Abstract
The second derivative of the digital photoplethysmogram (SDPTG) is an indicator of arterial stiffness. The ratio of the height of the d wave to the a wave of the SDPTG (d/a) is associated with functional peripheral vascular tension and represents aortic-blood pressure (BP) augmented by reflection waves from the periphery. This longitudinal study aimed to investigate the relationship between SDPTG and cardiovascular mortality in middle-aged and elderly Japanese women. From 1998 to 2008, we recruited 4373 women (50–79 years old at baseline) who underwent medical check-ups and SDPTG measurement. The SDPTG index (d/a) was calculated from the wave component height, and was divided into quartiles (Q) according to the d/a value. The median follow-up period was 9.0 years. The d/a value was negatively associated with age and BP, and positively associated with heart rate and body height. Using the Cox proportional hazards model, the hazard ratios for cardiovascular mortality for Q2, Q3 and Q4 were significantly higher than that of Q1. In multivariate analysis, the hazard ratio was 2.30 for Q3 (95% confidence interval (CI): 1.06–4.99, P<0.05) and 2.60 for Q4 (95% CI: 1.21–5.60, P<0.05), after adjustment for age, height, body mass index, BP levels, heart rate and other atherosclerosis-related factors. The hazard ratios of cardiovascular mortality for Q3 and Q4 were significantly higher compared with the reference (Q1). Thus, the SDPTG d/a is an independent predictor of cardiovascular mortality in middle-aged and elderly Japanese women.
Similar content being viewed by others
Introduction
Noninvasive pulse wave analysis is useful for evaluating vascular load and vascular stiffness. Measurement of arterial function is important to determine the risk for cardiovascular diseases. The photoplethysmogram detects changes in the amount of light absorbed by hemoglobin, which reflects changes in blood volume. The finger photoplethysmogram is used to evaluate arterial compliance in relation to changes in the amplitude of the pulse wave. Aortic pressure can be divided into two components in the systolic phase: the early systolic component is mainly caused by left ventricular ejection, and the late component is augmented by reflection waves from periphery. Likewise, the digital pulse wave can be divided into two components in the systolic phase. Munir et al.1 showed that the digital late systolic pulse pressure component closely approximated to the central late systolic pressure component, and the digital peripheral pressure pulse wave was related to the digital volume pulse wave.2
The second derivative of the digital photoplethysmogram (SDPTG) was developed to recognize the inflection points of the photoplethysmogram with ease. SDPTG has a and b waves in the early part of systole, c and d waves in the latter part of systole, and the e wave in diastole (Figure 1). The ratio of the height of the d wave to the a wave of the SDPTG (d/a) has been considered to reflect the ascending aortic systolic pressure augmented by reflection waves from the periphery and functional peripheral vascular tension. Takazawa et al.3 showed that d/a reflected the augmentation index in the ascending aorta by simultaneously recorded SDPTG and the aortic pressure waveform.
Several investigations have been performed to assess the association between the SDPTG indices and age, hypertension, left ventricular hypertrophy, arteriosclerosis, metabolic syndrome-related factors and coronary risk parameters.4, 5, 6, 7, 8, 9, 10 To the best of our knowledge, no studies have attempted to determine the relationship between SDPTG and cardiovascular mortality in a large population using a longitudinal design. Therefore, the purpose of the present study was to determine the association between d/a as an index of SDPTG and cardiovascular mortality in middle-aged and elderly Japanese women.
Methods
Study population
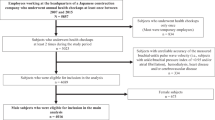
A total of 4727 women aged 50–79 years underwent a medical check-up, including a 75-g oral glucose tolerance test at the Hiroshima Atomic Bomb Casualty Council Health Management and Promotion Center between April 1998 and March 2008. They were followed up until December 2011. Participants with a history myocardial infarction, cardiovascular revascularization and cerebrovascular disease, and those with undergoing treatment for diabetes mellitus or a life-threatening illness were excluded. Subjects with an SDPTG waveform that could not be read were also excluded. Finally, 4373 subjects, mean age 68.1±6.6 years were recruited into this study. The mean follow-up period was 9.0±3.3 years (median 9.0 years).
Ethical considerations
The protocol of this study was approved by the Central Institutional Review Board of the Hiroshima Atomic Bomb Casualty Council Health Management and Promotion Center and Hiroshima University. Informed consent was obtained from the participants and their data were anonymized so that researchers could not identify the participants.
Definitions
Causes of death were ascertained based on death certificate information and medical records. Individual diagnoses were classified by ICD-9 (the International Classification of Diseases, 9th edition) codes. Cardiovascular disease was defined as the underlying cause of death with ICD-9 codes 401–438.
Measurements
At baseline, all participants were invited to undergo a medical check-up, including an oral glucose tolerance test after an overnight fast. Body weight and height were recorded. Brachial blood pressure (BP) was measured in the sitting position after a resting period of 15 min. Body mass index, calculated as body weight (kg)/square of height (m2), was used as a measure of obesity. Blood samples were drawn in the sitting position. Serum levels of total cholesterol and high-density lipoprotein (HDL) cholesterol were determined enzymatically with an autoanalyzer (7150, Hitachi, Japan). Blood samples were also collected for serum glucose determination in the 75-g oral glucose tolerance test. Diabetes was defined as a fasting glucose level ⩾126 mg dl−1 or a 2-h postload glucose tolerance test level ⩾200 mg dl−1. Glucose levels were determined by glucose oxidase methods. Assays for serum lipids were standardized using the Q-PAK Chemistry Control Serum 1 and 2 (Technicon Instrument Corp., New York, NY, USA). Estimated glomerular filtration rate (eGFR) was calculated using serum creatinine levels and age according to the MDRD (Modification of Diet in Renal Disease) formula modified for the Japanese population.11
SDPTG measurement
The SDPTG was measured using the automatic device FCP-4731 (Fukuda Denshi, Japan) in the supine position in the clinical laboratory at room temperature at 24–26 °C, as previously described.3, 7 The transducer was positioned at the cuticle of the second digit of the right hand. An example of the photoplethysmogram and SDPTG is shown in Figure 1.5 The SDPTG consists of four waves in systole (a, b, c and d waves) and one in diastole (e wave). The height of the a and d waves was measured from baseline, and the ratio of the height of the d wave to that of the a wave (d/a) was calculated.
Statistical analysis
Data are expressed as the mean±s.d. The d/a values were examined using quartiles, with the highest quartile (Q1) serving as the reference category. Quartiles were defined as follows: quartile 1 (Q1), −0.28 to 0; Q2, −0.35 to −0.29; Q3, −0.42 to −0.36; and Q4, −0.89 to −0.43. The relationship between d/a and cardiovascular risk factors was assessed using Pearson’s moment correlation coefficient. Univariate and multivariate regression analysis was performed to assess the linear association between d/a and clinical and cardiovascular disease-related parameters. For proportions, we used the χ2 statistic with Bonferroni correction of the probability values, as appropriate. One-way analysis of variance with Tukey’s test for multiple comparisons was used to examine differences between mean values in the quartiles. The outcome was cardiovascular mortality. The Kaplan–Meier method was used to estimate the unadjusted survival curves of the four groups, and comparisons were made using the log-rank test. Cox proportional hazards analysis was used to assess the association between d/a quartiles and study outcome. Hazard ratios (HRs) and 95% confidential intervals (CIs) were determined. All variables related to d/a and outcome measures were considered in the multivariate analysis. All analyses were performed with SAS version 9.3 for windows (SAS Institute Inc., Cary, NC, USA). A value of P<0.05 was considered significant.
Results
Baseline characteristics of the participants
The characteristics of the participants are shown in Table 1. The mean age at the baseline examination was 68.1±6.6 years, and d/a values ranged from −0.89 to 0, with a mean value of −0.36±0.10. A scattered plot between age and d/a are shown in Figure 2. In this population, the d/a value was significantly, inversely correlated with age (r=−0.172, P<0.0001). The d/a was positively correlated with body height (r=0.132, P<0.001) and heart rate (r=0.124, P<0.001), and negatively correlated with systolic BP (r=−0.140, P<0.001) and diastolic BP (r=−0.137, P<0.001). Body mass index, non-HDL cholesterol, fasting plasma glucose, smoking status and eGFR were not correlated with d/a. Univariate and multivariate regression analysis between d/a and clinical and cardiovascular disease-related parameters are shown in Table 2. In multivariate regression analysis, age, diastolic BP, body height, heart rate and body mass index were independently associated with d/a.
The baseline characteristics of the subjects in each d/a quartile are shown in Table 3. Age, systolic BP and diastolic BP significantly increased, and height and heart rate significantly decreased as the d/a value decreased. The percentage of current smoking was too small to determine any significant difference among the groups.
Cardiovascular mortality
Over a median follow-up of 9.0 years (39 732 person-years), there were 327 deaths, 79 of which were from cardiovascular disease. Figure 3 shows the event-free probabilities of cardiovascular mortality in the four groups. The Kaplan–Meier time-to-event curves for cardiovascular death were significantly different among the four groups (P=0.002).
In the Cox proportional hazard model, univariate analysis showed that the HR of cardiovascular mortality was 2.56 for Q2 (95% CI: 1.59–5.66, P<0.05), 2.96 for Q3 (95% CI: 1.37–6.39, P<0.01), and 4.17 for Q4 (95% CI: 1.97–8.85, P<0.001), using the Q1 group as reference. In multivariate analysis, the HR was 2.30 for Q3 (95% CI: 1.06–4.99, P<0.05) and 2.60 for Q4 (95% CI 1.21–5.60, P<0.05), after adjustment for age, body mass index, body height, diastolic BP, fasting plasma glucose, non-HDL cholesterol, eGFR, heart rate and smoking status. The HRs of cardiovascular mortality for Q3 and Q4 were significantly higher than that of the reference (Q1) (Table 4). The similarly significant HRs for Q3 (HR 2.30; 95% CI: 1.06–5.01, P<0.05) and Q4 (HR 2.69; 95% CI: 1.25–5.78, P<0.05) were obtained when systolic BP were used instead of diastolic BP for the adjustment.
Discussion
In this study with a median follow-up period of 9.0 years, d/a was found to be significantly associated with cardiovascular mortality in middle-aged and elderly Japanese women independently of age, BP levels and other atherosclerosis-related factors. Thus, d/a is a simple and useful index for predicting cardiovascular outcomes.
Several cross-sectional studies have been performed to assess the association between SDPTG and cardiovascular disease-related factors. The indices of SDPTG have been reported to be associated with vascular aging and hypertension.3, 4, 5, 6 The d/a was independently associated with coronary risk factors and the Framingham risk score in a Japanese community group,5 and with metabolic syndrome in male workers.6 In this study, d/a was significantly and negatively associated with age and BP. However, fasting plasma glucose, non-HDL-cholesterol and eGFR were not associated with d/a values. In addition, d/a was positively correlated with body height and heart rate, which is similar to the augmentation index.12, 13, 14 The augmentation index is a predictor of cardiovascular events, and high values have been reported to be associated with target organ damage.15 Takazawa et al. showed that a negative d/a reflected the systolic pressure augmented by reflection waves in the ascending aorta by simultaneously recording SDPTG and the aortic pressure waveform.3 They also indicated that d/a could be a useful marker of peripheral functional vascular tension and of the effect of vasodilator agents.3, 16 It has been reported that d/a was significantly correlated with the aortic augmentation index and related to left ventricular hypertrophy in patients with untreated hypertension.4 Increased arterial stiffness and augmented aortic pressure by wave reflection are independent predictors of cardiovascular events.17, 18, 19, 20 The central arterial augmentation index is generally greater in women than in men.21, 22, 23, 24, 25, 26, 27, 28 Left ventricular diastolic dysfunction and heart failure with a normal ejection fraction are relatively common in elderly women.29, 30, 31 In individuals with very stiff elastic arteries, such as hypertensive patients, aortic stiffness and aortic pressure augmented by reflection waves from the periphery accelerate left ventricular afterload and cause deterioration of left ventricular function. In the case of lower body height and small aortic diameter, such as in elderly women, earlier reflection waves to the heart from the periphery may augment the aortic pulse pressure. Severe arterial stiffness also accelerates the forward and backward speeds of the pulse wave. The pulse wave velocity is correlated with cardiovascular disease outcomes.32, 33, 34, 35, 36, 37 Therefore, the impact of augmented aortic pressure by wave reflection on left ventricular function may be increased.38 This study found that d/a was associated with cardiovascular mortality in middle-aged and elderly Japanese women, and indicated that d/a could have a role as a comparable marker of the aortic augmentation index. Smoking is a strong risk factor of arterial stiffness and coronary heart disease, and smoking also affects arterial dynamics.39, 40 However, the number of smokers was small in this cohort, therefore any effect of smoking was too small to determine a significant difference among the groups.
There are limitations in this study. The definition of cause of death was determined by information from death certificates, therefore the proportion of patients with cardiovascular disease may have been underestimated. Medication such as vasodilatory/vasoactive agents are known to potently affect aortic wave reflection and also alter d/a3. Information regarding medications for hypertension and dyslipidemia was not available in this study.
Further studies are required to compare other methodologies such as applanation tonometry devices to estimate central BP,41, 42 the augmentation index,43 and ambulatory arterial stiffness index44, 45 and indices of the echocardiogram in the determination of cardiovascular risk.
In conclusion, the present study showed that d/a of the SDPTG is significantly and independently associated with cardiovascular mortality in middle-aged and elderly Japanese women. We believe that d/a is a simple and noninvasive indicator of cardiovascular disease, and supports its important role in routine investigations in clinical practice.
References
Munir S, Guilcher A, Kamalesh T, Clapp B, Redwood S, Marber M, Chowienczyk P . Peripheral augmentation index defines the relationship between central and peripheral pulse pressure. Hypertension 2008; 51: 112–118.
Millasseau SC, Guigui FG, Kelly RP, Prasad K, Cockcroft JR, Ritter JM, Chowienczyk PJ . Noninvasive assessment of the digital volume pulse: comparison with the peripheral pressure pulse. Hypertension 2000; 36: 952–956.
Takazawa K, Tanaka N, Fujita M, Matsuoka O, Saiki T, Aikawa M, Tamura S, Ibukiyama C . Assessment of vasoactive agents and vascular aging by the second derivative of photoplethysmogram wave form. Hypertension 1998; 32: 365–370.
Iketani T, Iketani Y, Takazawa K, Yamashina A . The influence of the peripheral reflection wave on left ventricular hypertrophy in patients with essential hypertension. Hypertens Res 2000; 23: 451–458.
Otsuka T, Kawada T, Katsumata M, Ibuki C . Utility of second derivative of the finger photoplethysmogram for the estimation of the risk of coronary heart disease in the general population. Circ J 2006; 70: 304–310.
Kawada T, Otsuka T . Factor structure of indices of the second derivative of the finger photoplethysmogram with metabolic components and other cardiovascular risk indicators. Diabetes Metab J 2013; 37: 40–45.
Otsuka T, Kawada T, Katsumata M, Ibuki C, Kusama Y . Independent determinants of second derivative of the finger photoplethysmogram among various cardiovascular risk factors in middle-aged men. Hypertension Res 2007; 30: 1211–1218.
Hashimoto J, Chonan K, Aoki Y, Nishimura T, Ohkubo T, Hozawa A, Suzuki M, Matsubara M, Michimata M, Araki T, Imai Y . Pulse wave velocity and the second derivative of the finger photoplethysmogram in treated hypertensive patients: their relationship and associating factors. J Hypertens 2002; 20: 2415–2422.
Hashimoto J, Watanabe D, Kimura A, Takahashi H, Ohkubo T, Totsune K, Imai Y . Determinant of the second derivative finger photoplethysmogram and brachial-ankle pulse wave velocity; Ohasama study. Am J Hypertens 2005; 18: 477–485.
Imanaga I, Hara H, Koyanagi S, Tanaka K . Correlation between wave component of the second derivative of plethysmogram and arterial distensibility. Jpn Heart J 1998; 39: 775–784.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A Collaborators developing the Japanese equation for estimated GFR Binder J, Bailey KR, Seward JB, Squires RW, Kunihiro T, Hensrud DD, Kullo IJ . Aortic augmentation index is inversely associated with cardiorespiratory fitness in men without known coronary heart disease. Am J Hypertens 2006; 19: 1019–1024.
Reeve JC, Abhayaratna WP, Davies JE, Sharman JE . Central hemodynamics could explain the inverse association between height and cardiovascular mortality. Am J Hypertens 2014; 27: 392–400.
Rosenwasser RF, Shah NK, Smith SM, Wen X, Gong Y, Gums JG, Nichols WW, Chapman AB, Boerwinkle E, Johnson J, Epstein B . Baseline predictors of central aortic blood pressure: a PEAR substudy. J Am Soc Hypertens 2014; 8: 152–158.
Binder J, Bailey KR, Seward JB, Squires RW, Kunihiro T, Hensrud DD, Kullo IJ . Aortic augmentation index is inversely associated with cardiorespiratory fitness in men without known coronary heart disease. Am J Hypertens 2006; 19: 1019–1024.
Shimizu M, Kario K . Role of the augmentation index in hypertension. Ther Adv Cardiovasc Dis 2008; 2: 25–35.
Takazawa K, Fujita M, Yabe K, Saiki T, Maeda K, Yamashita Y, Hase M, Ibukiyama C . Clinical usefulness of the second derivative of photoplethysmogram (acceleration plethysmogram). J Cardiol 1993; 23: 207–217.
Vlachopoulos C, Aznaouridis K, O’Rourke MF, Safar ME, Baou K, Stefanadis C . Prediction of cardiovascular events and all-cause mortality with central haemodynamics; a systematic review and meta analysis. Eur Heart J 2010; 31: 1865–1871.
Weber T, Auer J, O’Rourke MF, Kvas E, Lassnig E, Berent R, Eber B . Arterial stiffness, wave reflection, and the risk of coronary artery disease. Circulation 2004; 109: 184–189.
London GM, Blacher J, Pannier B, Guerin AP, Marchais SJ, Safar ME . Arterial wave reflections and survival in end-stage renal failure. Hypertension 2001; 38: 434–438.
Mattace-Raso FU, van der Cammen TJ, Hofman A, van Popele NM, Bos ML, Schalekamp MA, Asmar R, Reneman RS, Hoeks AP, Breteler MM, Witteman JC . Arterial stiffness and risk of coronary heart disease and stroke: The Rotterdam Study. Circulation 2006; 13: 657–663.
Ayer JG, Harmer JA, Marks GB, Avolio A, Celermajer DS . Central arterial pulse wave augmentation is greater in girls than boys, independent of height. J Hypertens 2010; 28: 306–313.
Gatzka CD, Kingwell BA, Cameron JD, Berry KL, Liang YL, Dewar EM, Reid CM, Jennings GL, Dart AM . ANBO2 investigators. Australian comparative outcome trial of angiotensin converting enzyme inhibitor- and diuretic-based treatment of hypertension in the elderly. Gender differences in the timing of arterial wave reflection beyond differences in body height. J Hypertens 2001; 19: 2197–2203.
Russo C, Jin Z, Homma S, Rundek T, Elkind MS, Sacco RL, Di Tullio MR . Arterial stiffness and wave reflection: Sex differences and relationship with left ventricular diastolic function. Hypertension 2012; 60: 362–368.
Chirinos JA, Kips JG, Jacobs DR Jr, Brumback L, Duprez DA, Kronmal R, Bluemke DA, Townsend RR, Vemeersch S, Segers P . Arterial wave reflections and incident cardiovascular event heart failure: The Multiethnic Study of Atherosclerosis. J Am Coll Cardiol 2012; 60: 2170–2177.
Segers P, Rietzschel ER, Buyzere ML, Vermeersch SJ, Bacquer DD, Van Bortel LM, Backer GD, Gillebert TC, Verdonek GP, on behalf of the Asklepios Inveestigators. Noninvasive (input) impedance, pulse wave velocity, and wave reflection in healthy middle-aged men and women. Hypertension 2007; 49: 1248–1255.
Mitchell GF, Parise H, Benjamin EJ, Larson MG, Keyes MJ, Vita JA, Vasan RS, Levy D . Changes in arterial stiffness and wave reflection with advancing age in healthy men and women: Framingham Heart Study. Hypertension 2004; 43: 1239–1245.
Mitchell GF, Hwang S, Vasan RS, Larson MG, Pencina MJ, Hamburg NM, Vita JA, Levy D, Benjamin EJ . Arterial stiffness and cardiovascular events. The Framingham Heart Study. Circulation 2010; 121: 505–511.
Shim CY, Park S, Choi D, Yang WI, Cho IJ, Choi EY, Chung N, Ha JW . Sex Differences in central hemodynamic and their relationship to left ventricular diastolic function. J Am Coll Cardiol 2011; 57: 1226–1233.
Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM . Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med 2006; 355: 251–259.
Kitzman DW, Gardin JM, Gottdiener JS, Arnold A, Boineau R, Aurigemma G, Marino EK, Lyles M, Cushman M, Enright PL . Importance of heart failure with preserved systolic function in patients > or =65 years of age. CHS Research Group. Cardiovascular Health Study. Am J Cardiol 2001; 87: 413–419.
Devereux RB, Roman MJ, Liu JE, Welty TK, Lee ET, Rodeheffer R, Fabsitz RR, Howard BV . Congestive heart failure despite normal left ventricular systolic function in a population-based sample: the Strong Heart Study. Am J Cardiol 2000; 86: 1090–1096.
Laurent S, Boutouyrie P, Asmar R, Gautier I, Laloux B, Guize L, Ducimetiere P, Benetos A . Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension 2001; 37: 1236–1241.
Sutton-Tyrrell K, Samer S, Najjar SS, Boudreau RM, Venkitachalam L, Kupelian V, Simonsick EM, Havlik R, Lakatta EG, Spurgeon H, Kritchevsky S, Pahor M . Elevated aortic pulse wave velocity, a marker of arterial stiffness, predicts cardiovascular events in well-functioning older adults. Circulation 2005; 111: 3384–3390.
Willum-Hansen T, Staessen JA, Torp-Pedersen C, Rasmussen S, Thijs L, Ibsen H, Jeppesen J . Prognostic value of aortic pulse wave velocity as index of arterial stiffness in the general population. Circulation 2006; 113: 664–670.
Inoue N, Maeda R, Kawakami H, Shokawa T, Yamamoto H, Ito C, Sasaki H . Aortic pulse wave velocity predicts cardiovascular mortality in middle-aged men. Circ J 2009; 73: 549–553.
Syokawa T, Imazu M, Yamamoto H, Toyofuku M, Tasaki N, Okimoto T . Pulse wave velocity predicts cardiovascular mortality: Findings from the Hawaii-Los Angeles-Hiroshima study. Circ J 2005; 69: 259–264.
Otsuka K, Fukuda S, Shimada K, Suzuki K, Yoshiyama M, Yoshikawa J . Serial assessment of arterial stiffness by cardio-ankle vascular index for prediction of future cardiovascular events in patients with coronary artery disease. Hypertens Res 2014; 37: 1014–1020.
Zamani P, Jacobs DR Jr, Segers P, Duprez DA, Brumback L, Kronmal RA, Lilly SM, Townsend RR, Budoff M, Lima JA, Hannan P, Chirinos JA . Reflection magnitude as a predictor of mortality; the Multi-Ethnic Study of Atherosclerosis. Hypertension 2014; 64: 958–964.
Markus MR, Stritzke J, Baumeister SE, Siewert U, Baulmann J, Hannemann A, Schipf S, Meisinger C, Dorr M, Felix SB, Keil U, Volzke H, Hense HW, Schunkert H . MONICA/KORA Augsburg Cohort Study. Effects of smoking on arterial distensibility, central aortic pressures and left ventricular mass. Int J Cardiol 2013; 168: 2593–2601.
Tabara Y, Takahashi Y, Setoh K, Muro S, Kawaguchi T, Terao C, Kosugi S, Sekine A, Yamada R, Mishima M, Nakayama T, Matsuda F, on behalf of Nagahama Study Group. Increased aortic wave reflection and smaller pulse pressure amplification in smokers and passive smokers confirmed by urinary cotinine levels: Nagahama Study. Int J Cardiol 2013; 168: 2673–2677.
Miyashita H . Clinical assessment of central blood pressure. Curr Hypertens Rev 2012; 8: 80–90.
Seidlerova J, Filipovsky J, Mayer O, Wohlfahrt P, Cifkova R . Positive effects of antihypertensive treatment on aortic stiffness in the general population. Hypertens Res 2014; 37: 64–68.
Kelly R, Fitchett D . Noninvasive determination of aortic input impedance and external left ventricular power output: a validation and repeatability study of a new technology. J Am Coll Cardiol 1992; 20: 952–963.
Kollias A, Rarra V, Karpettas N, Roussias L, O’Brien E, Stergiou GS . Treatment-induced changes in ambulatory arterial stiffness index: one-year porspective study and meta-analysis of evidence. Hypertens Res 2015; 38: 627–631.
Laszlo A, Reusz G, Nemcsik J . Ambulatory arterial stiffness in chronic kidney disease: a methodological review. Hypertens Res 2016; 39: 192–198.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Inoue, N., Kawakami, H., Yamamoto, H. et al. Second derivative of the finger photoplethysmogram and cardiovascular mortality in middle-aged and elderly Japanese women. Hypertens Res 40, 207–211 (2017). https://doi.org/10.1038/hr.2016.123
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.123