Abstract
Nitrofuranyl benzimidazoles can be made in one synthetic step from commercially available starting materials. The compounds displayed unexpected antibacterial activity against methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin-resistant enterococci with MICs as low as 1 μg ml−1.
Similar content being viewed by others
Introduction
In 2004, the Infectious Disease Society of America reported that each year 90 000 of the two million people who acquired hospital bacterial infections died, a 4.5% mortality rate during hospitalization.1 Multidrug-resistant bacterial strains are a major problem that has been increasing very rapidly every year during the last few decades.2, 3 Since first reported in 1961, the incidence of methicillin-resistant Staphylococcus aureus (MRSA) has increased and accounted for >50% of S. aureus patient isolates in ICUs (intensive care units) within the NNIS (National Nosocomial Infection Surveillance) system by 1999. By 2003, 59.5% of isolates were MRSA.4, 5 Vancomycin-resistant enterococci has had a similar rapid rise in hospital isolates increasing from its discovery in 1986 to 25% of all enterococcal isolates in 1999 and then increasing further to 28.3% by 2003 in NNIS surveyed ICUs.6 It is apparent that without the introduction of new antibiotics, this rise in multidrug-resistant strains will continue exposing hospital patients to undue risk of infection and possible death. These alarming statistics motivated a broad screen of compounds generated in our laboratory against MRSA and various ‘hits’ were revealed in a screening collaboration with Achillion Pharmaceuticals. Among the scaffolds discovered were synthetically intensive quinolone–cephalosporins conjugates7 as well as various other scaffolds, all of which bore a reducible moiety. One synthetically attractive compound series (3a-e) was based on low molecular weight nitrofuran benzimidazoles with surprising potency against a number of important pathogens (Table 1). Herein, we describe our efforts to rapidly generate structure activity relationships from compound (1) utilizing commercially available diamines and the assessment of these agents as cost effective antibiotics against drug-resistant MRSA strains. Only the active compounds are described in this manuscript as analogs in which the nitro was missing or replaced by a bromide or sulfonic acid (SO3H), as well as benzimidazoles bearing a methyl ester, carboxylic acid or guanidine, were all inactive (>64 μg ml−1, data not shown).
The only three approved nitrofuran-containing drugs (nitrofurantoin CAS #67-20-9, furazolidone CAS #67-45-8 and nitrofurazone CAS #59-87-0) that are on the market to treat various infections (urinary tract, gastrointestinal and skin, respectively) are shown in Figure 1. All three are hydrazine derivatives, but many other preclinical nitrofuran-based agents have since emerged. For instance, Lee and colleagues, formerly at the University of Tennessee, demonstrated that various nitrofuran amides are potent inhibitors of Mycobacterium tuberculosis, the causative agent of tuberculosis.8 A dual action antimicrobial agent RBx-7644 reported by the Ranbaxy Laboratories9 is a nitrofuran substituted oxazolidinone modeled after linezolid. A number of recent patents also claim utility of nitrofuran bearing compounds.10, 11, 12, 13, 14, 15, 16 Other nitrofuran benzimidazole compounds with good antimicrobial activity have been studied for their antileukemic properties.17 Herein, we describe a one-step synthesis of nitrofuran benzimidazoles with activity against multidrug-resistant ‘super bug’ strains of MRSA and vancomycin-resistant enterococci.
Results and discussion
Chemistry
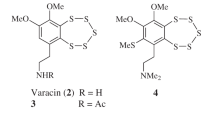
Condensation of 5-nitro-2-furaldehyde 1 with various diamines (2a–e) in methanol followed by in situ oxidation with potassium ferricyanide in air gave substituted benzimidazoles (3a–e) as shown in Scheme 1. The products were easily recrystallized from ethanol/water (80:20).
Biological assay results
Compounds 3a–e were initially screened for antibiotic activity against representative Gram-negative strains of Escherichia coli and Pseudomonas aeruginosa and representative strains of Gram-positive methicillin-susceptible and methicillin-resistant S. aureus. The MIC values obtained are shown in Table 1 and indicated that this initial set of compounds had good antibacterial activity. To further assess their potential, the effect of protein binding on the activity was assessed by adding 50% mouse or human serum to the MIC assays, and calculating the fold shift in MIC values. The results indicated compound-specific effects ranging from 2 × to 16 × increases in MICs. Potential mammalian toxicity was initially assessed by screening the compounds against the Hep2 cancer cell line. Though all compounds had similar antibacterial activity, compound 3e appeared to be the most promising of the set based on having the lowest MICs against E. coli (2 μg ml−1) and the two Gram-positive strains (2 μg ml−1) with only a 4 × MIC shift in the presence of either mouse or human serum and it exhibited the least cytotoxicity against mammalian cell lines.
Based on these positive initial screening results, compound 3e was selected for additional studies. The potency of 3e was retained against a set of MRSA clinical isolates and the MIC values of 1–2 μg ml−1 obtained were similar to those of vancomycin against the same strains (Table 2). In an expanded panel of Gram-positive bacteria, including various drug-resistant strains, compound 3e compared favorably with ciprofloxacin and was shown to be bactericidal by MBC analysis (Table 2) for 3e the MIC=MBC indicating bactericidal activity. Compound 3e showed significantly less activity against an expanded panel of Gram-negative bacteria, suggesting selectivity for Gram-positive bacteria.
Exposure of S. aureus American Type Culture Collection (ATCC) 29213 to various concentrations of 3e and determining time-kill curves confirmed the indication that 3e is bactericidal (Figure 2). At 2, 4 and 8 times the MIC, bacterial killing was observed throughout the full 24-h time course of the study. The efficacy of 3e at the 2–8 times MIC was comparable to vancomycin at four times MIC.
To further assess general toxicity and estimate a selectivity index, compound 3e was exposed to a panel of five eukaryotic cell lines: HepG-2, HeLa, CHO, CEM-SS and the yeast C. albicans. The CC50 values of 3e in these studies were 37, 20, 97 and 90 μM and an MIC of >64 μg ml−1 for C. albicans, respectively. While some toxicity was observed in the eukaryotic cell lines, there was notable antibacterial selectivity. Microbial selectivity was also indicated by the lack of antifungal activity against C. albicans.
Frequency of spontaneous resistance selection by compound 3e in three different strains of S. aureus (ATCC strains 29213, 700699 and 33591) was studied by exposure of the test strains to 2–4 times the MIC value of 3e. The rates of spontaneous resistant frequencies were very low for compound 3e: <2.6 × 10−10 (n=2), <6.4 × 10−10 (n=1) and <2.8 × 10−10 (n=1) for strains 29213, 700699 and 33591, respectively. Further attempts to induce resistance involved growing of S. aureus ATCC 29213 in liquid media containing compound 3e at 0.5–2 times its MIC. After eight passages only minimal (2 × ) resistance was observed, suggesting that multiple steps will be required for the acquisition of resistance.
Mechanism of action studies were run using compound 3e in macromolecular synthesis assays. As shown in Figure 3, 3e significantly inhibited DNA, RNA and protein syntheses at nearly equivalent levels. This profile is consistent with the mechanism of action of compounds such as nitrofurantoin that inhibit numerous cellular processes once internalized into the bacterial cytoplasm.18 3e was also negative for hemolysis in a rat red blood cell assay that can be indicative of membrane perturbation properties (data not shown).
Compound 3e also was shown to be reasonably stable in human, dog, rat, monkey and mouse plasma with half-lives (t1/2) of 4.5, 5.6, 3.9, 2.0 and 3.6 h, respectively. It was also stable in the dosing vehicle (potassium phosphate at pH 7.4) with no degradation after 4 h. However, compound 3e showed rapid metabolism in human liver and rat liver microsomes being completely cleared within 30 min. Stability of 3e in the human liver and rat liver S9 fractions (HLS9 and RLS9) showed rapid clearance in RLS9 (<30 min), but some limited stability in HLS9 with 13% remaining after 60 min of incubation and an estimated half-life of only 12.6 min.
Conclusion
Syntheses and microbiological analyses of nitrofuranyl benzimidazoles revealed that they are readily prepared, microbe-selective antibiotics with notable activity against important drug-resistant bacteria and drug-like properties appropriate for further development and consideration. Improved metabolic stability would be a key area to focus on in future lead optimization studies.
Experimental Procedure
All anhydrous solvents, reagent grade solvents for chromatography and starting materials were purchased from either Aldrich Chemical (Milwaulkee, WI, USA) or Fisher Scientific (Suwanee, GA, USA). Water was distilled and purified through a Milli-Q water system (Millipore, Bedford, MA, USA). The reactions were monitored by TLC on precoated Merck 60 F254 silica gel plates (Merck, Darmstadt, Germany) and visualized using UV light (254 nm). All compounds were analyzed for purity by HPLC and characterized by 1H and 13C NMR using Varian 300 MHz NMR and/or Varian 500 MHz NMR spectrometers (Varian, Inc., Palo Alto, CA, USA). Chemical shifts are reported in p.p.m. (δ) relative to the residual solvent peak in the corresponding spectra; dimethyl sulfoxide (DMSO) δ 2.50 and δ 39.52, methanol δ 3.31 and δ 49.00 and coupling constants (J) are reported in hertz (Hz) and analyzed using MestReC NMR data processing. Mass spectra values are reported as m/z. The liquid chromatography mass spectrum (‘LC/MS’) analyses were carried out on Waters ZQ instrument (Waters, Milford, MA, USA) consisting of chromatography module Alliance HT, photodiode array detector 2996, and mass spectrometer Micromass ZQ, using a 3 × 50 mm Pro C18 YMC reverse phase column. Mobile phases: 10 mM ammonium acetate in HPLC grade water (A) and HPLC grade acetonitrile (B). A gradient was formed from 5 to 80% of B in 10 min at 0.7 ml min−1. The MS electrospray source operated at capillary voltage 3.5 kV and a desolvation temperature 300 °C. All reactions were conducted with atmospheric exposure. Solvents were removed in vacuo on a rotary evaporator. DCM, dichloromethane; EtOH, ethanol; HOAc, acetic acid; HPLC tR, HPLC retention time.
2-(5-Nitrofuran-2-yl)-1- H -benzo[d]imidazole, 3a, 5-Nitro-2-furaldehyde (1, 1.0 g, 7.0 mmol) and 1,2-phenylenediamine (2a, 658 mg, 6.0 mmol) were dissolved in 15 ml of methanol. A solution of potassium ferricyanide (4.2 g, 12.6 mmol) in 8 ml of water was added and the reaction mixture was heated to reflux for 3 h with exposure to air. The reaction mixture was cooled, filtered and the filter pad washed with ethanol. The filtrate and washings were combined and concentrated in vacuo. The residue was recrystallized from EtOH:H2O (80:20) to give 1.34 g (7.0 mmol, 83%) of 3a as a tan solid after filtration. Mp 225–226 °C 1H NMR (300 MHz, DMSO) δ 7.91 (1H, d, J=3.9 Hz), 7.66 (2H, m), 7.48 (1H, d, J=3.7 Hz), 7.30 (2H, m); HPLC tR=5.55 min. (>95%), FABMS 230.3 (M+H); HRMS calcd. For C11H7N3O3, 230.0566 found 230.0561.
5-Chloro-2-(5-nitrofuran-2-yl)-1 H -benzo[d]imidazole, 3b was prepared by reaction of 1 (304 mg, 2.1 mmol) with 4-chloro-1,2-phenlyenediamine (2c, 253 mg, 1.8 mmol) in 10 ml of methanol for 16 h under the same conditions used for the preparation of 3a to give 257 mg (1.8 mmol, 55%) of 3b as a yellow solid after recrystallization. Mp 234–235 °C 1H NMR (300 MHz, DMSO) δ 7.96–7.82 (1H, bs), 7.76–7.57 (2H, bs), 7.55–7.43 (1H, bs), 7.37–7.23 (1H, bs). HPLC tR=7.03 min (>95%), FABMS 264.2 (M+H). HRMS calcd. for C11H6ClN3O3, 264.0176 found 264.0189.
5-Fluoro-2-(5-nitrofuran-2-yl)-1 H -benzo[d]imidazole, 3c was prepared by reaction of 1 (310 mg, 2.2 mmol) and 4-fluoro-1,2-phenlyenediamine (2c, 230 mg, 1.8 mmol) in 10 ml of methanol for 3 h under the same conditions used for the preparation of 3a to give 111 mg (1.8 mmol, 25%) of 3c as a yellow-green solid after recrystallization. Mp 224–225 °C 1H NMR (300 MHz, DMSO) δ 7.96–7.84 (1H, bs), 7.75–7.60 (1H, bs), 7.58–7.38 (2H, bs), 7.27–7.08 (1H, bs). HPLC tR=6.07 min (>95%), FABMS 248.3 (M+H). HRMS calcd. for C11H6FN3O3, 248.0471 found 248.0474.
7-Methyl-2-(5-nitrofuran-2-yl)-1 H -benzo[d]imidazole, 3d was prepared by reaction of 1 (407 mg, 2.8 mmol) 2,3-diaminotoluene (2f, 300 mg, 2.4 mmol) in 10 ml of methanol for 3 h under the same conditions used for the preparation of 3a to give 519 mg (2.8 mmol, 75%) of 3d as a brown-tan solid after recrystallization. Mp 222–223 °C 1H NMR (300 MHz, DMSO) δ 7.82 (1H, d, J=3.9 Hz), 7.40 (2H, m), 7.11 (1H, t, J=7.6, 7.6 Hz), 7.01 (1H, d, J=6.8 Hz), 2.61 (3H, s); HPLC tR=6.32 min (>95%), FABMS 244.4 (M+H). HRMS calcd. for C12H9N3O3, 244.0722 found 244.0729.
2-(5-Nitrofuran-2-yl)-3 H -benzo[d]imidazole-4ol, 3e was prepared by reaction of 1 (278 mg, 2.6 mmol) and 2,3-diaminophenol (2e, 300 mg, 2.4 mmol) in 10 ml of methanol for 16 h under the same conditions used for the preparation of 3a to give 340 mg (2.6 mmol, 53%) of 3e as a gold-orange solid after recrystallization. Mp >295 °C 1H NMR (300 MHz, DMSO) δ 7.90 (1H, m), 7.42 (1H, m), 7.06 (2H, m), 6.59 (1H, m); HPLC tR=4.73 min (>95%). FABMS 246.4 (M+H); HRMS calcd. for C11H7N3O4, 246.0515 found 246.0504.

(i) K2Fe(CN)6, methanol, air, reflux, 16 h.
Determination of in vitro antimicrobial activity
MICs were determined as outlined by the CLSI (CLSI (2006). Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard. CLSI document M7-A7, 7th 22 ed., vol. 26, 23 no. 2. CLSI, Wayne, PA, USA). The MIC was defined as the lowest concentration of each compound that resulted in inhibition of bacterial visible growth after incubation at 37 °C for 18–24 h. All bacterial strains used in this work were obtained from either the ATCC or the Achillion Pharmaceuticals Culture Collection.
Determination of bactericidal activity
Bactericidal activity was determined by two independent methods. MBCs were determined by plating 10 μl of inoculated medium from MIC wells that showed no visible bacterial growth. The lowest compound concentrations from the wells that resulted in no growth on the agar plates (>99.9% killing) were designated as the MBCs. Time-kill studies were also done. Briefly, all strains were cultured overnight at 37°C, diluted into fresh medium, grown to exponential phase, and then diluted again in medium to adjust cell densities to ∼107 CFU ml−1. Compounds were then added at concentration multiples of the MIC. Rates of killing were determined by measuring the reduction in viable bacteria (log10 CFU ml−1) at 0, 1, 2, 4, 6 and 24 h at fixed concentrations of compound. Experiments were performed in duplicate. If plates contained fewer than 10 CFU ml−1, the number of colonies was considered to be below the limit of quantitation. Samples of culture containing compound were diluted at least 10-fold to minimize drug carryover to the agar plates.
Macromolecular synthesis assays
The effects of compound 3e and control compounds ciprofloxacin (DNA synthesis), rifampicin (RNA synthesis) and chloramphenicol (protein synthesis) on DNA, RNA and protein synthesis in bacteria were determined using radiolabeled precursors [3H]-thymidine (DNA), [3H]-uracil (RNA), [3H]-leucine (protein) in mid-exponential-phase cultures (∼108 CFU ml−1) of S. aureus ATCC 29213 in a chemically defined medium as previously described.19 Final concentrations of 5 μCi ml−1 for thymidine and 2.5 μCi ml−1 for each of the other precursors were added to cultures immediately before the addition of antibiotics (10 × MIC). Negative controls for the macromolecular assays consisted of all reaction materials with no antibiotics added and the resulting counts were used as the 100% values. After an additional 20 min incubation at 37 °C in the presence of antibiotics, samples were removed for trichloroacetic acid precipitation and subsequent scintillation counter analyses for determination of radioactive incorporation into DNA, RNA or protein, and the data expressed as a percent inhibition of incorporation into a drug-free control.
Cytotoxicity assay
Cytotoxicity is reported as a CC50 value, defined as the concentration of drug that results in toxicity to 50% of the cells compared with untreated control cells. Cytotoxicity was measured by Alamar Blue reduction as the amount of fluorescence or absorbance is proportional to the number of living cells and corresponds to cellular metabolic activity. Damaged and non-viable cells have lower innate metabolic activity, and thus generate a proportionally lower signal than healthy cells. Hep2 (human laryngeal carcinoma) HepG-2 (human hepatocellular carcinoma), HeLa (cervical carcinoma), CHO (Chinese hamster ovary), CEM-SS (human T lymphoblastoid) cell lines were incubated with drug concentrations at 37 °C for 72 h to generate seven-point CC50 data.
References
Infectious Diseases Society of America. Bad Bugs, No Drugs. http://www.idsociety.org/pa/IDSA_Paper4_final_web.pdf. Infectious Diseases Society of America, Alexandria, VA, 2004.
Klevens, R. M. et al. Changes in the epidemiology of methicillin-resistant Staphylococcus aureus in intensive care units in US hospitals, 1992–2003. Clin. Infect. Dis. 42, 389–391 (2006).
Gaynes, R. & Edwards, J. R. Overview of nosocomial infections caused by gram-negative bacilli. Clin. Infect. Dis. 41, 848–854 (2005).
Fridkin, S. K. et al. The effect of vancomycin and third-generation cephalosporins on prevalence of vancomycin-resistant enterococci in 126 U.S. adult intensive care units. Ann. Intern. Med. 135, 175–183 (2001).
Jones, R. N. Resistance patterns among nosocomial pathogens. Trends over the past few years. Chest 119, 397S–404S (2001).
Treitman, A. N., Yarnold, P. R., Warren, J. & Noskin, G. A. Emerging incidence of Enterococcus faecium among hospital isolates (1993 to 2002). J. Clin. Microbiol. 43, 462–463 (2005).
Zhao, G., Miller, M. J., Franzblau, S., Wan, B. & Möllmann, U. Syntheses and studies of quinolone-cephalosporins as potential anti-tuberculosis agents. Bioorg. Med. Chem. Lett. 16, 5534–5537 (2006).
Tangallapally, R. P., Yedapally, R., Lee, R. E., Lenaerts, A. J. M. & Lee, R. E. Synthesis and evaluation of cyclic secondary amine substituted phenyl and benzyl nitrofuranyl amides as novel antituberculosis agents. J. Med. Chem. 48, 8261–8269 (2005).
Das, B., Metha, A. & Rattan, A. (Ranbaxy Laboratories Limited). Polymorphic forms of phenyl oxazolidinone derivatives. WO 2003/097059, 27 November (2003).
Chamberland, S. & Malouin, F. (Ulysses Pharmaceutical Products, Inc.). Halogenated quinazolinyl nitrofurans as antibacterial agents. WO 2005/014585, 17 February (2005).
Szarvasi, E. & Fontaine, L. (Lipha, Lyonnaise Industrielle Pharmaceutique). Novel substituted (Nitrofurylacrylidene) hydrazines with antibacterial properties. US 3847911, 7 January (1971).
Agarwal, S. K., Akella, S.S.V.S. & Samuel, M. M. (Orchid Chemicals & Pharmaceuticals Ltd.). Oxazolidinone derivatives as antibacterial agents. WO 2003/097640, 27 November (2003).
Spazzoni, P. (Sigma-Tau Industrie Farmaceutiche Riuite). Process for preparing nitrofurylbenzimidazole and pharmaceutical compositions having antimycotic, antibacterial and antitubercular activities containing same. EP 0252028A1, 1 January (1988).
Chamberland, S. & Malouin, F. (Ulysses Pharmaceutical Products, Inc.). New substituted furan compounds-useful for the treatment of bacterial infection. WO 2006/032138, 30 March (2006).
Yonezawa, K., Shibata, H. & Mori, Y. (Toyama Chemical Company Ltd.). Anti-heliobacter agents. WO 1996/008247, 21 March (1996).
Magee, A. S. et al. (Essential Therapeutics, Inc.). Novel anti-infective nitrofuran-containing heterocyclic derivatives. WO 2003/000255, 1 March (2003).
Pedini, M., Bistocchi, G. A., Ricci, A., Bastianini, L. & Lepri, E. New heterocyclic derivatives of benzimidazole with germicidal activity—XII—Synthesis of N1-glycosyl-2-furyl benzimidazoles. Farmaco 49, 823–827 (1994).
McOsker, C. C. & Fitzpatrick, P. M. Nitrofurantoin: mechanism of action and implications for resistance development in common uropathogens. J. Antimicrob. Chemother. 33, 23–30 (1994).
Mychajlonka, M., McDowell, T. D. & Shockman, G. D. Inhibition of peptidoglycan, ribonucleic acid, and protein synthesis in tolerant strains of Streptococcus mutants. Antimicrob. Agents Chemother. 17, 572–582 (1980).
Acknowledgements
This research was supported in part by Grant 2R01AI054193 from the National Institutes of Health (NIH). We would like to thank the Mass Spectrometry and Proteomics Facility (Bill Boggess, Michelle Joyce, Nonka Sevova), which is supported by the grant CHE-0741793 from the NSF and Viktor Krchnak for LC-MS analysis. We thank Prof. Jennifer DuBois for her scientific discussions and constant support. We thank Jijun Cheng for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moraski, G., Thanassi, J., Podos, S. et al. One-step syntheses of nitrofuranyl benzimidazoles that are active against multidrug-resistant bacteria. J Antibiot 64, 667–671 (2011). https://doi.org/10.1038/ja.2011.67
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2011.67
Keywords
This article is cited by
-
Tackling vancomycin-resistant bacteria with ‘lipophilic–vancomycin–carbohydrate conjugates’
The Journal of Antibiotics (2015)