Abstract
Isolated office hypertension (IOH) has been associated with structural cardiac abnormalities; however, its relation to worse cardiovascular prognosis remains uncertain. Less is known regarding the consequences of uncontrolled IOH in treated hypertensives. The aim was to investigate whether uncontrolled IOH was independently associated with two subclinical markers of cardiovascular disease, aortic stiffness and left ventricular hypertrophy (LVH). Clinical laboratory and 24-h ambulatory blood pressure (BP) data were obtained in 523 hypertensive patients with type 2 diabetes. Controlled office-ambulatory hypertension was defined by office blood pressure <140/90 mm Hg and 24-h BP <130/80 mm Hg, whereas uncontrolled IOH by office blood pressure⩾140/90 mm Hg and 24-h BP <130/80 mm Hg. Arterial stiffness was assessed by carotid-femoral pulse wave velocity (PWV) and left ventricular mass index (LVMI) by echocardiography. Statistics included multivariate linear and logistic regressions. According to BP patterns, 152 patients (29.1%) had controlled office-ambulatory hypertension, and 172 (32.9%) had uncontrolled IOH. Patients with uncontrolled IOH had greater LVMI (62.0±21.9 vs. 52.9±17.0 g m−2.7, P<0.001) and PWV (11.5±2.4 vs. 10.2±2.1 m s−1, P<0.001) than those with controlled hypertension. On linear model, after adjustment for several potential confounders, patients with uncontrolled IOH persisted with higher PWV (P=0.003) and LVMI (P=0.015). On logistic regression, the presence of uncontrolled IOH was independently associated with 2.7-fold (95% CI: 1.3–5.5) and 2.1-fold (95% CI: 1.1–4.0) higher risks of having increased aortic stiffness and LVH, respectively. In conclusion, uncontrolled IOH is associated with increased aortic stiffness and LVH in hypertensive type 2 diabetic patients. This may be a link to augmented cardiovascular risk.
Similar content being viewed by others
Introduction
Some studies showed a better cardiovascular prognosis for isolated office hypertension patients (white-coat hypertension) than for those with sustained hypertension;1, 2, 3 however, its prognostic significance in relation to sustained normal blood pressure (BP) remains controversial. 1, 4, 5, 6 Nonetheless, isolated office hypertension has been associated with structural cardiac abnormalities in general population studies, mainly increased left ventricular mass,7, 8, 9 which is a known marker of increased cardiovascular risk.10 In normoalbuminuric type 2 diabetic patients, the prevalence of isolated office hypertension appears to be identical to hypertensive nondiabetic individuals,11 and the presence of isolated office hypertension has been associated with macroalbuminuria and diabetic retinopathy.12 However, less knowledge is available regarding the importance of uncontrolled isolated office hypertension (the white-coat effect) in treated hypertensives in relation to those with sustained controlled office and ambulatory hypertension.
In recent years, there is a growing knowledge on the importance of arterial stiffness in the pathogenesis of cardiovascular diseases.13 Type 2 diabetic patients have increased arterial stiffness14, 15 and are at particularly augmented risk for cardiovascular morbidity and mortality. Arterial hypertension and ageing are the main determinants of arterial stiffness;13 and previous reports suggested that white-coat hypertensives may have higher arterial stiffness than normotensive individuals,16 and that the white-coat effect may be associated with increased arterial stiffness.17 Nevertheless, relationships between aortic stiffness and isolated office hypertension in diabetic patients have not been specifically investigated. We previously showed that aortic stiffness was independently related to microvascular complications in type 2 diabetic patients.18 The white-coat phenomenon, acute rises in BP levels that underlie uncontrolled isolated office hypertension in treated patients, was shown to increase retinal flow, suggesting that acute alterations in BP may have a deleterious effect on retinal vessels.19 Hence, we hypothesized that type 2 diabetic patients with uncontrolled isolated office hypertension may have increased aortic stiffness in comparison to those with controlled office and ambulatory BP levels. Therefore, we planned to investigate office and ambulatory BP patterns in a cohort of hypertensive type 2 diabetic patients, with particular attention to the relationships between uncontrolled isolated office hypertension (white-coat effect) and two markers of subclinical cardiovascular disease, increased aortic stiffness and left ventricular mass.
Methods
Study patients and baseline procedures
It was a cross-sectional study within a cohort of 567 patients with type 2 diabetes enrolled from August 2004 to December 2007 in the outpatient clinic of a tertiary-care university hospital. Exclusion criteria to enter the cohort were a body mass index ⩾40 kg m−2, serum creatinine ⩾2 mg per 100 ml or the presence of any serious concomitant disease limiting life expectancy. Diagnosis of diabetes followed the guidelines of the American Diabetes Association.20 All patients gave written informed consent and local ethics committee approved the study protocol. They were submitted to a standard protocol that included a complete clinical examination, laboratory evaluation, 24-h ambulatory BP monitoring (ABPM), 2D echocardiogram and carotid-femoral (aortic) pulse wave velocity (PWV) measurement. For this report, we excluded 48 normotensive subjects (8.5%), totaling 523 hypertensive patients with type 2 diabetes evaluated. Diagnostic criteria for macrovascular and microvascular degenerative complications were detailed previously.18, 21 In brief, coronary heart disease was diagnosed by clinical (history of angina or previous myocardial infarction), electrocardiographic (signs of ischemia or necrosis) or echocardiographic (segmental wall motion abnormalities) criteria, or by positive ischemic stress tests. Cerebrovascular disease was diagnosed by history and physical examination and peripheral arterial disease by systolic ankle-brachial index <0.9. The diagnosis of diabetic retinopathy was made by an ophthalmologic examination, performed by an experienced ophthalmologist. The diagnosis of nephropathy20 needed at least a urinary albumin excretion rate ⩾30 mg per 24 h or proteinuria ⩾0.5 g per 24 h in two nonconsecutive sterile 24-h urine collections or confirmed reduction of glomerular filtration rate (calculated by Cockcroft–Gault formula, <60 ml min−1 per 1.73 m2). Peripheral neuropathy was ascertained by history and clinical examination (knee and ankle reflex activities, feet sensation with the Semmes–Weinstein 5.07 monofilament and vibration, using a 128-Hz tuning fork). Neuropathy was defined as the presence of at least two of the following symptoms: reduced vibration perception, insensitivity to monofilament and absent tendon reflexes. Laboratory evaluation included fasting glycemia, glycated hemoglobin, serum creatinine and lipid profile. Dyslipidemia was defined by an abnormal lipid profile, following the guidelines of the National Cholesterol Education Program,22 or by being prescribed any hypolipemic drug. Urinary albumin excretion rate, proteinuria and creatinine were evaluated in two nonconsecutive sterile 24-h urine collections. Two-dimensional transthoracic echocardiography (Sonoline G60S; Siemens, Munich, Germany) was performed by the same experienced observer. Left ventricular mass was calculated by Devereux's formula23 and indexed to height2.7 (left ventricular mass index, LVMI). Left ventricular hypertrophy (LVH) was defined as LVMI >44 g m−2.7 in women and >48 g m−2.7 in men.24
Blood pressure measurements
Office BP was measured three times using a digital oscillometric BP monitor (HEM-907 XL; OMRON, Omron Healthcare, Kyoto, Japan) with a suitable sized cuff. The first measure was discarded and BP considered was the mean between the two last readings. Another set of office BP measurements was performed 2 weeks later. Arterial hypertension was diagnosed if mean (between the two visits) office systolic BP (SBP) ⩾140 mm Hg or diastolic BP (DBP) ⩾90 mm Hg or if antihypertensive drugs had been prescribed. ABPM was recorded using Mobil O Graph, version 12, equipment (Dinamap; Cardios, São Paulo, Brazil), approved by the British Society of Hypertension. Antihypertensive medications were optimized when necessary before performing ABPM, patients with uncontrolled office BPs had their antihypertensive drugs increased to maximal dosages, but no new antihypertensive drug was initiated before ABPM. All patients used their prescribed antihypertensive drugs during ABPM. A reading was taken every 15 min throughout the day and every 30 min at night. Nighttime period was ascertained for each individual patient from registered diaries. Parameters evaluated were 24-h, daytime and nighttime SBP and diastolic BP. Patients were classified into four groups based on office and ambulatory 24-h BPs: (1) controlled office-ambulatory hypertension (office BP <140/90 mm Hg and 24-h BP <130/80 mm Hg); (2) uncontrolled isolated office hypertension (office BP ⩾140/90 mm Hg and 24-h BP <130/80 mm Hg); (3) uncontrolled masked hypertension (office BP <140/90 mm Hg and 24-h BP ⩾130/80 mm Hg) and (4) uncontrolled office-ambulatory (sustained) hypertension (office BP ⩾140/90 mm Hg and 24-h BP ⩾130/80 mm Hg). An alternative analysis was performed with cutoff values for controlled office BP <130/80 mm Hg and 24-h ambulatory BP <125/75 mm Hg.
Arterial stiffness measurement
Immediately after the 24-h ABPM recording, a single trained independent observer unaware of other patients’ data, measured PWV along the descending thoracoabdominal aorta using the foot-to-foot velocity method with the Complior equipment (Artech Medical, Pantin, France), previously validated.25Methods used were detailed elsewhere.18 Briefly, waveforms were obtained transcutaneously over the right common carotid and the right femoral arteries simultaneously during a minimum period of 10–15 s. Three consecutive readings were obtained and PWV considered was the mean between them. Increased arterial stiffness was defined as aortic PWV >12 m s−1.26
Statistical analysis
Statistics was carried out by SPSS 13.0. statistical package (SPSS Inc., Chicago, IL, USA). Continuous variables were described as means (s.d.'s) when normally distributed or as medians (interquartile range) when asymmetrically distributed. Overall comparisons among the four subgroups of patients were performed by one-way analysis of variance (for continuous normal variables), Kruskal–Wallis test (for continuous asymmetrical variables) and χ2-test (for categorical variables). Post hoc comparisons with the reference subgroup with controlled office-ambulatory hypertension were performed with Bonferroni correction for multiple comparisons. Independent associations between continuous aortic PWV and LVMI with uncontrolled isolated office hypertension status were examined by a general linear model with adjustments for the following covariates: age, gender, body mass index, smoking status, dyslipidemia, macrovascular and microvascular diabetic complications, glycated hemoglobin, creatinine clearance, 24-h ambulatory SBP, number of drugs and specific classes of antihypertensive drugs in use. The multivariate analyses regarding aortic PWV were further adjusted for mean heart rate during PWV measurement. Associations between increased aortic stiffness and LVH with uncontrolled isolated office hypertension status were tested by multivariate logistic regression with adjustment for the same covariates. A two-tailed P-value <0.05 was regarded as significant.
Results
Baseline characteristics of patients grouped according to office and ambulatory BPs
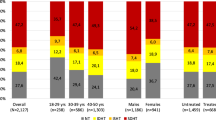
BP patterns according to office and 24-h BP levels were as follows: 152 patients (29. 1%) had controlled office-ambulatory hypertension, 172 (32.9%) uncontrolled isolated office hypertension, 42 (8.0%) uncontrolled masked hypertension and 157 (30.0%) uncontrolled office-ambulatory hypertension. Table 1 outlines the characteristics of the four subgroups. Patients with uncontrolled isolated office hypertension resembled those with controlled BP except that they were slightly older, less frequently current smokers, had a nonsignificant higher prevalence of diabetic retinopathy and used more antihypertensive drugs. Otherwise, patients with uncontrolled masked hypertension resembled those with uncontrolled office-ambulatory hypertension, except for a lower prevalence of diabetic nephropathy and for using fewer antihypertensive drugs. Table 2 shows office and ambulatory BP levels of the four subgroups of patients. Beyond presenting higher office BPs, patients with uncontrolled isolated office hypertension had also slightly higher ambulatory SBPs, both during daytime and nighttime periods. Mean difference in 24-h SBP between those with controlled office-ambulatory hypertension and uncontrolled isolated office hypertension subgroups was 2.0 mm Hg (95% CI: 0.2–3.8 mm Hg, P=0.029).
Independent associations between arterial stiffness and left ventricular mass with uncontrolled isolated office hypertension
Table 3 presents crude nonadjusted and adjusted associations between aortic stiffness and LVMI, analyzed both as continuous and as categorical variables, with uncontrolled isolated office hypertension in comparison to the reference subgroup with controlled office-ambulatory hypertension. Patients with uncontrolled isolated office hypertension had significantly higher aortic PWV, both nonadjusted and adjusted for several potential confounders, than those with controlled BP. On logistic regression, the presence of uncontrolled isolated office hypertension was independently associated with a 2.7-fold (95% CI: 1.3–5.5) higher risk of having increased aortic stiffness (PWV>12 m s−1) than patients with controlled office-ambulatory BPs, after the same multivariate adjustment. In the same manner, patients with uncontrolled isolated office hypertension had higher nonadjusted LVMI than those with controlled office-ambulatory hypertension and this difference persisted after proper statistical adjustment for potential confounders. Otherwise, uncontrolled isolated office hypertension status implied a significantly 2.1-fold (95% CI: 1.1–4.0) increased odds of having echocardiographic LVH after multivariate adjustment by logistic regression.
Changing the cutoff value for considering controlled BP to <130/80 mm Hg in office and to <120/75 mm Hg in ambulatory measurements decreased the number of individuals in the subgroups with controlled office-ambulatory hypertension (66 patients, 12.6%) and with uncontrolled isolated office hypertension (154 patients, 29.4%), whereas it increased the number of patients with uncontrolled office-ambulatory hypertension (270 patients, 51.6%). Even though, patients with uncontrolled isolated office hypertension persisted with higher aortic PWV and LVMI than patients with controlled office-ambulatory BP (Table 4). However, due to the smaller number of patients in each subgroup, a comprehensive multivariate adjustment could not be performed.
Discussion
This study evaluated the associations between two markers of preclinical cardiovascular disease, increased aortic stiffness and left ventricular mass, and the occurrence of uncontrolled isolated office hypertension in type 2 diabetic patients. It showed that subjects with uncontrolled isolated office hypertension had higher aortic stiffness and LVH prevalence than those with controlled office-ambulatory hypertension, after adjusting for several potential confounders including ambulatory BP levels, hypertension severity (reflected by the number of antihypertensive drugs and specific classes of drugs in use), metabolic parameters and presence of macrovascular and microvascular diabetic complications. Therefore, it suggests that uncontrolled isolated office hypertension may not be a benign condition, as increased aortic stiffness and LVH have been convincingly shown to predict a worse cardiovascular outcome in several clinical conditions,10, 27, 28, 29, 30 including type 2 diabetes.31 It also provides evidence in favor of treating white-coat hypertension in type 2 diabetic patients, a recent debated question.32, 33
Few previous studies evaluated the relationships between aortic stiffness and isolated office hypertension, generally with small number of individuals and none in diabetic patients. The first one16 suggested that patients with isolated office hypertension had higher aortic stiffness than those with sustained normal BP only if they had concomitantly other cardiovascular risk factors, such as diabetes or dyslipidemia. Another study34 also reported greater aortic PWV in isolated office hypertensives than in sustained normotensives. However, a third study35 did not find differences in aortic PWV between sustained normotensives and white-coat hypertensives. Our results cannot be compared to these previous reports because we enrolled only type 2 diabetic patients with treated hypertension. A recent study12 reported a greater prevalence of diabetic retinopathy and clinical nephropathy (macroalbuminuria) in type 2 diabetic patients with isolated office hypertension in comparison to sustained normotensives. Interestingly, we have recently reported18 that the presence of microvascular complications is associated with increased aortic stiffness. Furthermore, our subgroup with uncontrolled isolated office hypertension had a greater prevalence of diabetic retinopathy than those with controlled office-ambulatory BP. Otherwise, we showed that the significant association between increased aortic stiffness and uncontrolled isolated office hypertension was independent of the presence of microvascular and macrovascular chronic diabetic complications. Hence, increased large artery stiffness may be the pathophysiological mechanism underlying the reported12 association between isolated office hypertension and diabetic microvascular complications. Alternatively, both large artery and microcirculation may be damaged by the sudden BP rises that occur frequently in isolated office hypertension patients due to sympathetic overactivity. This has been shown to acutely increase retinal blood flow, which may be deleterious to retinal microcirculation.19
Contrary to aortic stiffness, the relationships between increased left ventricular mass and isolated office hypertension have been extensively evaluated, although also with controversial results.7, 8, 9, 36, 37, 38 The two largest studies, for example, reported opposite findings: one,7 with 1632 individuals from a population-based sample, found an increased LVMI in patients with isolated office hypertension, after adjustments for age, gender and 24-h BP, whereas the other,38 with 1535 consecutive patients referred for ABPM, reported no difference in LVMI between isolated office hypertensives and sustained normotensives. These discrepancies possibly originated from multiple reasons: different characteristics of patients evaluated (treated or untreated), different selection criteria (population-based or from a reference hypertension clinic), different selection of normotensive controls and also different cutoff values for defining ambulatory BP normality. In particular, the lack of established ABPM partition values for defining hypertension diagnosis and therapeutic targets in diabetic patients remains an important unresolved issue.39
Most importantly, the significance of either uncontrolled isolated office hypertension or isolated office hypertension to predict future cardiovascular morbidity and mortality remains unsettled. Studies focusing on target-organ damage suggested that patients with isolated office hypertension may be at an intermediate risk between sustained normotensives and those with sustained hypertension.7, 8, 9, 33 One meta-analysis and a study pooling data from four studies, all prospective cohorts, reported divergent results. The meta-analysis6 found a nonsignificant 12% higher risk of cardiovascular events in isolated office hypertensives (two of the seven studies included were performed in treated hypertensives), whereas the other study1 reported a trend toward an increased risk of stroke after the sixth year of follow-up in relation to sustained normotensives (in one of the four pooled studies antihypertensive medication was not withdrawn). Clearly, additional prospective studies with large number of individuals and long-term follow-up are needed to clarify this issue.
It should be emphasized that in this study, similar to others,7, 11 diabetic patients with uncontrolled isolated office hypertension had ambulatory BPs, although in the normal range, slightly higher than those with controlled office-ambulatory BP (in this study a mean difference of 2 mm Hg in 24-h SBP). This might explain, at least in part, the higher prevalence of subclinical cardiovascular disease in uncontrolled isolated office hypertension patients, because it is known that the relation between BP and cardiovascular disease is linear also in the normal BP range.7 Nonetheless, it does not entirely accounts for the increased cardiovascular risk profile associated with the white-coat effect, because the associations with increased aortic stiffness and LVH persisted after adjusting for 24-h BP levels. We may speculate that the increased LVM and aortic stiffness associated with uncontrolled isolated office hypertension may depend at least in part on neurohumoral, metabolic or other factors unrelated to BP levels. Among the mechanisms involved, an abnormal sympathetic response to environmental stimuli leading to acute rises in BP could lead to cardiovascular damage.11, 18
This study has some potential limitations. The cross-sectional design of this study precludes any causal inferences regarding the associations between aortic stiffness and LVH with the white-coat effect. All patients were under antihypertensive treatment or had uncontrolled office hypertension, so these results may not be generalized to normotensive diabetic patients. Furthermore, the associations of uncontrolled isolated office hypertension with both subclinical markers of cardiovascular disease remained significant even after adjusting for the number and each antihypertensive drug class in use; although a residual confounding effect of antihypertensive treatment cannot be ruled out. Also, the inclusion of subjects under antihypertensive treatment is common in most studies comparing the prognosis of different ABPM subgroups.6 Finally, this study was carried on in a tertiary-care hospital, with predominantly middle aged to elderly individuals and probably more severe patients, so our findings may not be generalized to younger diabetic patients and to patients followed-up at primary-care centers.
In conclusion, this study shows in a relatively large group of type 2 diabetic patients, independent associations between uncontrolled isolated office hypertension (white-coat effect) and increased aortic stiffness and LVH, two well-known markers of adverse cardiovascular outcomes. These relationships may be a pathophysiological link to augmented cardiovascular risk independent of other established determinants of cardiovascular damage; and uncontrolled isolated office hypertension shall not be considered a benign condition in type 2 diabetic patients.
References
Verdecchia P, Reboldi GP, Angeli F, Schillaci G, Schwartz JE, Pickering TG, Imai Y, Ohkubo T, Kario K . Short- and long-term incidence of stroke in white-coat hypertension. Hypertension 2005; 45: 203–208.
Pierdomenico SD, Lapenna D, Di Mascio R, Cuccurullo F . Short- and long-term risk of cardiovascular events in white-coat hypertension. J Hum Hypertens 2008; 22: 408–414.
Eguchi K, Hoshide S, Ishikawa J, Ishikawa S, Pickering TG, Gerin W, Ogedegbe G, Schwartz JE, Shimada K, Kario K . Cardiovascular prognosis of sustained and white-coat hypertension in patients with type 2 diabetes mellitus. Blood Press Monit 2008; 13: 15–20.
Gustavsen PH, Høegholm A, Bang LE, Kristensen KS . White coat hypertension is a cardiovascular risk factor: a 10-year follow-up study. J Hum Hypertens 2003; 17: 811–817.
Ohkubo T, Kikuya M, Metoki H, Asayama K, Obara T, Hashimoto J, Totsune K, Hoshi H, Satoh H, Imai Y . Prognosis of ‘masked’ hypertension and ‘white-coat’ hypertension detected by 24-h ambulatory blood pressure monitoring 10-year follow-up from the Ohasama study. J Am Coll Cardiol 2005; 46: 508–515.
Fagard RH, Cornelissen VA . Incidence of cardiovascular events in white-coat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens 2007; 25: 2193–2198.
Sega R, Trocino G, Lanzarotti A, Carugo S, Cesana G, Schiavina R, Valagussa F, Bombelli M, Giannattasio C, Zanchetti A, Mancia G . Alterations of cardiac structure in patients with isolated office, ambulatory, or home hypertension: data from the general population (Pressione Arteriose Monitorate E Loro Associazioni [PAMELA] study). Circulation 2001; 104: 1385–1392.
Palatini P, Mormino P, Santonastaso M, Mos L, Dal Follo M, Zanata G, Pessina AC . Target-organ damage in stage I hypertensive subjects with white-coat and sustained hypertension: results from the HARVEST study. Hypertension 1998; 31: 57–63.
Grandi AM, Broggi R, Colombo S, Santillo R, Imperiale D, Bertolini A, Guasti L, Venco A . Left ventricular changes in isolated office hypertension: a blood pressure-matched comparison with normotension and sustained hypertension. Arch Intern Med 2001; 161: 2677–2681.
Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP . Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. New Engl J Med 1990; 322: 1561–1566.
Nielsen FS, Gaede P, Vedel P, Pedersen O, Parving HH . White coat hypertension in NIDDM patients with and without incipient and overt diabetic nephropathy. Diabetes Care 1997; 20: 859–863.
Kramer CK, Leitão CB, Canani LH, Gross JL . Impact of white-coat hypertension on microvascular complications in type 2 diabetes. Diabetes Care 2008; 31: 2233–2237.
Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, Pannier B, Vlachopoulos C, Wilkinson I, Struijker-Boudier H . Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 2006; 27: 2588–2605.
Kimoto E, Shoji T, Shinohara K, Inaba M, Okuno Y, Miki T, Koyama H, Emoto M, Nishizawa Y . Preferential stiffening of central over peripheral arteries in type 2 diabetes. Diabetes 2003; 52: 448–452.
De Angelis L, Millasseau SC, Smith A, Viberti G, Jones RH, Ritter JM, Chowienczyk PJ . Sex differences in age-related stiffening of aorta in subjects with type 2 diabetes. Hypertension 2004; 44: 67–71.
Ribeiro L, Gama G, Santos A, Asmar R, Martins L, Polónia J . Arterial distensibility in subjects with white-coat hypertension with and without diabetes or dyslipidaemia: comparison with normotensives and sustained hypertensives. Blood Press Monit 2000; 5: 11–17.
de Simone G, Schillaci G, Chinali M, Angeli F, Reboldi GP, Verdecchia P . Estimate of white-coat effect and arterial stiffness. J Hypertens 2007; 25: 827–831.
Cardoso CR, Ferreira MT, Leite NC, Barros PN, Conte PH, Salles GF . Microvascular degenerative complications are associated with increased aortic stiffness in type 2 diabetic patients. Atherosclerosis 2009; 205: 472–476.
Rassam SM, Patel V, Kohner EM . The effect of experimental hypertension on retinal vascular autoregulation in humans: a mechanism for the progression of diabetic retinopathy. Exp Physiol 1995; 80: 53–68.
American Diabetes Association. Standards of medical care in diabetes—2007. Diabetes Care 2007; 30: S4–S41.
Cardoso CR, Leite NC, Freitas L, Dias SB, Muxfeld ES, Salles GF . Pattern of 24-hour ambulatory blood pressure monitoring in type 2 diabetic patients with cardiovascular dysautonomy. Hypertens Res 2008; 31: 865–872.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001; 285: 2486–2497.
Devereux RB, Reichek N . Echocardiographic determination of left ventricular mass in man. Anatomic validation of the method. Circulation 1977; 55: 613–618.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ, Chamber Quantification Writing Group; American Society of Echocardiography's Guidelines and Standards Committee; European Association of Echocardiography. Recommendations for chamber quantification: a report from the American Society of Echocardiography's guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of cardiology. J Am Soc Echocardiogr 2005; 18: 1440–1463.
Asmar R, Benetos A, Topouchian J, Laurent P, Pannier B, Brisac AM, Target R, Levy BI . Assessment of arterial distensibility by automatic pulse wave velocity: validation and clinical application studies. Hypertension 1995; 26: 485–490.
The task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Guidelines for the management of arterial hypertension. Eur Heart J 2007; 28: 1462–1536.
Laurent S, Boutouyrie P, Asmar R, Gautier I, Laloux B, Guize L, Ducimetiere P, Benetos A . Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension 2001; 37: 1236–1241.
Mattace-Raso FU, van der Cammen TJ, Hofman A, van Popele NM, Bos ML, Schalekamp MA, Asmar R, Reneman RS, Hoeks AP, Breteler MM, Witteman JC . Arterial stiffness and risk of coronary heart disease and stroke: the Rotterdam study. Circulation 2006; 113: 657–663.
Willum-Hansen T, Staessen JA, Torp-Pedersen C, Rasmussen S, Thijs L, Ibsen H, Jeppesen J . Prognostic value of aortic pulse wave velocity as index of arterial stiffness in the general population. Circulation 2006; 113: 664–670.
Sunström J, Lind L, Ärnlöv J, Zethelius B, Andrén B, Lithell HO . Echocardiographic and electrocardiographic diagnoses of left ventricular hypertrophy predict mortality independently of each other in a population of elderly men. Circulation 2001; 103: 2346–2351.
Cruickshank K, Riste L, Anderson SG, Wright JS, Dunn G, Gosling RG . Aortic pulse wave velocity and its relationship to mortality in diabetes and glucose intolerance: an integrated index of vascular function? Circulation 2002; 106: 2085–2090.
Mancia G, Sega R, Bombelli M, Quarti-Trevano F, Facchetti R, Grassi G . Should white-coat hypertension in diabetes be treated? Pro. Diabetes Care 2009; 32: S305–S309.
Bursztyn M, Ben-Dov IZ . White-coat hypertension should not treated in subjects with diabetes. Diabetes Care 2009; 32: S310–S313.
Longo D, Zaetta V, Perkovic D, Frezza P, Ragazzo F, Mos L, Santonastaso M, Garbelotto R, Benetos A, Palatini P . Impaired arterial elasticity in young patients with white-coat hypertension. Blood Press Monit 2006; 11: 243–249.
Silva JA, Barbosa L, Bertoquini S, Maldonado J, Polónia J . Relationship between aortic stiffness and cardiovascular risk factors in a population of normotensives, white-coat normotensives, white-coat hypertensives, sustained hypertensives and diabetic patients. Rev Port Cardiol 2004; 23: 1533–1547.
Pierdomenico SD, Lapenna D, Guglielmi MD, Antidormi T, Schiavone C, Cuccurullo F, Mezzetti A . Target organ status and serum lipids in patients with white coat hypertension. Hypertension 1995; 26: 801–807.
Owens PE, Lyons SP, Rodriguez SA, O’Brien ET . Is elevation of clinic blood pressure in patients with white coat hypertension who have normal ambulatory blood pressure associated with target organ damage? J Hum Hypertens 1998; 12: 743–748.
Kotsis V, Stabouli S, Toumanidis S, Papamichael C, Lekakis J, Germanidis G, Hatzitolios A, Rizos Z, Sion M, Zakopoulos N . Target organ damage in ‘white coat hypertension’ and ‘masked hypertension’. Am J Hypertens 2008; 21: 393–399.
Parati G, Bilo G . Should 24-h ambulatory blood pressure monitoring be done in every patient with diabetes? Diabetes Care 2009; 32: S298–S304.
Acknowledgements
G Salles and C Cardoso have research grants from Conselho Brasileiro de Desenvolvimento Científico e Tecnológico (CNPq) and from Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Salles, G., Teixeira, G., Leite, N. et al. Uncontrolled isolated office hypertension is associated with subclinical markers of cardiovascular disease in hypertensive type 2 diabetic patients. Hypertens Res 33, 819–824 (2010). https://doi.org/10.1038/hr.2010.80
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2010.80
Keywords
This article is cited by
-
Association of Arterial Stiffness Indexes, Determined From Digital Volume Pulse Measurement and Cardiovascular Risk Factors in Chronic Kidney Disease
American Journal of Hypertension (2011)