Abstract
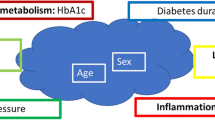
Arterial stiffness is an independent predictor of vascular morbidity and mortality in patients with atherosclerosis. Angiographic score (ASc) reflects severity of atherosclerosis in patients with peripheral arterial disease (PAD). Osteopontin (OPN) and oxidized low-density lipoprotein (oxLDL) are involved in the pathogenesis of atherosclerosis. The aim of the present study was to evaluate the association between arterial stiffness, ASc, serum OPN and oxLDL in patients with symptomatic PAD, and in clinically healthy subjects. We studied 79 men with symptomatic PAD (mean age 64±7 years) and 84 healthy men (mean age 63±8 years). Calculation of the ASc was based on severity and location of atherosclerotic lesions in the arteries of the lower extremities. Aortic pulse wave velocity (aPWV) was evaluated by applanation tonometry using the Sphygmocor device. Serum OPN and oxLDL levels were determined by enzyme-linked immunosorbent assay. The aPWV (10±2.4 VS. 8.4±1.7 (m s−1); P<0.001), OPN (75 (62.3–85.8) VS. 54.8 (47.7–67.9) (ng ml−1); P<0.001) and oxLDL (67 (52.5–93.5) VS. 47.5 (37–65.5); P<0.001) were different for the patients and for the controls. In multiple regression models, aPWV was independently determined by ASc, log-OPN, log-oxLDL and estimated glomerular filtration rate in the patients (R2=0.44; P<0.001) and by log-OPN, log-oxLDL, age and heart rate in the controls (R2=0.38; P<0.001). The independent relationship of a PWV with serum levels of OPN and oxLDL in the patients with PAD and in the controls indicates that OPN and oxLDL might influence arterial stiffening in patients with atherosclerosis and in clinically healthy subjects.
Similar content being viewed by others
Introduction
Arterial stiffness is an independent determinant of cardiovascular risk and a strong contributor to atherosclerosis.1 Increased arterial stiffness is associated with coronary artery disease,2 carotid atherosclerosis3 and peripheral arterial disease (PAD).4 Aortic pulse wave velocity (aPWV) is a well-established marker of arterial stiffness and predicts cardiovascular events in general population and in patients with atherosclerosis.1, 4
Osteopontin (OPN) is a glycoprotein that has been implicated in the pathogenesis of atherosclerosis.5 The OPN is expressed in atherosclerotic plaques, and stimulates recruitment of macrophages and production of inflammatory cytokines.6 Serum OPN level is related to the presence and extent of coronary artery disease,7 and is an independent predictor of adverse cardiovascular events in patients with chronic stable angina.8
High-grade oxidative stress is another important factor in progression of atherosclerosis. Profound oxidative stress contributes to endothelial dysfunction9 and arterial stiffening.10, 11 Oxidized low-density lipoprotein (oxLDL) is a marker of oxidative stress, which is associated with the presence of atherosclerotic lesions in different parts of the vasculature system.11
Angiographic score (ASc) assessed by digital subtraction angiography provides information about distribution and severity of atherosclerotic lesions in the arteries of the lower extremities.12 The ASc is inversely related to ankle-brachial pressure index (ABPI) and maximum walking distance,13 and is positively associated with biomarkers of inflammation13 and oxidative stress14 in patients with atherosclerosis.
Animal models indicate that OPN could contribute to initiation and progression of atherosclerosis.15 However, no studies have examined the potential association of serum OPN with aortic stiffness and ASc in patients with atherosclerosis. Moreover, there exist only limited data about associations of aortic stiffness with anatomic distribution of atherosclerotic lesions and serum oxLDL. The main aim of the present study was to investigate the relationship between aPWV and serum levels of OPN and oxLDL in patients with symptomatic PAD and in healthy subjects. In addition, we evaluated the association between aPWV and ASc in patients with atherosclerosis.
Materials and methods
Study population
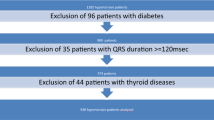
The study population comprised of 79 men (mean age 64±7 years) with symptomatic PAD. The patients were recruited from the Department of Vascular Surgery, Tartu University Hospital, Tartu, Estonia. All patients had ABPI <0.9. The patients had stage II (n=54), III (n=17) or IV (n=8) of chronic ischemia as defined by Fontaine: stage II=intermittent claudication; stage III=leg pain at rest; stage IV=focal tissue necrosis or gangrene. Patients were excluded if they had had myocardial infarction, coronary revascularization or cerebrovascular events during the previous 6 months, earlier revascularization procedures at the lower limb, upper limb occlusive arterial disease, atrial fibrillation, valve pathologies, known inflammatory conditions, diabetes mellitus, malignancies and renal failure (estimated glomerular filtration rate (eGFR) <60 ml min−1 per 1.73 m2). Overall, 31 (39%) patients with hypertension and 12 (15%) patients with coronary artery disease were included in the study. A significant proportion of the patients used concomitant medications: 32 patients received pentoxifylline, 21 patients used aspirin, 9 patients were treated with statins, 15 patients were treated with angiotensin-converting enzyme inhibitors, 15 patients used calcium channel blockers, 8 patients were treated with angiotensin-receptor blockers, 6 patients used beta-blockers, and 3 patients received diuretics.
A total of 84 clinically healthy men (mean age 63±8 years) were recruited by a family physician and by a specialist of sports medicine. The exclusion criteria for the control group were the following: coronary artery disease, cardiac arrhythmias or valve pathologies, cerebral or peripheral atherosclerotic disease, diabetes mellitus, malignancies, renal failure (eGFR <60 ml min−1 per 1.73 m2) and known inflammatory conditions. The control subjects did not use any medications on a regular basis. The study complies with the Declaration of Helsinki. The study protocol was approved by the Ethics Committee of the University of Tartu. All subjects gave written informed consent.
Hemodynamic measurements
Brachial blood pressure (BP) and heart rate were recorded in the supine position from the left arm with an automated digital oscillometric BP monitor (OMRON M4-I; Omron Healthcare Europe, Hoofdorp, The Netherlands). Radial artery pressure waveforms were obtained with a high-fidelity applanation tonometer (SPT-301B; Millar Instruments, Houston, TX, USA) from the wrist of the left hand. Pulse wave analysis (SCOR Px, 7.0; AtCor Medical, Sydney, Australia) was then used to generate a corresponding central (ascending aortic) waveform using a generalized transfer function, which has been prospectively validated for assessment of ascending aortic BP.16 Augmentation index (AIx), mean arterial pressure, central systolic BP, central diastolic BP and central pulse pressure were determined by pulse wave analysis. The AIx was calculated as the difference between the second and the first systolic peaks, divided by pulse pressure and expressed in percentages.17 The AIx values were adjusted to a heart rate of 75 beats per minute (AIx@75) using a SphygmoCor built-in algorithm. The within- and between-observer coefficients of variation for AIx@75 were 3.4 and 7.1%, respectively. Pulse wave velocity (PWV) was measured by the foot-to-foot method, using the same device. The aortic PWV (aPWV) was determined by sequentially recording electrocardiogram-gated carotid and femoral artery waveforms, as described in detail previously.17 The within- and between-observer coefficients of variation for aPWV were 2.3 and 6.2%, respectively. Brachial PWV (bPWV) was measured from carotid and radial waveforms. The within- and between-observer coefficients of variation for bPWV were 2.9 and 5.5%, respectively. All measurements were made in duplicate by two trained investigators, and the mean values were used in subsequent analysis.
The ABPI was measured using the Bidirectional Doppler MD 6 (D.E, Hokanson, Bellevue, WA, USA). Systolic BP was assessed bilaterally over the brachial, tibialis posterior and dorsalis pedis arteries. The higher systolic BP of the dorsalis pedis or the posterior tibial artery was used for calculation of the ABPI.12 Two readings of the ABPI were performed and the mean was calculated. The lower ABPI of the two legs was included in the statistical analysis. The within- and between observer coefficients of variation for ABPI were 4.1 and 8.6%, respectively.
Angiographic score
All patients were examined with digital subtraction angiography (Axiom Artis, Siemens Medical Solutions, Forchheim, Germany) of the aorta and the arteries of the lower extremities using the standard technique via the femoral approach at the Department of Radiology, Tartu University Hospital, Tartu, Estonia. In the majority of the PAD patients, digital subtraction angiography was followed by percutaneous transluminal angioplasty with stenting or by bypass surgery. In some patients, conservative treatment was chosen owing to concomitant diseases and the high risk of surgery. The following arterial segments were evaluated: abdominal aorta, common iliac artery, external iliac artery, common femoral artery, profunda femoris artery, superficial femoral artery, popliteal artery, tibio-peroneal trunk, anterior tibial artery, posterior tibial artery and peroneal artery. Severity of stenosis was assessed according to the following validated grading system: 0=normal; 1=stenosis <50%; 2=stenosis >50%; 3=occlusion.13 Different scores for each of the 21 segments were then added up to obtain an angiographic score for each patient, 63 being the maximal score. The angiographic score was evaluated independently by an experienced radiologist, who was blinded to the results of hemodynamic and laboratory measurements. The within-observer coefficient of variation for ASc was 5.4%.
Blood sample analysis
Venous blood samples were drawn in the morning after an overnight fasting. Serum OPN levels were measured using an enzyme-linked immunosorbent assay (R&D Systems, Minneapolis, MN, USA). The intra- and interassay coefficients of variation for OPN were 4.0 and 6.6%, respectively. Serum oxLDL levels were determined by enzyme-linked immunosorbent assay (Mercodia AB, Uppsala, Sweden). The intra- and interassay coefficients of variation for oxLDL were 5.5 and 6.2%, respectively. Biochemical parameters, such as glucose, LDL-cholesterol, HDL-cholesterol, triglycerides, creatinine and high-sensitivity C-reactive protein were measured according to standardized protocols in the local clinical laboratory. Calculation of eGFR was performed using the Modification of Diet in Renal Disease formula, equation MDRD 1.18
Study protocol
All subjects were studied between 0800 and 1000 h after an overnight fast in a quiet temperature-controlled room. First, body weight and height were measured to calculate the body mass index. After 15 min of rest in the supine position, brachial BP and radial artery waveforms were recorded in all subjects. Then aPWV, bPWV, AIx@75 and ABPI were determined. Blood (20 ml) was drawn from the cubital vein into plain tubes. Further, the patients underwent routine digital subtraction angiography of the aorta and the arteries of the lower extremities.
Statistical analysis
Software STATISTICA (version 10.0 for Windows; StatSoft, Tulsa, OK, USA) was used for all statistical analyses. Continuous variables are shown as a mean±s.d. Categorical variables are presented in percentages. The Kolmogorov–Smirnov test was performed to prove variables for normal distribution. Because of the skewed distribution of OPN and oxLDL, logarithmic transformation was performed before statistical analysis. Owing to a significant difference in BP between the study groups, aPWV and bPWV were adjusted for mean arterial pressure before analysis. Correlations between continuous variables were quantified using Pearson’s correlation coefficient. Multiple regression analysis was performed to investigate the independent determinants of aPWV. P-values of <0.05 were considered statistically significant.
Results
Participant characteristics
The baseline characteristics of the study population are shown in Table 1. The groups did not differ with respect to age or body mass index. The patients with PAD had higher aPWV, AIx@75, heart rate, as well as measures of peripheral and central BP. By contrast, ABPI was significantly higher among the controls. Biomarkers of inflammation and oxidative stress, such as high-sensitivity C-reactive protein, OPN and oxLDL, were higher in the patient group.
Determinants of arterial stiffness
The aPWV was positively correlated with ASc (Figure 1) and negatively with ABPI (Table 2) for the patient group. The aPWV correlated significantly with log-OPN (Figure 2a) and oxLDL (Figure 2b) in the patients with PAD and in the controls. Moreover, aPWV was significantly correlated with age, bPWV and eGFR in the patients and in the controls (Table 2). In multiple regression analysis, aPWV was independently associated with ASc, log-OPN, log-oxLDL and eGFR in the patients (R2=0.44, P<0.001), and with age, log-oxLDL, heart rate and log-OPN in the controls (R2=0.38, P<0.001) (Table 3). These associations persisted after correction for pack years of smoking, ABPI, BMI, LDL-cholesterol, HDL-cholesterol, triglycerides, glucose, heart rate and log-high-sensitivity C-reactive protein. As shown in Figure 3, higher levels of OPN and oxLDL were related to higher aPWV values in both study groups. We did not find any association between bPWV and ASc in the patients with PAD (r=−0.01, P=0.95). Moreover, neither bPWV nor AIx@75 was correlated with ABPI, log-oxLDL, or log-OPN in either of the study groups (data not shown).
Correlation between aPWV and log-OPN for the patients (r=0.39, P<0.001) and for the control subjects (r=0.41, P<0.001) (a). Correlation between aPWV and log-oxLDL for the patients (r=0.28, P=0.01) and for the control subjects (r=0.26, P=0.02) (b). The aPWV has been adjusted for mean arterial pressure (MAP). Filled dots represent patients; empty dots represent controls. Continuous line represents regression line through the patient data; interrupted line represents regression line through the control data.
Determinants of biomarkers and angiographic score
In the patients with PAD, log-OPN was significantly correlated with ASc (r=0.29, P=0.01), ABPI (r=−0.32, P=0.007) and age (r=0.25, P=0.03). Moreover, a trend towards correlation was observed between log-OPN and log-oxLDL (r=0.22, P=0.058) for the patient group. In the healthy subjects, log-OPN was correlated with age (r=0.43, P<0.001) but not with ABPI (r=−0.02, P=0.98). The log-oxLDL correlated significantly with LDL (r=0.51, P<0.001) in the PAD patients, and with weight (r=0.25, P=0.03) and LDL (r=0.43, P<0.001) in the controls. Furthermore, ASc was correlated with ABPI (r=−0.35, P=0.004).
Discussion
We demonstrated that arterial stiffness was independently associated with serum levels of OPN and oxLDL in the patients with PAD, as well as in the healthy subjects. To the best of our knowledge, this is the first study which investigated the relationship between serum OPN and aPWV in patients with symptomatic PAD in comparison with clinically healthy subjects. These results suggest that OPN and oxLDL might influence arterial stiffening in atherosclerosis and in healthy individuals. Moreover, aPWV was independently associated with ASc in the PAD patients. This finding could suggest that aortic stiffness is related to the distribution and severity of atherosclerotic lesions in the lower extremity arteries in patients with the established diagnosis of PAD.
A recent cross-sectional study has shown an independent relationship between aPWV and OPN in patients with rheumatoid arthritis.19 Similarly, we observed an independent association between serum OPN and aPWV in patients with PAD and in healthy subjects. There are several possible explanations for these findings. Data from animal models indicate that OPN modulates proliferation of the vascular smooth muscle and thickening of the media,20 which may increase arterial stiffness. Moreover, OPN stimulates production of matrix metalloproteinases, which are associated with degradation of elastic fibers and further increase in arterial stiffness.21 Alternatively, the relationship between OPN and arterial stiffness might be influenced by vascular calcification. The OPN is an important inhibitor of vascular calcification.21 As PAD is associated with vascular calcification,22, 23 it might be that increased serum OPN represents a compensatory mechanism aiming to inhibit progression of vascular calcification. However, further experimental studies are needed to determine the exact role of OPN in arterial stiffening.
A growing body of evidence suggests that OPN has a major role in atherosclerotic plaque formation. A recent longitudinal study demonstrated that OPN levels predict cardiovascular death, myocardial infarction, stroke and endovascular interventions in patients undergoing carotid surgery.24 In our study, serum OPN was correlated with ABPI in the patients with atherosclerosis, but not in the controls. These findings suggest that serum OPN may be a marker of atherosclerotic burden in patients with PAD, but not in apparently healthy individuals.
High-grade oxidative stress is another important contributor to the pathogenesis of cardiovascular disease.25 Previously, we have demonstrated the relationship between urinary 8-iso-prostaglandin F2a concentration and the indices of arterial elasticity in patients with PAD.10 In the present study, we extended our previous findings by demonstrating an independent association between oxLDL and aPWV, the ‘gold standard’ measure of arterial stiffness in the patients with PAD and in healthy subjects. It may be possible that high-grade oxidative stress stimulates hypertrophy of vascular smooth cells, which would lead to an increase in arterial stiffness.26 However, the exact mechanisms underlying the association between aPWV and oxLDL need to be clarified in further studies.
Arterial stiffness is related to atherosclerosis at different sites in the arterial tree. Results from a longitudinal study demonstrate that aPWV is an independent predictor of coronary events in patients with essential hypertension.2 Furthermore, arterial stiffness is strongly associated with carotid intima-media thickness4 and ABPI27 in elderly subjects. In the present study, aPWV was independently associated with ASc in patients with atherosclerosis. This finding suggests that arterial stiffening might be involved in the pathogenesis of PAD. However, owing to the cross-sectional design of this study, it is not possible to infer that the association between arterial stiffness and atherosclerosis is causal.
The relationship between increased arterial stiffness and atherosclerosis could be potentially explained by several mechanisms. First, arterial stiffening leads to an increase in pulse pressure and could influence progression of the atherosclerotic process.2 Second, presence of calcified plaques in the aorta may increase arterial stiffness.22 Third, both arterial stiffening and atherosclerosis might be the consequences of aging.26 Age-related arterial stiffening is characterized by fibrosis, degradation of elastic fibers and hypertrophy of vascular smooth cells.26 All these morphological changes accelerate progression of the atherosclerotic process. Fourth, endothelial dysfunction might mediate the relationship between atherosclerosis and arterial stiffness. In patients with atherosclerosis, a reduction in the synthesis of nitric oxide increases vascular tone, which in turn leads to an increase in arterial stiffness.26
It has been demonstrated that stiffness of the peripheral conduit arteries has no predictive value in patients with end-stage renal disease.28 Additionally, we did not observe any association between bPWV and ASc, or between bPWV and ABPI in patients with atherosclerosis. The lack of association between bPWV and indices of severity of atherosclerosis might be related to the fact that PAD mainly affects stiffness of the aorta and the arteries of the lower rather than the upper extremities.12
The present study has several limitations. First, as it was a cross-sectional study, we cannot establish causal relationship between arterial stiffness, OPN, oxLDL and atherosclerosis. Second, all study participants were men. Therefore, our results cannot be extrapolated to women. Third, as the sample size was relatively small, the results of our study should be verified in large-scale investigations. Finally, a substantial proportion of the study participants used cardiovascular medications, which might have affected the results of hemodynamic measurements.
In summary, our findings provide evidence that aPWV is independently associated with serum levels of OPN and oxLDL in patients with lower extremity atherosclerosis and in healthy individuals. The OPN and oxLDL may have an important role in arterial stiffening in patients with atherosclerosis and in clinically healthy individuals. Furthermore, aPWV is related to ASc in the PAD patients, suggesting that aortic stiffness is related to atherosclerosis in the lower extremity arteries.
References
Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, Pannier B, Vlachopoulos C, Wilkinson I, Struijker-Boudier H . European Network for non-invasive investigation of large arteries. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 2006; 27: 2588–2605.
Boutouyrie P, Tropeano A, Asmar R, Gautier I, Benetos A, Lacolley P, Laurent S . Aortic stiffness is an independent predictor of primary coronary events in hypertensive patients: a longitudinal study. Hypertension 2002; 39: 10–15.
Agabiti-Rosei E, Muiesan M . Carotid atherosclerosis, arterial stiffness and stroke events. Adv Cardiol 2007; 44: 173–186.
Van Popele N, Grobbee D, Bots M, Asmar R, Topouchian J, Reneman R, Hoeks A, van der Kuip D, Hofman A, Witteman J . Association between arterial stiffness and atherosclerosis: the Rotterdam study. Stroke 2001; 32: 454–460.
Kurata M, Okura T, Kumon Y, Tagawa M, Watanabe H, Nakahara T, Miyazaki T, Higaki J, Nose M . Plasma thrombin-cleaved osteopontin elevation after carotid artery stenting in symptomatic ischemic stroke patients. Hypertens Res 2012; 35: 207–212.
Scatena M, Liaw L, Giachelli C . Osteopontin: a multifunctional molecule regulating chronic inflammation and vascular disease. Arterioscler Thromb Vasc Biol 2007; 27: 2302–2309.
Ohmori R, Momiyama Y, Taniguchi H, Takahashi R, Kusuhara M, Nakamura H, Ohsuzu F . Plasma osteopontin levels are associated with the presence and extent of coronary artery disease. Atherosclerosis 2003; 170: 333–337.
Minoretti P, Falcone C, Calcagnino M, Emanuele E, Buzzi M, Coen E, Geroldi D . Prognostic significance of plasma osteopontin levels in patients with chronic stable angina. Eur Heart J 2006; 27: 802–807.
Heitzer T, Schlinzig T, Krohn K, Meinertz T, Münzel T . Endothelial dysfunction, oxidative stress, and risk of cardiovascular events in patients with coronary artery disease. Circulation 2001; 104: 2673–2678.
Kals J, Kampus P, Kals M, Zilmer K, Kullisaar T, Teesalu R, Pulges A, Zilmer M . Impact of oxidative stress on arterial elasticity in patients with atherosclerosis. Am J Hypertens 2006; 19: 902–908.
Madamanchi N, Vendrov A, Runge M . Oxidative stress and vascular disease. Arterioscler Thromb Vasc Biol 2005; 25: 29–38.
Hirsch A, Haskal Z, Hertzer N, Bakal C, Creager M, Halperin J, Hiratzka L, Murphy W, Olin J, Puschett J, Rosenfield K, Sacks D, Stanley J, Taylor L, White C, White J, White R, Antman E, Smith S, Adams C, Andreson J, Faxon D, Fuster V, Gibbons R, Halperin J, Hunt S, Jacobs A, Nishimura R, Ornato J, Page R, Riegel B . ACC/AHA 2005 Guidelines for the management of patients with peripheral arterial disease. J Am Coll Cardiol 2006; 47: e1–e192.
Nylaende M, Kroese A, Stranden E, Morken B, Sandbaek G, Lindahl A, Arnesen H, Seljeflot I . Markers of vascular inflammation are associated with the extent of atherosclerosis assessed as angiographic score and treadmill walking distances in patients with peripheral arterial occlusive disease. Vasc Med 2006; 11: 21–28.
Basarici I, Altekin R, Demir I, Yilmaz H . Urinary 8-isoprostane levels can predict the presence, severity and extent of angiographic coronary artery disease. Acta Cardiol 2008; 63: 415–422.
Isoda K, Kamezawa Y, Ayaori M, Kusuhara M, Tada N, Ohsuzu F . Osteopontin transgenic mice fed with a high-cholesterol diet develop early fatty-streak lesions. Circulation 2003; 107: 679–681.
Sharman J, Lim R, Qasem A, Coombes J, Burgess M, Franco J, Garraphy P, Wilkinson I, Marwick T . Validation of a generalized transfer function to noninvasively derive central blood pressure during exercise. Hypertension 2006; 47: 1203–1208.
Wilkinson I, Fuchs S, Jansen I, Spratt J, Murray G, Cockcroft J, Webb D . The reproducibility of pulse wave velocity and augmentation index measured by pulse wave analysis. J Hypertens 1998; 16: 2079–2084.
Nakagawa N, Takahashi F, Chinda J, Kobayashi M, Hayashi Y, Abe M, Saijo Y, Kikuchi K, Hasebe N . A newly estimated glomerular filtration rate is independently associated with arterial stiffness in Japanese patients. Hypertens Res 2008; 31: 193–201.
Bazzichi L, Ghiadoni L, Rossi A, Bernardini M, Lanza M, De Feo F, Giacomelli C, Mencaroni I, Raimo K, Rossi M, Mazzone A, Taddei S, Bombardieri S . Osteopontin is associated with increased arterial stiffness in rheumatoid arthritis. Mol Med 2009; 15: 402–406.
Isoda K, Nishikawa K, Kamezawa Y, Yoshida M, Kusuhara M, Moroi M, Tada N, Ohsuzu F . Osteopontin plays an important role in the development of medial thickening and neointimal formation. Circ Res 2002; 91: 77–82.
Wada T, McKee M, Steitz S, Giachelli C . Calcification of vascular smooth muscle cell cultures: inhibition by osteopontin. Circ Res 1999; 84: 166–178.
Zagura M, Serg M, Kampus P, Zilmer M, Eha J, Unt E, Lieberg J, Cockcroft J, Kals J . Aortic stiffness and vitamin D are independent markers of aortic calcification in patients with peripheral arterial disease and in healthy subjects. Eur J Vasc Endovasc Surg 2011; 42: 689–695.
Zagura M, Serg M, Kampus P, Zilmer M, Zilmer K, Eha J, Unt E, Lieberg J, Kals J . Association of osteoprotegerin with aortic stiffness in patients with symptomatic peripheral artery disease and in healthy subjects. Am J Hypertens 2010; 23: 586–591.
de Kleijn D, Moll F, Hellings W, Ozsarlak-Sozer G, de Bruin P, Doevendans P, Vink A, Catanzariti L, Schoneveld A, Algra A, Daemen M, Biessen E, de Jager W, Zhang H, de Vries J, Falk E, Lim S, van der Spek P, Sze S, Pasterkamp G . Local atherosclerotic plaques are a source of prognostic biomarkers for adverse cardiovascular events. Arterioscler Thromb Vasc Biol 2010; 30: 612–619.
Patel R, Al Mheid I, Morris A, Ahmed Y, Kavtaradze N, Ali S, Dabhadkar K, Brigham K, Hooper W, Alexander R, Jones D, Quyyumi A . Oxidative stress is associated with impaired arterial elasticity. Atherosclerosis 2011; 218: 90–95.
Zieman S, Melenovsky V, Kass D . Mechanisms, pathophysiology, and therapy of arterial stiffness. Arterioscler Thromb Vasc Biol 2005; 25: 932–943.
Lind L . Arterial stiffness, but not endothelium-dependent vasodilatation, is related to a low ankle-brachial index. Clin Physiol Funct Imaging 2011; 31: 182–187.
Pannier B, Guerin A, Marchais S, Safar M, London G . Stiffness of capacitive and conduit arteries: prognostic significance for end-stage renal disease patients. Hypertension 2005; 45: 592–596.
Acknowledgements
We gratefully acknowledge E. Jaigma for the linguistic revision of the manuscript. This study was supported by grants of the Estonian Science Foundation (Nos. 9094 and 8273), by target financing (Nos. 0180105s08 and 0180001s07) by the European Union through the European Regional Development Fund (Centre of Excellence for Translational Medicine).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Zagura, M., Kals, J., Serg, M. et al. Structural and biochemical characteristics of arterial stiffness in patients with atherosclerosis and in healthy subjects. Hypertens Res 35, 1032–1037 (2012). https://doi.org/10.1038/hr.2012.88
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2012.88
Keywords
This article is cited by
-
Aortic stiffness is associated with the central retinal arteriolar equivalent and retinal vascular fractal dimension in a population along the southeastern coast of China
Hypertension Research (2015)
-
Metabolomic signature of arterial stiffness in male patients with peripheral arterial disease
Hypertension Research (2015)