, the positive effect of TGF-β1 cannot be further amplified when rapamycin was added.
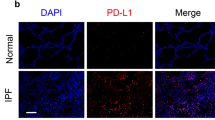
Smad2/3 activation and location in normal fibroblast. (a) Quiescent N-HLFs were stimulated with either vehicle (−) or with rapamycin (5 ng/ml), TGF-β1 (10 ng/ml), or both for the indicated time points. Then, cells were lysed for western blot analysis and probed with anti-(phospho)-Smad 2/3-specific antibodies. The typical western blot bands are representative for three independent experiments (each with duplicates) from three different cell lines giving similar results. Molecular weight: (p)-Smad2/3, 58 KDa. (b) Densitometric results as the ratio of p-Smad2/3 to Smad2/3 analyzed by ImageJ software. Data represent means±s.e.m (n=3, *P<0.05, ***P<0.001 vs. control group). (c) Quiescent N-HLFs were first simulated with vehicle or rapamycin (5 ng/ml), TGF-β1 (10 ng/ml), or both for 1 h. Then cells were fixed and stained with anti-p-Smad2/3 antibody. FITC-conjugated goat anti-rabbit secondary antibodies were used for color making. DAPI staining was used to detect nuclei. Bar shows 20 μM.
Smad2/3 activation and location in fibrotic fibroblast. (a) Quiescent F-HLFs were stimulated with either vehicle (−) or with rapamycin (5 ng/ml), TGF-β1 (10 ng/ml), or both and were lysed for western blot analysis. The bands are representative for three independent experiments (each with duplicates) from three different cell lines giving similar results. Molecular weight: (p)-Smad2/3, 58 KDa. (b) The quantified results measured by using ImageJ software show the densitometry as the ratio of p-Smad2/3 to Smad2/3. Data represent means±s.e.m. (n=3, *P<0.05, **P<0.01, ***P<0.001 vs. control group). (c) The subcellular localization of p-Smad2/3 in F-HLFs was analyzed by immunostaining with p-Smad2/3-specific antibody after incubation with rapamycin (5 ng/ml), TGF-β1 (10 ng/ml), or both for 1 h. DAPI staining was used to detect nuclei. Bar shows 20 μM.
Next, we designed experiment to explore whether rapamycin affects nuclear translocation of p-Smad2/3 in HLFs. As indicated in Figure 5c and Figure 6c, in basal state, p-Smad2/3 was expressed largely in cytoplasm of N-HLFs and F-HLFs. When cells were treated with rapamycin (5 ng/ml) for 1 h, nuclear translocation of p-Smad2/3 in N/F-HLFs remained unchanged. However, TGF-β1 treatment either in the presence or in the absence of rapamycin for 1 h significantly promoted p-Smad2/3 nuclear translocation. In addition, total Smad2/3 can localize to both the nucleus and cytoplasm of basal N-/F-HLFs; however, the nucleus was the predominant locating site. This feature was not affected by rapamycin, TGF-β1, or both (Supplementary Figures S1 and S2).
Third, we used SB431542 (Smad inhibitor) to determine whether it could block rapamycin’s positive action on CTGF expression in N-/F-HLFs. SB431542 alone failed to induce a remarkable change of CTGF expression in N-/F-HLFs (Supplementary Figure S3A and C). Also, we found that SB431542 (5 μM) did not change CCN2 mRNA expression induced by rapamycin (Figures 7a and d, left column). Larger dose of SB431542 (15 μM) could even potentiate rapamycin’s positive action on CCN2 expression. On the contrary, SB431542 (5 and 15 μM) significantly attenuated CCN2 mRNA expression induced by TGF-β1 treatment (Figures 7b and e, middle column). In N-HLFs, SB431542 also downregulated CCN2 mRNA expression when cells were treated with both rapamcyin and TGF-β1 (Figure 7c). This was inconsistent with SB431542’s effects on F-HLFs, which showed that it even facilitated CCN2 mRNA production (Figure 7f).
The effect of SB431542 on CCN2 expression of normal and fibrotic fibroblast. After incubations with rapamycin (a and d), TGF-β1 (b and e) or both (c and f) in the presence of SB431542 for 24h, CCN2 mRNA steady-state levels in N-HLFs (a–c) and F-HLFs (d–f) were determined by quantitative RT-PCR. Bars indicate mean±s.e.m. of three independent experiments from three different cell lines, each with duplicates. *, **, ***Significant difference, P<0.05, P<0.01, P<0.001, respectively.
Next, whether the PI3K pathway regulates rapamycin’s positive effects on CCN2 expression in N-/F-HLFs was examined. We first showed that rapamycin (5 ng/ml) treatment significantly promoted p-AKT (S473) expression, especially when treated with TGF-β1 (10 ng/ml) (Figures 8a and 9a). LY294002, an inhibitor to the PI3K-AKT pathway, cannot change the basal expression of CCN2 in N-/F-HLFs (Supplementary Figure S3B and D). However, we then showed that LY294002 (5 and 15 μM) completely blocked CCN2 mRNA that was induced by rapamcyin (Figures 8b and 9b, left panel). LY294002 also significantly reduced CCN2 mRNA expression induced by TGF-β1 (Figures 8b and 9b, middle panel). Furthermore, rapamycin and TGF-β1 co-stimulated N-HLFs/F-HLFs also showed reduced CCN2 expression when incubated with LY294002 (Figures 8b and 9b, right panel).
PI3K-AKT was involved in CCN2 expression of normal fibroblast. (a) Serum-starved N-HLFs were stimulated with either vehicle (−) or rapamycin (5 ng/ml), TGF-β1 (10 ng/ml) or both and were lysed for western blot analysis. Left panel: The typical gel is shown to represent three independent experiments (each with duplicates) from three different cell lines giving similar results. Molecular weight: (p)AKT, 56 KDa. Right panel: Densitometric analysis as the ratio of p-AKT to total AKT is shown with mean±s.e.m. (n=3, *P<0.05, **P<0.01, ***P<0.001 vs. control group). (b) After incubations with rapamycin, TGF-β1, or both in the presence of LY-294002 for 24 h, CCN2 mRNA steady-state levels were determined by quantitative RT-PCR. Bars indicate mean±s.e.m. of three independent experiments performed, each with duplicates. **, *** Significant difference, P<0.01, P<0.001, respectively.
PI3K-AKT was involved in CCN2 expression of fibrotic fibroblast induced by rapamycin and TGF-β1. (a) Serum-starved F-HLFs were stimulated with either vehicle (−) or with rapamycin (5 ng/ml), TGF-β1 (10 ng/ml), or both and were lysed for western blot analysis. Left panel: The typical gel is shown to represent three independent experiments (each with duplicates) from three different cell lines giving similar results. Molecular weight: (p)AKT, 56 KDa. Right panel: Densitometric analysis as the ratio of p-AKT to total AKT is shown with mean±s.e.m. (n=3, **P<0.01, ***P<0.001 vs. control group). (b) CCN2 mRNA steady-state levels of F-HLFs were determined by quantitative RT-PCR. Bars indicate mean±s.e.m. of three independent experiments performed, each with duplicates. **, *** Significant difference, P<0.01, P<0.001, respectively.
Rapamycin Does Not Affect Migration of F-HLF
It was previously showed that CCN2 and tissue inhibitor matrix metalloproteinase-1 (TIMP-1) were all evolved in modulating migration of different cell types.23, 24 ELISA found that rapamycin itself remarkably increased TIMP-1 protein level in culture media (Figure 10e). However, wound healing study showed that the migratory capacity of F-HLFs was not changed by rapamycin (Figure 10a and b). In addition, this was further proved by chamber migration assay (Figure 10c and d), which indicated that rapamycin had no regulatory effects on cell traversing capability from upper to lower chamber.
Effect of rapamycin on the migrating ability of fibrotic fibroblast. (a, b) Serum-starved fibrotic HLFs were further incubated for 12, 24, and 48 h in the absence or presence of rapamycin (5 ng/ml) in DMEM containing 1% FBS. (a) A representative example of wound healing assay. (b) Summary of wound assay results. Values are healed area of wound compared with scratching time; bars show s.e.m.; (c, d): Fibrotic HLFs were incubated with serum-free medium for 24 h, and then different doses of rapamycin (0.1–10 ng/ml) were added for another 24 h. Cells were harvested and seeded on the upper side of millipore chambers for migrating analysis. (c) Representative example of transwell migration assay. (d) Summary of wound assay results. Values are numbers of migrated HLFs compared with vehicle group; bars show s.e.m. (e) ELISA for TIMP-1 protein level in cell culture medium. Bars represent the average of three independent experiments with standard error, each with duplicate samples. *P<0.05, **P<0.01.
DISCUSSION
Currently, rapamycin was mainly used for immunosuppressive therapy because of its anti-inflammatory and anti-immunity actions.7, 25 However, mTOR is universally expressed regardless of cell types, so rapamycin was gradually used in anti-cancer and anti-fibrotic therapies.11, 26, 27 We used N- and F-HLFs to demonstrate that rapamycin potently exerts direct profibrotic activities by promoting CCN2 expression in a Smad-independent and PI3K-dependent manner. In our sister paper,28 we also showed rapamycin potentiates CCN2 expression in alveolar epithelial cells by PI3K pathway. Furthermore, we and others also showed that while rapamycin downregulated collagen mRNA or protein expression in normal human fibroblast,18, 29 it could even facilitate the expression of collagen I α1 mRNA in the presence of TGF-β1 (unpublished preliminary data), indicating that the downstream effectors are differentially modulated by mTORC when inhibited by rapamycin and may be highly cell specific. The overall effect of rapamycin on lung fibrosis relies on the balance of the controversial functions on lung structural cells. Consideration of rapamycin’s complex actions, we and others suggest it should be handled carefully for clinical uses.14, 15, 16, 30, 31 In addition, we also show here the hypothesis that monotherapy with rapamycin may be unhelpful but combined inhibition of mTOR and PI3K may be more effective therapeutic strategy for lung fibrosis.
CCN2 is a multifunctional, matricellular protein that is widely documented to relate to the progression of various fibroproliferative diseases and patients outcome.32 CCN2 regulates different cell types, including pulmonary type II alveolar cells, mesangial cells, and interstitial fibroblasts.33 In the present study, we showed that rapamycin (5 ng/ml) significantly potentiated basal CCN2 mRNA and protein expression in N-/F-HLFs (Figures 2,3,4). TGF-β1 is a potent inducer of CCN2,34 we also found that rapamycin further induced CCN2 expression in N-/F-HLFs in the presence of TGF-β1 (Figures 2,3,4), indicating a powerful synergistic action between them. Considering TGF-β1 signal is overactivated in IPF lung and fibrotic lung, fibroblasts are more responsive to rapamycin in CCN2 production, our findings suggest that treatment of IPF with rapamycin may significantly potentiate the profibrotic activities of both rapamcyin and TGF-β1 and aggravate disease evolution rather than alleviate it. Other findings are consistent with us. One in vitro study showed that rapamycin and cyclosporine A synergistically upregulated human mesangial cells’ (HMCs) CCN2 expression and may also exert profibrotic effects.35 Another in vitro study showed that rapamycin promoted CCN2 mRNA and protein expression in rat mesangial cells (RMCs) in transcriptional way.36 An in vivo study37 used a rat model of chronic nephrotoxicity to show that rapamycin further augmented CCN2 expression in kidney tissue and promoted kidney fibrosis. However, other data38 also showed that rapamcyin attenuated human chronic allograft nephropathy by reducing CCN2 expression. This seems rather paradoxical. We suggest that various doses and treatment time windows of rapamycin and different animal models may serve to reconcile discrepancies regarding the modulatory effects of rapamycin on CCN2 expression.
But how does rapamycin, through inhibiting mTOR signal cascade, promote CCN2 expression of fibroblast? Previous study showed rapamycin promotes CCN2 and PAI-1 gene expression of RMCs via a TGF-β/Smad cascade-dependent way.36 However, our studies showed that in contrast to TGF-β1 (10 ng/ml) inducing an early and persistent increase in p-smad2/3 expression and nuclear transition rapamycin cannot (Figures 5 and 6). Also, Smad signal-specific inhibitor SB431542 could partly block CCN2 mRNA expression induced by TGF-β1, but not by rapamycin (Figure 7). SB431542 also partly inhibited rapamcyin and TGF-β1’s synergic functions in N-HLFs, which was not seen in F-HLFs. This may be interpreted that in F-HLFs, SB431542’s effect on rapamycin offsets and overcomes the effect on TGF-β1, so CCN2 expression induced by rapamcyin and TGF-β1 co-incubation was even augmented. To sum up, we suggest that, in contrast to TGF-β1 that induces CCN2 expression partly dependent on smad signal, rapamcyin’s positive effect on CCN2 expression is smad independent.
Alternatively, we found that rapamycin facilitated AKT phosphorylation in S473 of N-/F-HLFs, especially at early exposure and when incubated with TGF-β1 (Figures 8a and 9a). Considering that acute inhibitory effect of rapamycin primarily focuses on mTORC1 (not mTORC2), and it has been shown that mTORC2 is the kinase of Akt at the serine in position 473,39 we suspect that uninhibited or hyperactive mTORC2 is sufficient to phosphorylate AKT and contributes to the early AKT activation of lung fibroblasts induced by rapamycin. Persistent exposure of rapamycin may inhibit mTORC2, especially when the concentration of rapamycin is relatively high, up to μM range.40 In all, 5 ng/ml (5.5 nM) rapamycin was used in this study, so the later inhibitory effect on mTORC2 may be limited in a small range. Thus, rapamycin alone failed to induce a significant reduction in the level of AktS473 phosphorylation at later stage especially in F-HLFs (Figures 8a and 9a). On the other hand, continuous and significant suppression of mTORC1 leads to the loss of negative feedback loop resided in S6K41 and secondary activation of known or unknown compensatory kinase, which eventually increases the level of AktS473 phosphorylation. This is especially true when lung fibroblasts continuously challenged with rapamycin in the presence of TGF-β1 (Figures 8a and 9a). AKT phosphorylation in S473, together with the one at T308, is needed for maximal Akt activity. In the previous study, we also showed that rapamycin activated PI3K (p110a), p-AKT (Thr308), and p-AKT (Ser 473) in different lung epithelial cell lines.28 Also, LY294002 almost completely blocked basal CCN2 mRNA expression induced by rapamycin, indicating that PI3K-AKT signal contributed to the positive effect of rapamycin on CCN2 expression (Figures 8b and 9b). This was in line with our previous study28 and not in accordance with Osman B’s study.36 So signal pathway that lies behind the positive modulatory effects of rapamycin may vary in the concern of different cell type. The underling mechanisms involving in rapamycin function on fibrotic HLFs should be further elucidated. Collectively, we draw the conclusion that rapamycin blocks one output of PI3K-Akt signaling (mTORC1) at the expense of activating other outputs.
It was previously shown that CCN2 enhanced the migration of monocyte cells by increasing monocyte chemoattractant protein (MCP-1) expression.23 Also, another profibrotic mediator, TIMP-1, was shown to promote the migration of cancer-associated fibroblasts (CAFs).24 So, we hypothesized that whether rapamycin, via modulating CCN2 and TIMP-1 expression, affects HLFs migration. We found although CCN2 and TIMP-1 expression was upregulated by rapamycin, the migration of fibroblast was unchanged (Figure 10). These results offer at least two possibilities. One is that mTORC1 signal pathway does not affect the motor ability of fibroblasts. Another is that mTORC1 may affect cell mobility but the dose of rapamycin or detecting time covers the possible changes. Further studies should be done to illustrate rapamcyin’s effect on migration of HLFs not only in the basal state which is merely chemotacticed by the concentration gradient of fetal bovine serum (FBS), but also in the TGF-β1-induced state. Also, experiments should be done to determine whether rapamcyin modulates other functional features of HLFs, such as differentiation ability in vitro.
CONCLUSION
Despite their beneficial roles, mTOR inhibitors in some cases can induce significant interstitial pneumonia and early fibrotic changes with largely unknown mechanisms.30, 31 In this study, we showed that lung fibroblast would respond to rapamycin by augmenting CCN2 expression via PI3K-AKT pathway. In fact, in tumor treatment, it was said that there were limitations of monotherapy for inhibiting feedback-regulated pathways and suggested that combined treatment with mTOR and P3IK/MAPK inhibitors would show more anti-tumor activity in a wide range of human malignance.42 In line with this idea, we hypothesized that if rapamycin was used for the treatment of fibrotic diseases, combined inhibition of PI3K and mTOR pathways may have additive anti-fibrotic effects. Further in vivo studies should be designed to determine whether these findings are value.
Change history
27 October 2020
A Correction to this paper has been published: https://doi.org/10.1038/s41374-020-00501-5
References
Raghu G, Collard HR, Egan JJ et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 2011;183:788–824.
Camelo A, Dunmore R, Sleeman MA et al. The epithelium in idiopathic pulmonary fibrosis: breaking the barrier. Front Pharmacol 2014;4:173.
King TE Jr., Pardo A, Selman M . Idiopathic pulmonary fibrosis. Lancet 2011;378:1949–1961.
de Winter P, Leoni P, Abraham D . Connective tissue growth factor: structure-function relationships of a mosaic, multifunctional protein. Growth Factors 2008;26:80–91.
Leask A, Abraham DJ . The role of connective tissue growth factor, a multifunctional matricellular protein, in fibroblast biology. Biochem Cell Biol 2003;81:355–363.
Vancheri C, Failla M, Crimi N et al. Idiopathic pulmonary fibrosis: a disease with similarities and links to cancer biology. Eur Respir J 2010;35:496–504.
Webster AC, Lee VW, Chapman JR et al. Target of rapamycin inhibitors (sirolimus and everolimus) for primary immunosuppression of kidney transplant recipients: a systematic review and meta-analysis of randomized trials. Transplantation 2006;81:1234–1248.
Huber TB, Walz G, Kuehn EW . mTOR and rapamycin in the kidney: signaling and therapeutic implications beyond immunosuppression. Kidney Int 2011;79:502–511.
Sarbassov DD, Ali SM, Sengupta S et al. Prolonged rapamycin treatment inhibits mTORC2 assembly and Akt/PKB. Mol Cell 2006;22:159–168.
Shor B, Zhang WG, Toral-Barza L et al. A new pharmacologic action of CCI-779 involves FKBP12-independent inhibition of mTOR kinase activity and profound repression of global protein synthesis. Cancer Res 2008;68:2934–2943.
Korfhagen TR, Le Cras TD, Davidson CR et al. Rapamycin prevents transforming growth factor-alpha-induced pulmonary fibrosis. Am J Respir Cell Mol Biol 2009;41:562–572.
Mehrad B, Burdick MD, Strieter RM . Fibrocyte CXCR4 regulation as a therapeutic target in pulmonary fibrosis. Int J Biochem Cell Biol 2009;41:1708–1718.
Simler NR, Howell DC, Marshall RP et al. The rapamycin analogue SDZ RAD attenuates bleomycin-induced pulmonary fibrosis in rats. Eur Respir J 2002;19:1124–1127.
Renken CFD, Kundt G, Gretz N, Haffner D . Inhibition of mTOR with sirolimus does not attenuate progression of liver and kidney disease in PCK rats. Nephrol Dial Transplant 2011;26:92–100.
Madala SK, Maxfield MD, Davidson CR et al. Rapamycin Regulates Bleomycin-Induced Lung Damage in SP-C-Deficient Mice. Pulm Med 2011;2011:653524.
Lorenzen JM, Schonenberger E, Hafer C et al. Failed rescue therapy with rapamycin after paraquat intoxication. Clin Toxicol (Phila) 2010;48:84–86.
Jablonska E, Markart P, Zakrzewicz D et al. Transforming growth factor-beta1 induces expression of human coagulation factor XII via Smad3 and JNK signaling pathways in human lung fibroblasts. J Biol Chem 2010;285:11638–11651.
Gao Y, Xu X, Ding K et al. Rapamycin inhibits transforming growth factor beta1-induced fibrogenesis in primary human lung fibroblasts. Yonsei Med J 2013;54:437–444.
Xu X, Wan X, Geng J et al. Kinase inhibitors fail to induce mesenchymal-epithelial transition in fibroblasts from fibrotic lung tissue. Int J Mol Med 2013;32:430–438.
Schmittgen TD, Livak KJ . Analyzing real-time PCR data by the comparative C(T) method. Nat Protoc 2008;3:1101–1108.
Pilquil C, Dewald J, Cherney A et al. Lipid phosphate phosphatase-1 regulates lysophosphatidate-induced fibroblast migration by controlling phospholipase D2-dependent phosphatidate generation. J Biol Chem 2006;281:38418–38429.
Wang SL, Shi XH, Yang Z et al. Osteopontin (OPN) is an important protein to mediate improvements in the biocompatibility of C ion-implanted silicone rubber. PLoS ONE 2014;9:e98320.
Liu SC, Hsu CJ, Fong YC et al. CTGF induces monocyte chemoattractant protein-1 expression to enhance monocyte migration in human synovial fibroblasts. Biochim Biophys Acta 2013;1833:1114–1124.
Gong Y, Scott E, Lu R et al. TIMP-1 promotes accumulation of cancer associated fibroblasts and cancer progression. PLoS ONE 2013;8:e77366.
Sehgal SN . Rapamune (RAPA, rapamycin, sirolimus): mechanism of action immunosuppressive effect results from blockade of signal transduction and inhibition of cell cycle progression. Clin Biochem 1998;31:335–340.
Dancey J . mTOR signaling and drug development in cancer. Nat Rev Clin Oncol 2010;7:209–219.
Bridle KR, Popa C, Morgan ML et al. Rapamycin inhibits hepatic fibrosis in rats by attenuating multiple profibrogenic pathways. Liver Transpl 2009;15:1315–1324.
Xu X, Wan X, Geng J et al. Rapamycin regulates connective tissue growth factor expression of lung epithelial cells via phosphoinositide 3-kinase. Exp Biol Med (Maywood) 2013;238:1082–1094.
Shegogue D, Trojanowska M . Mammalian target of rapamycin positively regulates collagen type I production via a phosphatidylinositol 3-kinase-independent pathway. J Biol Chem 2004;279:23166–23175.
Filippone EJ, Carson JM, Beckford RA et al. Sirolimus-induced pneumonitis complicated by pentamidine-induced phospholipidosis in a renal transplant recipient: a case report. Transplant Proc 2011;43:2792–2797.
Shihab FS, Bennett WM, Yi H et al. Sirolimus increases transforming growth factor-beta1 expression and potentiates chronic cyclosporine nephrotoxicity. Kidney Int 2004;65:1262–1271.
Cheng O, Thuillier R, Sampson E et al. Connective tissue growth factor is a biomarker and mediator of kidney allograft fibrosis. Am J Transplant 2006;6:2292–2306.
Moussad EE, Brigstock DR . Connective tissue growth factor: what's in a name? Mol Genet Metab 2000;71:276–292.
Hardie WD, Hagood JS, Dave V et al. Signaling pathways in the epithelial origins of pulmonary fibrosis. Cell Cycle 2010;9:2769–2776.
O'Connell S, Slattery C, Ryan MP et al. Sirolimus enhances cyclosporine a-induced cytotoxicity in human renal glomerular mesangial cells. J Transplant 2012;2012:980910.
Osman B, Doller A, Akool el S et al. Rapamycin induces the TGFbeta1/Smad signaling cascade in renal mesangial cells upstream of mTOR. Cell Signal 2009;21:1806–1817.
Shihab FS, Bennett WM, Yi H et al. Effect of cyclosporine and sirolimus on the expression of connective tissue growth factor in rat experimental chronic nephrotoxicity. Am J Nephrol 2006;26:400–407.
Liu M, Zhang W, Gu M et al. Protective effects of sirolimus by attenuating connective tissue growth factor expression in human chronic allograft nephropathy. Transplant Proc 2007;39:1410–1415.
Sarbassov DD, Guertin DA, Ali SM et al. Phosphorylation and regulation of Akt/PKB by the rictor-mTOR complex. Science 2005;307:1098–1101.
Foster DA, Toschi A . Targeting mTOR with rapamycin: one dose does not fit all. Cell Cycle 2009;8:1026–1029.
Sabatini DM . mTOR and cancer: insights into a complex relationship. Nat Rev Cancer 2006;6:729–734.
Roberts PJ, Usary JE, Darr DB et al. Combined PI3K/mTOR and MEK inhibition provides broad antitumor activity in faithful murine cancer models. Clin Cancer Res 2012;18:5290–5303.
Acknowledgements
We would like to thank Dr Bin You, Jinbai Miao, Qirui Chen, Department of Thoracic Surgery, Beijing Chao-Yang Hospital for their kind supply of lung tissue specimens from informed patients. We also thank Prof. Jun Wang, AP Yan Liang, AP Xingyuan Jia, RA Ran Miao, RA Dong Leng, RA Ying Wang, Beijing Key Laboratory of Respiratory and Pulmonary Circulation Disorders, for their excellent technical assistance. This work was supported by grants from the Key Program of National Natural Science Foundation of China (No. 81430001) and the Key Program of Beijing Natural Science Foundation (No. 7131008).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Laboratory Investigation website
In this paper, the authors show that rapamycin significantly augments basal or transforming growth factor (TGF)-β1-induced connective tissue growth factor expression in normal and fibrotic human lung fibroblasts via activation of the phosphatidyl-inositol-3-kinase (PI3K)-AKT pathway. Rapamcin has no antifibrotic effect and in some cases, even promotes the generation of fibrotic lesions. Combined inhibition of PI3K and mTOR may be a more effective regime for antifibrotic treatment.
Rights and permissions
About this article
Cite this article
Xu, X., Dai, H., Geng, J. et al. Rapamycin increases CCN2 expression of lung fibroblasts via phosphoinositide 3-kinase. Lab Invest 95, 846–859 (2015). https://doi.org/10.1038/labinvest.2015.68
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.2015.68
This article is cited by
-
Buyang Huanwu Tang inhibits cellular epithelial-to-mesenchymal transition by inhibiting TGF-β1 activation of PI3K/Akt signaling pathway in pulmonary fibrosis model in vitro
BMC Complementary Medicine and Therapies (2020)
-
Connective tissue growth factor promotes temozolomide resistance in glioblastoma through TGF-β1-dependent activation of Smad/ERK signaling
Cell Death & Disease (2017)