Abstract
The aim of this clinical study was to evaluate the influence of aging on the levels of lipid peroxidation (quantified as thiobarbituric acid-reactive substances (TBARS) content), lipid hydroperoxide (LOOH), hexanoyl lysine (HEL), 8-iso-prostaglandin F2α (8-iso-PGF2α) and total antioxidant capacity (TAC), and determine their relationships to the demographic and cardiovascular risk factors in elderly hypertensive (HT) patients. This study consisted of four groups: two elderly groups with 30 HT patients (11 males, 19 females) and 30 normotensive healthy volunteers (15 males, 15 females), and two young groups with 30 HT patients (13 males, 17 females) and 30 normotensive healthy volunteers (12 males, 18 females). In the elderly control group, the TBARS, LOOH, HEL and 8-iso-PGF2α levels, and the carotid intima media thickness (CIMT) were significantly higher than in the young control group. The TBARS, LOOH, HEL and 8-iso-PGF2α levels and the CIMT measurements were significantly higher in the elderly HT group than in the young HT group. In addition, the TAC levels were significantly lower in the elderly and young HT groups than in the elderly and young control groups. The CIMT was significantly positively correlated with TBARS (r=0.40, P<0.001), HEL (r= 0.30, P=0.001), LOOH (r= 0.44, P<0.001) and 8-iso-PGF2α (r= 0.32, P<0.001) in all of the HT groups. It seems that in elderly patients, the LOOH and TBARS are better biomarkers of lipid peroxidation in hypertension in terms of sensitivity. In all of the HT groups, 8-iso-PGF2α had the highest sensitivity. Hypertension is associated with lipid peroxidation due to an impaired oxidant/antioxidant status. Increased lipid peroxidation and decreased antioxidants with aging indicate that peroxidative damage further increases with higher blood pressure and the aging process.
Similar content being viewed by others
Introduction
Aging is speculated to be a biological process characterized by a progressive decline in metabolic mechanisms and physiological functions. For example, the prevalence of hypertension considerably increases in the elderly. In addition, biological aging predisposes individuals to various morbidities through the age-related perturbation of the systemic oxidative balance, that is, uncontrolled reactive oxygen species (ROS) production. Oxidative damage and hypertension occur frequently in the elderly.1
Lipid peroxidation is a complex chain reaction process due to the oxygen-free radical- mediated attack on the cell membrane lipids, such as polyunsaturated fatty acids (PUFA), resulting in cell damage and dysfunction.2 Oxidative damage to lipid peroxidation has an important role in various diseases and aging processes. Thiobarbituric acid reactive substances (TBARS) are formed as a byproduct of lipid peroxidation, which can be detected by the TBARS assay using thiobarbituric acid as a reagent. During the early stages of lipid peroxidation, lipid hydroperoxides (LOOHs) are formed as a result of fatty acid oxidation. In addition, N-epsilon-hexanoyl-lysine (HEL) is a novel lipid peroxidation biomarker, which is derived from the oxidation of omega-6 unsaturated fatty acids.3 8-iso-prostaglandin F2α (8-iso-PGF2α) is an isoprostane that is produced by the non-enzymatic peroxidation of arachidonic acid in membrane phospholipids, and the measurement of it is a reliable tool for the identification of subjects with enhanced rates of lipid peroxidation.4 Cells, tissues and body fluids are equipped with powerful defense systems that help counteract oxidative challenge. Total antioxidant capacity (TAC) is commonly used to evaluate lipid peroxidation and antioxidant defenses in experimental and human hypertension. In recent years, several methods have been proposed to determine the TAC. The ferric reducing antioxidant power (FRAP) assay is a novel method that can be widely used for this purpose.5
Significant numbers of asymptomatic hypertensive patients are attacked by subclinical target organ damage, such as microalbuminuria and carotid atherosclerosis. Microalbuminuria is a predictor of cardiovascular events in patients with HT. Carotid intima-media thickness (CIMT), measured by ultrasonography, is a noninvasive test used to assess the presence of subclinical atherosclerosis. The relationships between endothelial dysfunction and increased CIMT in elderly hypertensive patients have been found in several studies.6 In addition, in another study conducted recently, there was an emphasis on the importance of early detection and control of systolic blood pressure for the prevention of atherosclerosis progression in hypertensive patients.7
No data are available concerning the possible association of the biomarkers of lipid peroxidation with aging in elderly hypertensive patients. Therefore, in the present study, our aim was to investigate the influence of aging on TBARS, LOOH, HEL, 8-iso-PGF2α, and the TAC levels and determine their relationships with demographical and cardiovascular risk factors in elderly hypertensive patients.
Materials and methods
Informed consent
The protocol for the sample collection was approved by the Istanbul University, Cerrahpasa Medicine Faculty Ethics Committee and was carried out according to the requirements of the Declaration of Helsinki. All of the patients were fully informed of the study procedures before they gave their consent.
Study population
Patients enrolled in the study were selected from Geriatrics and Internal Medicine outpatient clinics over a 1-year period from March 2013 to June 2014. A total of sixty patients who were 60 years and older were enrolled in the elderly groups and a total of 60 patients who were between the ages of 20–50 years were enrolled in the young groups. The elderly groups consisted of 30 HT patients (11 males, 19 females; age: 72.1±8.3) and 30 normotensive healthy volunteers (15 males, 15 females; age: 69.5±7.2), and the young groups consisted of 30 HT patients (13 males, 17 females; age: 43.2±3.6) and 30 normotensive healthy volunteers (12 males, 18 females; age: 42.1±4.2). The age limits of the study groups and the grouping of the various age limits were based on previously published literature.8, 9
The patients of the elderly and young HT groups who had been previously diagnosed and followed up in our outpatient clinic were selected from cases treated with calcium channel blockers and/or diuretics that are thought to have fewer antioxidant effects than the other antihypertensive therapies, such as angiotensin-converting enzyme inhibitors (ACEinh).10, 11 The elderly and young hypertensive groups were created homogeneously in terms of drug purchases. In the HT groups, 23 young and 22 elderly hypertensive patients were taking calcium channel blockers therapy, and 13 young and 15 elderly hypertensive patients were taking diuretics therapy.
The eligible subjects did not have any of the following: LDL >130 mg dl−1, diabetes mellitus, metabolic syndrome, body mass index >25 kg m−2, subjects with signs or symptoms of atherosclerotic vascular disease, malignancy, connective tissue diseases, endocrine diseases, smoking or alcoholism. Patients using drugs for HT and lipid metabolism, which could affect oxidative stress (statins, fibrates, angiotensin-converting enzyme inhibitors, angiotensin-receptor blockers, beta blockers and so on) were also excluded. The BMI of each subject was calculated using the following formula: weight (kg) per height (m)2.
The same doctor obtained brachial arterial pressures with a mercury sphygmomanometer (Riester Big Ben Round, Jungingen, Germany), which was standardized in accordance with the approval of American and British Hypertension Society and World Health Organization. The measurements were performed on three different occasions within a span of 5 days. The average of three measurements was taken as clinical systolic blood pressure (SBP) and diastolic blood pressure (DBP). Subjects with a blood pressure <130/80 mm Hg served as the control groups.
Ultrasonographic measurement of CIMT
The extracranial carotid arteries were examined using a standardized protocol. Ultrasonographic examinations were performed in a quiet, temperature-controlled room (22 °C). After 10 min of rest, the examinations were performed with a color Doppler ultrasound unit (ATL, Ultramark 9 HDI, Bothell, WA, USA) equipped with a 5–10-MHz transducer. All of the ultrasonographic measurements were performed and evaluated by a single radiologist blinded to the groupings of the patients. With the subjects in the supine position with a slight hyperextension of the neck, the common carotid arteries, carotid bulb and extracranial internal carotid arteries were identified. Two parallel echogenic lines separated by an anechoic space can be visualized at the level of the artery wall. It was previously shown that these lines were generated by the blood-intima and the media-adventitia interfaces.12 The distance between the two lines gives a reliable index. Ultrasound scans of the right and left distal centimeter of the common carotid arteries, the bifurcation and of the first proximal centimeter of the internal carotid arteries were performed to determine the CIMT. Because the far wall was better visualized than the near wall, the far-wall CIMT was calculated for each segment. In the presence of plaques, the wall thickness was never obtained at the level of plaque. The location, size, number and hemodynamic effects of the atherosclerotic plaques were determined with the help of grayscale, color Doppler and spectral Doppler ultrasound. All of the measurements were made at the time of scanning of the frozen images from the longitudinal scans using the machine’s electronic caliper.
Sample collection and measurements
After an overnight fast, in the morning (0800–0900 hours), blood and urine samples were collected at the same time. The blood samples were collected in EDTA-containing tubes and anticoagulant-free tubes. After centrifugation at 2500 × g for 5 min, the plasma and serum were separated for at least 30 min. Each sample (serum, plasma and urine) was divided into four aliquots, and the samples were stored at −80 °C until biochemical analysis.
The erythrocyte sedimentation rate was measured in the EDTA-blood samples using the Wintergreen method. Serum CRP levels were measured by the nephelometric method (Image 800 Beckman Coulter, Inc., Brea, CA, USA). The other biochemical parameters were measured using routine methods with commercial kits. Albumin excretion in the 24-h urine samples was measured using a Roche Hitachi P800 modular chemistry analyzer (Roche, Mannheim, Germany) with an ALBT2 microalbumin kit, and the mean value was calculated as the daily albumin excretion. An albumin excretion of⩽30 mg per 24 h was accepted as normoalbuminuria.
Measurements of the serum TBARS levels
Lipid peroxidation was measured as the amount of TBARS, and it was determined using the method described by Buege and Aust.13 The TBARS concentration was calculated using 1.56 × 105 (M−1 x cm−1) as a mole per liter extinction coefficient. The coefficients of the intra- and inter-assay variations were 2.3% (n=10) and 3.5% (n=10), respectively.
Measurements of the serum LOOH levels
Serum levels were measured using a commercially available colorimetric assay kit (Abnova, Walnut, CA, USA). The coefficients of the intra- and inter-assay variations were 3.8% (n=10) and 4.6% (n=10), respectively.
Measurements of the serum HEL levels
Serum HEL levels were measured by ELISA using a commercial kit (Northwest Life Science Specialties, Vancouver, WA, USA). The HEL studies were performed using a competitive immunoassay kit according to the manufacturer’s directions. The coefficients of the intra- and inter-assay variations were 4.8% (n=10) and 7.1% (n=10), respectively.
Measurements of the urine 8-iso-PGF2α levels
Urine 8-iso-PGF2α levels were measured using a commercially available competitive enzyme-linked immunoassay kit (Cell Biolabs, San Diego, CA, USA). The coefficients of the intra- and inter-assay variations were 5.1% (n=10) and 7.2% (n=10), respectively.
Measurements of the serum FRAP levels as an indicator of the TAC
The antioxidant status of the serum samples was evaluated using the FRAP assay.14 The modified FRAP assay uses reductant antioxidants in a redox-linked colorimetric method. In this assay, at low pH ferric-2,4,6-tripyridyl-s-triazine (FeIII-TPTZ) complex was reduced to the ferrous form, which was blue-colored and monitored by measuring the change in absorption at 593 nm. The change in absorbance is directly proportional to the reducing power of the electron-donating antioxidants present in the sample. Three hundred mmol per liter of acetate buffer (pH 3.6); 10 mmol l−1 2,4,6-tripyridyl-s-triazine (TPTZ) in 40 mmol l−1 HCl and 20 mmol l−1 FeCl3.6H2O in a ratio of 10:1:1 gave the working FRAP reagent. The Fe (II) standards were used. Fe (II) (1000 μmol l−1) is equivalent to 1000 μmol l−1 of the FRAP. Seven hundred and fifty microliters of working FRAP reagent was mixed with 25 μl of the supernatant or the standard in a test tube. The absorbance at 593 nm was recorded against the reagent blank. The absorbance change was converted into a FRAP value in mM by relating the change of absorbance at 593 nm of the test sample to that of a standard solution of a known FRAP value (3–0.375 mM). The coefficients of the intra- and inter-assay variations for the modified FRAP assay were 3.0% (n=10) and 4.6% (n=10), respectively.
Statistical analysis
A sample size of 30 patients per group was needed to achieve an 80% power at a two-sided alpha of 0.001 to detect the expected difference in the mean relative lipid peroxidation markers levels. The statistical analyses were performed using SPSS 20.0 software (SPSS, Chicago, IL, USA) for Windows. The difference in gender was analyzed by the chi-square test. The normal distribution of the data was tested using the one-sample Kolmogorov–Smirnov test. All of the statistical comparisons were performed using the analysis of variance (ANOVA) to compare the multiple-group means. The following post hoc evaluation was made by the Bonferroni method. All of the data were expressed as the mean±s.d. Pearson’s correlation was used for the numerical data. Spearman’s correlation was used for the nominal data. To evaluate the diagnostic accuracy, we carried out a receiver operating characteristic (ROC) curve analysis. The ROC curves were plotted to see the power of the oxidative stress biomarkers to differentiate the HT from the NT groups. The area under the curve (AUC) was then estimated with a 95% confidence interval. Values of P<0.05 were considered to be statistically significant.
Results
The general characteristics and laboratory findings of the studied groups are shown in Table 1. The lipid peroxidation parameters of the young and elderly groups are shown in Table 2.
The lipid peroxidation parameters of the control and hypertensive groups are shown in Table 3.
In all of the HT groups, age was significantly positively correlated with HEL (r=0.42, P<0.001), LOOH (r=0.44, P<0.001), TBARS (r=0.45, P<0.001), 8-iso-PGF2α (r=0.35, P<0.001) and CIMT (r=0.74, P<0.001) and significantly negatively correlated with TAC (r=−0.4, P=0.001). In addition, disease duration was significantly positively correlated with HEL (r=0.37, P=0.003), LOOH (r=0.39, P=0.002) and TBARS (r=0.25, P=0.04) in all of the HT groups. 8-iso-PGF2α was significantly positively correlated with TBARS (r=0.25, P=0.005), HEL (r=0.19, P=0.03) and LOOH (r=0.29, P=0.001), and significantly negatively correlated with TAC (r=−0.28, P=0.003) in all of the HT groups. In addition, the HEL was significantly positively correlated with LOOH and negatively correlated with TAC in all of the HT groups (r=0.50, P<0.001 and r=−0.31, P<0.001, respectively). In addition, in all of the HT groups, the CIMT was significantly positively correlated with TBARS (r=0.40, P<0.001), HEL (r=0.30, P=0.001), LOOH (r=0.44, P<0.001) and 8-iso-PGF2α (r=0.32, P<0.001) and significantly negatively correlated with TAC (r=−0.35, P<0.001).
In the young HT group, the TAC was significantly negatively correlated with LOOH (r=−0.4, P=0.002) and HEL (r=−0.3, P=0.02). 8-iso-PGF2α was significantly positively correlated with TBARS (r=0.27, P=0.035) in the young HT group. Particularly in the young HT group, the SBP values were significantly positively correlated with TBARS (r=0.4, P=0.001), LOOH (r=0.37, P=0.003) and 8-iso-PGF2α (r=0.47, P<0.001). The DBP values were significantly positively correlated with TBARS (r=0.3, P=0.02) and 8-iso-PGF2α (r=0.3, P=0.01) in the young HT group. In addition, in the young HT group, the CIMT measurement was significantly positively correlated with LOOH (r=0.52, P<0.001), 8-iso-PGF2α (r=0.33, P=0.01), SBP values (r=0.54, P<0.001) and DBP values (r=0.46, P<0.001).
In the elderly HT group, age was significantly positively correlated with TBARS (r=0.3, P=0.02) and DBP values (r=0.27, P=0.03). The HEL was significantly positively correlated with LOOH (r=0.40, P=0.002) and SBP values (r=0.30, P=0.02) in the elderly HT group. The SBP values were also significantly positively correlated with TBARS (r=0.37, P=0.003) and significantly negatively correlated with TAC (r=−0.27, P=0.03) in the elderly HT group.
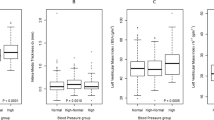
A comparison of the ROC curves with sensitivity, specificity, AUC, cutoff, and the asymptotic significance of TBARS, LOOH, HEL, 8-iso-PGF2α, TAC levels and the CIMT measurement in all HT groups is shown in Table 4 and Figures 1a and b. In addition, TBARS, LOOH and TAC had AUC values of 0.798 (P<0.001), 0.716 (P=0.004) and 0.204 (P<0.001), respectively, which demonstrate their sufficiency at distinguishing the elderly HT from the normotensive elderly control group (Figure 2a). When the ROC analyses were performed to test the power of these biomarker levels at distinguishing the young control and the young HT groups, the AUC levels of TBARS, LOOH, 8-iso-PGF2α and TAC were 0.759 (P=0.001), 0.809 (P<0.001), 0.904 (P<0.001), 0.362 (P=0.066), respectively (Figure 2b).
Discussion
Aging has been described as an independent risk factor for the development of cardiovascular disorders, such as atherosclerosis and hypertension. In addition, aging has been associated with the accumulation of lipid peroxides in the cell. Our results indicate that there is an increase in lipid peroxidation generation and a decrease in the TAC in elderly people compared with normal young subjects. The TBARS, LOOH, HEL and 8-iso-PGF2α levels, and the CIMT measurements were significantly higher in the elderly HT group than in the young HT group. In addition, age was significantly positively correlated with the TBARS, LOOH, HEL, 8-iso-PGF2α and CIMT, and significantly negatively correlated with the TAC in all of the HT groups. The increase in lipid peroxidation and the decrease in antioxidants with aging indicate that the peroxidative damage further increases with higher blood pressure and the aging process.
Oxidative damage to the lipids (lipid peroxidation) has an important role in various diseases and aging processes. Free radicals or nonradical species attack lipids containing carbon–carbon double bond(s), especially polyunsaturated fatty acids, which are a main target of oxidative attack, leading to the formation and accumulation of lipid oxidation products. The main primary products of lipid peroxidation are LOOHs;15 however, there are important problems in the determination of the indicators of lipid peroxidation. The lipid hydroperoxide assay kit used in our study measures the hydroperoxides, which directly utilizes the redox reactions with the ferrous ions. This procedure eliminates any interference caused by the hydrogen peroxide or endogenous ferric ions in the sample and provides a sensitive and reliable assay for lipid peroxidation.16
The TBARS, one of the end products of lipid peroxidation, was higher in the elderly HT group than in the elderly control group. In the young HT group, the TBARS levels were higher than in the young control group, which confirmed previous studies.15, 16, 17, 18, 19, 20, 21 In all of the HT groups, age, disease duration and the CIMT were positively correlated with the TBARS. The CIMT measurements were also significantly higher in the elderly HT group than in the young HT group, showing the relationship of the TBARS with the CIMT, which is a marker of cardiovascular disease related to aging. In addition, the SBP values were positively correlated with the TBARS in both the elderly and young hypertensive patients in the present study, while the LOOH levels offer a high sensitivity (80%) but a low specificity (54.3%). The ROC analysis revealed that the TBARS and LOOH were also the variables that had a significant effect on blood pressure in both the elderly and young hypertensive groups. This shows that elderly hypertensive patients are predisposed to increased free radical attacks due to lipid peroxidation. Kedziora-Kornatowska et al.22 demonstrated that the erythrocyte malondialdehyde levels, one of the end products of lipid peroxidation, were significantly higher in the hypertensive patients than in the young and elderly control groups. Our study along with the study of Kedziora-Kornatowska et al.22 confirm the exacerbation of lipid peroxidation in elderly patients, especially with associated primary hypertension.
The initial stage of the oxidative damage from biomolecules, such as proteins or aminolipids, may be required for the comprehension of aging and age-related diseases. The HEL is a novel lipid peroxidation biomarker, which is formed upon the oxidative modification of omega-6 fatty acids, such as linoleic acid, the predominant polyunsaturated fatty acid in the human diet and arachidonic acid.3 Tabak et al.23 have shown the relationship between hyperglycemia and lipid peroxidation; however, there were no significant differences in the HEL levels between the diabetic patients and the control groups. The presence of the HEL moiety in oxidized LDL (oxLDL) and human atherosclerotic lesions has been revealed by using a specific polyclonal antibody to the HEL moiety.24 In another study, an early oxidative stress marker, renal HEL accumulation, was observed in the Ang II-induced nephropathy model.25 No data are available concerning the possible association of HEL with aging and hypertension, but the HEL levels were higher in the elderly HT group than in the young HT group in the present study. The HEL was also positively correlated with the LOOH and SBP values in the elderly HT group. The results of our study show that HEL may be one of the early markers of lipid peroxidation in aging and hypertension.
We found increased levels of urine 8-iso-PGF2α in the elderly HT patients compared with the young HT group. In addition, the 8-iso-PGF2α was positively correlated with the TBARS, HEL, LOOH and CIMT and negatively correlated with the TAC in all of the HT groups. In addition, urine 8-iso-PGF2α had a higher sensitivity in the young HT group than in the elderly HT group, according to ROC analyzes that were performed separately in the elderly HT group, the young HT group and in all of the HT groups. However, 8-iso-PGF2α (85%) had the highest sensitivity in all of the HT groups. Hozawa et al.26 showed that the level of plasma 8-iso-PGF2α appeared to be elevated in older subjects with severe hypertension, while De Faria et al.27 demonstrated that the 8-iso-PGF2α levels were markedly higher in resistant hypertension (RHTN), compared with the HT patients. A significant inverse correlation was observed between the flow-mediated dilation and 8-iso-PGF2α in RHTN but not with the pulse wave velocity measurements. The multiple logistic regression analysis indicated that 8-iso-PGF2α is a significant predictor of endothelial dysfunction (flow-mediated dilation⩽median), adjusted for age, gender, BMI, presence of type 2 diabetes, aldosterone, SBP levels, LDL-cholesterol and smoking status, in the RHTN group. These results suggest that 8-iso-PGF2α may be an important therapeutic target for future intervention strategies and cardiovascular protection in RHTN. Rodrigo et al.28 demonstrated that the plasma and urine 8-iso-PGF2α levels were 36% and 32% higher, respectively, compared with the normotensive patients. There was a relationship between the SBP or DBP and the plasma and urine 8-iso-PGF2α levels. In addition, Wang et al.29 revealed a positive correlation between age and the 8-iso-PGF2α concentration in the patients with age-related cataracts and the controls. After the exclusion of the controls, the 8-iso-PGF2α concentrations correlated better with age in the case group. Cardiac oxidative stress, as measured by the production of cardiac and urinary 8-iso-PGF2α, was higher in 10-week-old spontaneously hypertensive rats compared with age-matched WistarKyoto rats and increased in 50-week-old spontaneously hypertensive rats.30 In summary, the present study and other clinical and experimental studies18, 26, 27, 28, 29, 30 demonstrate that 8-iso-PGF2α as a noninvasive index of oxidative stress may be a risk factor for hypertension and aging.
Antioxidants are substances that reduce the oxidation of other molecules due to oxygen and nitrogen, such as the reactions caused by free radicals. In a normal situation, a balanced equilibrium exists among oxidants, antioxidants and biomolecules; however, increased free radicals may defeat natural cellular antioxidant defenses, leading to lipid peroxidation and further contributing to organ damage. In the present study, the TAC levels were significantly lower in the elderly and young HT groups than in the elderly and young control groups. In addition, the SBP values were significantly negatively correlated with the TAC in the elderly HT group, while age and the CIMT were negatively correlated with the TAC in all of the HT groups. Circulating antioxidants might predict the aging conditions related to hypertension. Antioxidant scavengers can protect (particularly) cell membranes from the damaging effects of lipid oxidation and inhibit or delay the oxidation of a substrate in minutes. A lower total plasma antioxidant capacity was related to the presence of diabetes and arterial hypertension in a study by Da Cruz et al.,31 and the TAC levels decreased with age. Our study confirms other studies32, 33, 34, 35, 36, 37, 38 in that antioxidants may be used in order to reduce the production of lipid peroxidation in the cells and their harmful effects on the organism. However, whether antioxidant intake is beneficial and promotes helpful effects is still controversial.37, 38
Our study design utilized both young and elderly groups to search the effect of lipid peroxidation in the aging process and hypertension. Thus, we attentively studied the hypertensive patients who were taking antihypertensive medications because of age. The patients who were using calcium channel blockers and diuretics are specifically thought to show less of an antioxidant effect than the other groups (like ACEinh) that were included into the study.10, 11 However, in our study, the increased levels of the lipid peroxidation parameters of all of the HT groups whose tensions are regulated with calcium channel blockers and diuretic therapies suggest that these therapies may not be effective enough to prevent HT with the aging process. Additional larger studies are needed to evaluate the proper effects of these therapies on lipid peroxidation in the elderly HT patients because of our small numbers in the studied groups. Our results indicate that lipid peroxidation increases in both HT and the aging process. The maximum oxidative damage was observed in the elderly HT patients who have regulated blood pressures under an antihypertensive therapy for a long time.
Aging is a physiological process, but it also influences the deterioration of blood pressure. As a result of our study, HT may be triggered by a number of factors, and one of the most important influential factors is an association of the lipid peroxidation of oxidative stress and aging. Furthermore, the occurrence of oxidative stress due to increased lipid peroxidation contributes to the aging process; however, the rate of these deficiency statuses increases in the aging process, as does the deficiency in antioxidants. Antioxidants, such as hydrogen sulfide, may prevent the progression of aging related to hypertension, but the antioxidant effects of antihypertensive drugs on the oxidative stress of the aging process are yet not clear.39 In addition, it seems that the serum LOOH and TBARS levels are better biomarkers of lipid peroxidation in hypertensive elderly patients in terms of the sensitivity of HT. In addition, the 8-iso-PGF2α level (85%) had the highest sensitivity in all of the HT groups. More research is needed to understand how these biomarkers can help monitor oxidative stress in elderly hypertensive patients.
References
Saxena R . Arthritis as a disease of ageing and changes in antioxidant status. In: Preedy VR (ed), Aging: Oxidative Stress and Dietary Antioxidants, 1st edn. Academic Press Elsevier Publications: London. 2014, 49–59.
Ramana KV, Srivastava S, Singhal SS . Lipid peroxidation products in human health and disease 2014. Oxid Med Cell Longev 2014; 2014: 162414.
Sakai K, Kino S, Masuda A, Takeuchi M, Ochi T, Osredkar J, Rejc B, Gersak K, Ramarathnam N, Kato Y . Determination of HEL (Hexanoyl-lysine adduct): a novel biomarker for omega-6 PUFA oxidation. Subcell Biochem 2014; 77: 61–72.
Basu S . Fatty acid oxidation and isoprostanes: oxidative strain and oxidative stress. Prostaglandins Leukot Essent Fatty Acids 2010; 82: 219–225.
Sies H . Total antioxidant capacity: appraisal of a concept. J Nutr 2007; 137: 1493–1495.
Kong X, Jia X, Wei Y, Cui M, Wang Z, Tang L, Li W, Zhu Z, Chen P, Xu D . Association between microalbuminuria and subclinical atherosclerosis evaluated by carotid artery intimamedia in elderly patients with normal renal function. BMC Nephrol 2012; 13: 37–39.
Xie W, Liu J, Wang W, Wang M, Li Y, Sun J, Liu J, Qi Y, Zhao F, Zhao D . Five-year change in systolic blood pressure is independently associated with carotid atherosclerosis progression: a population-based cohort study. Hypertens Res 2014; 37: 960–965.
Reaven PD, Napoli C, Merat S, Witztumc JL . Lipoprotein modification and atherosclerosis in aging. Exp Gerontol 2000; 34: 527–537.
Seres I, Paragh G, Deschene E, Fulop T Jr, Khalil A . Study of factors influencing the decreased HDL associated PON1 activity with aging. Exp Gerontol 2004; 39: 59–66.
Dincer Y, Sekercioglu N, Pekpak M, Gunes KN, Akcay T . Assessment of DNA oxidation and antioxidant activity in hypertensive patients with chronic kidney disease. Ren Fail 2008; 30: 1006–1011.
Yoo SM, Choi SH, Jung MD, Lim SC, Baek SH . Short-term use of telmisartan attenuates oxidation and improves Prdx2 expression more than antioxidant β-blockers in the cardiovascular systems of spontaneously hypertensive rats. Hypertens Res 2015; 38: 106–115.
Pignoli P, Tremoli E, Poli A, Oreste P, Paoletti R . Intimal plus medial thickness of the arterial wall: a direct measurement with ultrasound imaging. Circulation 1986; 74: 1399–1406.
Buege JA, Aust SD . Microsomal lipid peroxidation. Methods Enzymol 1978; 52: 302–310.
Benzi IFF, Strain JJ . Ferric reducing/antioxidant power assay: direct measure of total antioxidant activity of biological fluids and modified version for simultaneous measurement of total antioxidant power and ascorbic acid concentration. Methods Enzymol 1999; 299: 15–27.
Uzun H, Karter Y, Aydin S, Curgunlu A, Simşek G, Yücel R, Vehiyd S, Ertürk N, Kutlu A, Benian A, Yaldiran A, Oztürk E, Erdine S . Oxidative stress in white coat hypertension; role of paraoxonase. J Hum Hypertens 2004; 18: 523–528.
Dominguez LJ, Galioto A, Pineo A, Ferlisi A, Ciaccio M, Putignano E, Belvedere M, Costanza G, Barbagallo M . Age, homocysteine, and oxidative stress: relation to hypertension and type 2 diabetes mellitus. J Am Coll Nutr 2010; 29: 1–6.
Kedziora-Kornatowska K, Szewczyk-Golec K, Czuczejko J, Pawluk H, van Marke de Lumen K, Kozakiewicz M, Bartosz G, Kedziora J . Antioxidative effects of melatonin administration in elderly primary essential hypertension patients. J Pineal Res 2008; 45: 312–317.
Sato K, Dohi Y, Kojima M, Miyagawa K, Takase H, Katada E, Suzuki S . Effects of ascorbic acid on ambulatory blood pressure in elderly patients with refractory hypertension. Arzneimittelforschung 2006; 56: 535–540.
Armas-Padilla MC, Armas-Hernández MJ, Sosa-Canache B, Cammarata R, Pacheco B, Guerrero J, Carvajal AR, Hernández-Hernández R, Israili ZH, Valasco M . Nitric oxide and malondialdehyde in human hypertension. Am J Ther 2007; 14: 172–176.
Akila VP, Harishchandra H, D'souza V, D'souza B . Age related changes in lipid peroxidation and antioxidants in elderly people. Indian J Clin Biochem. 2007; 22: 131–134.
Ahmad A, Singhal U, Hossain MM, Islam N, Rizvi I . The role of the endogenous antioxidant enzymes and malondialdehyde in essential hypertension. J Clin Diagn Res 2013; 7: 987–990.
Kedziora-Kornatowska K, Czuczejko J, Pawluk H, Kornatowski T, Motyl J, Szadujkis-Szadurski L, Szewczyk-Golec K, Kedziora J . The markers of oxidative stress and activity of the antioxidant system in the blood of elderly patients with essential arterial hypertension. Cell Mol Biol Lett 2004; 9: 635–641.
Tabak O, Gelisgen R, Erman H, Erdenen F, Muderrisoglu C, Aral H, Uzun H . Oxidative lipid, protein, and DNA damage as oxidative stress markers in vascular complications of diabetes mellitus. Clin Invest Med 2011; 34: E163–E171.
Kato Y, Mori Y, Makino Y, Morimitsu Y, Hiroi S, Ishikawa T, Osawa T . Formation of Nepsilon-(hexanonyl)lysine in protein exposed to lipid hydroperoxide. A plausible marker for lipid hydroperoxide-derived protein modification. J Biol Chem 1999; 274: 20406–20414.
Ichikawa D, Kamijo-Ikemori A, Sugaya T, Yasuda T, Hoshino S, Igarashi-Migitaka J, Hirata K, Kimura K . Renal liver-type fatty acid binding protein attenuates angiotensin II-induced renal injury. Hypertension 2012; 60: 973–980.
Hozawa A, Ebihara S, Ohmori K, Kuriyama S, Ugajin T, Koizumi Y, Suzuki Y, Matsui T, Arai H, Tsubono Y, Sasaki H, Tsuji I . Increased plasma 8-isoprostane levels in hypertensive subjects: the Tsurugaya Project. Hypertens Res 2004; 27: 557–561.
de Faria AP, Fontana V, Modolo R, Barbaro NR, Sabbatini AR, Pansani IF, Ferreira-Melo SE, Moreno H . Plasma 8-isoprostane levels are associated with endothelial dysfunction in resistant hypertension. Clin Chim Acta 2014; 433: 179–183.
Rodrigo R, Prat H, Passalacqua W, Araya J, Guichard C, Bächler JP . Relationship between oxidative stress and essential hypertension. Hypertens Res 2007; 30: 1159–1167.
Wang B, Zhu H, Sun H, Pan J, Yuan Z, Yu R . Plasma 8-isoprostane concentrations in patients with age-related cataracts. Clin Chem 2005; 51: 1541–1544.
Ito N, Ohishi M, Yamamoto K, Tatara Y, Shiota A, Hayashi N, Komai N, Yanagitani Y, Rakugi H, Ogihara T . Renin-angiotensin inhibition reverses advanced cardiac remodeling in aging spontaneously hypertensive rats. Am J Hypertens 2007; 20: 792–799.
Da Cruz AC, Petronilho F, Heluany CC, Vuolo F, Miguel SP, Quevedo J, Romano-Silva MA, Dal-Pizzol F . Oxidative stress and aging: correlation with clinical parameters. Aging Clin Exp Res 2014; 26: 7–12.
Okoduwa SI, Umar IA, Ibrahim S, Bello F, Habila N . Age-dependent alteration of antioxidant defense system in hypertensive and type-2 diabetes patients. J Diabetes Metab Disord 2015; 14: 32.
Goraca A . Assessment of total antioxidant capacity in human plasma. Folia Med (Plovdiv) 2004; 46: 16–21.
Cao G, Russell RM, Lischner N, Prior RL . Serum antioxidant capacity is increased by consumption of strawberries, spinach, red wine or vitamin C in elderly women. J Nutr 1998; 128: 2383–2390.
Gawron-Skarbek A, Chrzczanowicz J, Kostka J, Nowak D, Drygas W, Jegier A, Kostka T . Cardiovascular risk factors and total serum antioxidant capacity in healthy men and in men with coronary heart disease. Biomed Res Int 2014; 2014: 216964.
Iversen PO, Ha L, Blomhoff R, Hauge T, Veierød MB . Baseline oxidative defense and survival after 5-7 years among elderly stroke patients at nutritional risk: Follow-up of a randomized, nutritional intervention trial. Clin Nutr 2015; 34: 775–778.
Fusco D, Colloca G, Lo Monaco MR, Cesari M . Effects of antioxidant supplementation on the aging process. Clin Interv Aging 2007; 2: 377–387.
Henríquez-Sánchez P, Sánchez-Villegas A, Ruano-Rodríguez C, Gea A, Lamuela-Raventós RM, Estruch R, Salas-Salvadó J, Covas MI, Corella D, Schröder H, Gutiérrez-Bedmar M, Santos-Lozano JM, Pintó X, Arós F, Fiol M, Tresserra-Rimbau A, Ros E, Martínez-González MA, Serra-Majem L . Dietary total antioxidant capacity and mortality in the PREDIMED study. Eur J Nutr, (e-pub ahead of print 7 February 2015)..
Magableh MR, Kemp-Harper BK, Hart JL . Hydrogen sulfide treatment reduces blood pressure and oxidative stress in angiotensin II-induced hypertensive mice. Hypertens Res 2015; 38: 13–20.
Acknowledgements
This work was supported by the Research Fund of Istanbul University (Project Number: 30184).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Yavuzer, H., Yavuzer, S., Cengiz, M. et al. Biomarkers of lipid peroxidation related to hypertension in aging. Hypertens Res 39, 342–348 (2016). https://doi.org/10.1038/hr.2015.156
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.156
Keywords
This article is cited by
-
Lipofuscin, amyloids, and lipid peroxidation as potential markers of aging in Daphnia
Biogerontology (2023)
-
Spectroscopic analysis of breath ethylene and oxidative stress relation with glycaemic status in type 2 diabetes
Optical and Quantum Electronics (2017)