Abstract
Increased arterial stiffness may be causally related to resistant hypertension. Our objective was to investigate the variables, particularly those derived from ambulatory blood pressure (BP) monitoring (ABPM), associated with increased aortic stiffness in resistant hypertensives. In a cross-sectional study, 600 resistant hypertensive patients without peripheral arterial disease were evaluated. Arterial stiffness was assessed by aortic pulse wave velocity (PWV), and was considered increased if >12 m s−1. Statistical analyses included multiple linear and logistic regressions to assess the independent correlates of increased aortic stiffness. One hundred and sixty-eight patients (28%) had aortic PWV >12 m s−1. Patients with increased PWV were older and had a higher prevalence of cardiovascular risk factors than did those patients with low PWV. On ABPM, patients with elevated PWV had higher daytime and night time systolic BP (SBP) and pulse pressures (PP), less nocturnal decrease in SBP and a higher prevalence of non-dipping pattern. On multiple linear regression, the independently associated variables with aortic PWV were age (P<0.001), 24-h PP (P<0.001), high-density lipoprotein (HDL)-cholesterol (P<0.001), microalbuminuria (P<0.001), fasting glycemia (P=0.001) and a decrease in nocturnal SBP (P=0.002). Multivariate logistic regression confirmed these results, with the non-dipping patients having a 72% higher likelihood of presenting with increased aortic stiffness (95% confidence interval: 1.12–2.65, P=0.013). This association was observed in both the reduced and reverted dipping patterns, but not in the extreme dipping pattern. In conclusion, a blunted nocturnal decrease in BP is independently associated with increased aortic stiffness in resistant hypertensive patients. Other independent correlates are older age, diabetes, microalbuminuria, low HDL-cholesterol and a widened 24-h PP.
Similar content being viewed by others
Introduction
In recent years, there has been a growing awareness of the important role of both central arterial stiffness and abnormally large artery function in the pathogenesis of cardiovascular diseases.1, 2 Arterial stiffness depends on the material and geometric properties of the arterial wall, as well as on the artery's distending pressure. Aging and blood pressure (BP) are the main determinants of arterial stiffness.1, 2 The measurement of pulse wave velocity (PWV) between the common carotid and femoral arteries, that is, along the descending thoraco-abdominal aorta, is considered the gold standard evaluation of central arterial stiffness because it is a simple, non-invasive, robust and reproducible method.1 Most importantly, it has been shown to predict cardiovascular morbidity and mortality above and beyond other traditional cardiovascular risk factors in patients with end-stage renal disease,3 hypertension4, 5 and diabetes,6 as well as in elderly individuals7 and in the general population.8
Resistant hypertension (RH) is a common, but generally understudied, clinical condition.9 Defined as the failure to control office BP despite an optimal treatment with at least three antihypertensive drugs in full dosages, one of which is always a diuretic, its prevalence ranges from 10% to almost 30% of general hypertensives.9 It is a clinical condition in which the persistently elevated BP levels frequently lead to the rapid development of target organ damage and a high cardiovascular morbidity and mortality.10, 11 RH is also a well-established indication for ambulatory BP monitoring (ABPM)9, 12 to guide diagnosis, therapy and prognosis.10, 11, 12, 13, 14 Recent studies15 suggest that, on the basis of their common correlates, increased central arterial stiffness may be a cause of RH. Nevertheless, aortic stiffness has never been evaluated in patients with RH.
Therefore, the objective of this study was to investigate the independent correlates of increased aortic stiffness in a large group of RH patients. Specifically, we focused on well-known prognostic markers derived from ABPM, the nocturnal BP fall and circadian BP variability patterns16, 17 and their relationships to aortic stiffness.
Methods
Patients and baseline procedures
This was a cross-sectional study involving 600 patients with RH (mean (s.d.) age: 65 (11)years, 27.4% males) enrolled consecutively between March 2006 and April 2008 in the hypertension outpatient clinic of a tertiary-care university hospital. All participants gave written informed consent, and the study protocol was approved by the local Ethics Committee. The characteristics of this cohort, the baseline procedures and the diagnostic definitions have been detailed elsewhere.11, 12, 13, 18 In brief, all patients with essential hypertension (secondary hypertension was excluded, except sleep apnea syndromes that were not evaluated) who fulfilled criteria for RH (office BP ⩾140/90 mm Hg using at least three antihypertensive drugs in full dosages, always including a diuretic, and considered at least moderately adherent to treatment by a validated questionnaire19) but were without peripheral arterial disease (diagnosed by clinical examination or by an ankle-brachial index <0.9) were submitted to a standard protocol that included a thorough clinical examination, laboratory evaluation, 12-lead ECG, two-dimensional-echocardiography, 24-h ABPM and PWV measurement. BP was measured twice, with patients in the sitting position, using a digital blood pressure monitor (Omron HEM-907 XL, Omron Healthcare Co. Ltd., Kyoto, Japan) with a suitably sized cuff. The BP used in the study was the mean between the two readings. Pulse pressure (PP) was calculated as systolic BP minus diastolic BP (SBP−DBP). Physical activity was defined as the self-reporting of any activity in leisure hours for a minimum of 150 min per week. Coronary heart disease was diagnosed by one of the following: a history of angina, previous myocardial infarction or myocardial revascularization procedures; or by pathological Q-waves on ECG (Minnesota codes: 1.1, 1.2); or by echocardiographic segmental wall motion abnormalities. A history of stroke or transient ischemic attacks was diagnostic of cerebrovascular disease. Echocardiographic left ventricular mass was calculated by the Devereux formula and indexed to body surface area (LVMI). Left ventricular hypertrophy was defined as LVMI >125 g m−2 in men and >110 g m−2 in women. Laboratory evaluation included fasting glycemia, serum creatinine, electrolytes, lipid profile and urinary albumin excretion rate (UAER) in a sterile 24-h urine collection. Glomerular filtration rate was estimated by the Cockcroft-Gault equation.
Ambulatory blood pressure (BP) monitoring was performed with a Mobil O Graph version 12 (Dynamapa-Cardios Ltd., São Paulo, Brazil) recorder, which has been approved by the British Society of Hypertension.20 All patients used their prescribed antihypertensive medications during ABPM. A reading was taken every 15 min during the day. During the night time period, which was ascertained for each individual patient from registered diaries, readings were taken every 30 min. The parameters evaluated were mean 24 h, daytime and night time SBP, DBP and PP. Nocturnal SBP reduction was analyzed as a continuous variable (the night-to-day SBP ratio) and also dichotomized at well-established values. Patients were classified as non-dipping pattern (night-to-day SBP ratio >0.9) or as dipping (night-to-day SBP ratio ⩽0.9). We subclassified the patients by the nocturnal BP reduction as follows: normal dipping (night-to-day SBP ratio ⩽0.9 and >0.8), extreme dipping (night-to-day SBP ratio ⩽0.8), reduced dipping (night-to-day SBP ratio >0.9 and ⩽1.0) and reverted dipping pattern (night-to-day SBP ratio >1.0).
Immediately after the 24-h ABPM recording, a single trained independent observer, unaware of other patients' data, measured carotid-femoral PWV—using the foot-to-foot velocity method—with the Complior SP equipment and software21 (Artech-Medical, Paris, France). For this measurement, patients were in the supine position after a minimum 10 min rest at a comfortable room temperature. All examinations were carried out in the morning, between 0900 and 1100 hours, after patients had taken their morning dose of antihypertensive drugs. Briefly, waveforms were obtained transcutaneously over the right common carotid artery and the right femoral artery simultaneously during a minimum period of 10–15 s. The time delay (t) was measured between the troughs of the two waveforms, and the distance (D) covered by the waves was measured directly between the femoral recording site and the carotid recording site. Aortic PWV was calculated as D (meters)/t (seconds). Three consecutive readings were obtained, and the mean of these three readings was reported as the PWV. Increased central arterial stiffness was defined as an aortic PWV >12 m s−1.22
Statistical analysis
Continuous data were described as means±s.d. if normally distributed, or as medians (with interquartile range) if asymmetrically distributed. Bivariate comparisons between patients with and without increased aortic stiffness were performed by unpaired t-test (for continuous normal variables), Mann–Whitney test (for continuous asymmetric variables) and by χ2-test (for categorical variables). Simple Pearson's coefficients of correlation were used to evaluate the associations between aortic PWV and both office and ambulatory BPs. We also used the z-test for comparison of r values for these associations. Independent correlates of increased central arterial stiffness were assessed both by means of multiple linear regression (with continuous aortic PWV as the dependent variable) and multiple logistic regression (with aortic PWV >12 m s−1 as the dependent variable). For both multivariate analyses, a stepwise forward selection procedure was used, in which a P-value <0.10 was the criterion to remain in the models. The candidate variables were the following: age, gender, waist circumference, presence of diabetes, physical inactivity, dyslipidemia, smoking status, coronary heart disease and cerebrovascular disease at baseline, ambulatory 24-h PP and the nocturnal SBP fall, heart rate, fasting glycemia, serum total and high-density lipoprotein (HDL)-cholesterol, triglycerides, UAER and estimated glomerular filtration rate. UAER and estimated glomerular filtration rate were log10 transformed because of their high positive-skewed distribution. For logistic regression, age was dichotomized at 65 years, 24-h PP at 57 mm Hg (the median value), with the nocturnal SBP fall as dipping/non-dipping pattern, HDL-cholesterol at values suggested by the Third Report of the National Cholesterol Education Program Expert Panel, and UAER as normal (<30 mg/24 h) and abnormal microalbuminuria (⩾30 mg/24 h). Finally, for comparisons of aortic PWV among subgroups of different dipping patterns, analysis of covariance was used with post hoc Bonferroni's correction for pairwise comparisons with the reference normal dipping subgroup, adjusted for other covariates (age, 24-h mean arterial pressure, glycemia, HDL-cholesterol and log10 UAER). All statistical analyses were performed with the SPSS statistical package version 13.0 (SPSS Inc., Chicago, IL, USA) and a two-tailed P-value <0.05 was regarded as significant.
Results
Baseline characteristics
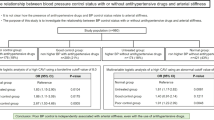
Aortic PWV averaged 10.9 m s−1 (s.d.: 2.3, median value: 10.7, range: 5.2–23.4 m s−1) with normal distribution. One hundred and sixty-eight patients (28%) presented with increased aortic PWV (>12 m s−1). Table 1 outlines the baseline characteristics of patients with normal and increased aortic PWV. Patients with increased PWV were older, with a wider waist circumference, an increased prevalence of cardiovascular risk factors (diabetes, physical inactivity, dyslipidemia and microalbuminuria) and more coronary heart disease at baseline compared with patients with lower aortic PWV. They also had higher office and ambulatory SBP and PP, lower nocturnal BP decline and a higher prevalence of non-dipping patterns than those without increased PWV. There were no differences in the antihypertensive drug treatment between the two groups in either the number or the specific classes of antihypertensive drugs used. There was also no difference in antihypertensive treatment between the dipper and non-dipper patients. All patients used a median of four antihypertensive drugs at baseline (range 3–6 drugs, 100% were on diuretics) and a median of two drugs at bedtime (all patients took at least one antihypertensive drug at bedtime).
Independent correlates of increased aortic stiffness
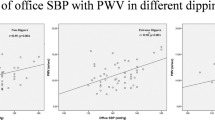
Table 2 shows the simple linear correlations of SBP and PP, both office and ambulatory, with aortic PWV. Correlation coefficients were significantly higher for ambulatory BPs and PP than for office BPs and SBP (respectively). In addition, night time BPs tended to be more closely correlated with aortic PWV than daytime BPs. On account of this, we chose to include 24-h PP (which included the daytime and the night time periods) in the multivariate analyses.
Table 3 shows the independent correlates of aortic PWV, evaluated as a continuous variable, by means of multiple linear regressions. Age, 24-h PP, HDL-cholesterol, UAER, fasting glycemia and the nocturnal SBP decline—all analyzed as continuous variables—were the independent correlates of central arterial stiffness. The inclusion of 24-h SBP in the regression model, instead of PP, did not affect the results. Twenty-four hours SBP replaced 24-h PP as the second most strongly associated variable with aortic PWV (partial correlation: 0.25, P<0.001), but did not change any of the other significant covariates. For example, the nocturnal SBP reduction remained significantly associated with aortic PWV, and the parameters were virtually unchanged. The B-coefficient changed from 0.26 to 0.27, and the partial correlation coefficient remained unchanged at 0.13.
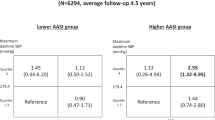
Table 4 presents the independent variables associated with increased aortic stiffness (PWV >12 m s−1) when evaluated by multivariate logistic regression. Similar to the previous analysis, older age, a widened 24-h PP, presence of diabetes, a low HDL-cholesterol, abnormal microalbuminuria and non-dipping pattern were the independent correlates. Changing the cutoff value for increased aortic PWV to >10 m s−1, or using age-dependent cutoffs (>10 m s−1 in individuals younger than 65 years and >12 m s−1 in those older than 65 years), did not alter qualitatively the results of logistic regression.
Finally, Figure 1 shows that an association between the non-dipping pattern and increased aortic stiffness is observed in both the reduced and the reverted dipping patterns, whereas the extreme dipping subgroup had an aortic PWV equal to the normal-dipping patients.
Box-plot graphic representation of aortic pulse wave velocity in the four subgroups of dipping patterns. P-values are for analysis of covariance (ANCOVA) post hoc comparisons (after Bonferroni's correction) using a normal dipping group as the reference, and after further adjustment for age, 24-h mean arterial pressure, fasting glycemia, high-density lipoprotein-cholesterol and log10 urinary albumin excretion rate.
Discussion
This study shows that a blunted nocturnal BP reduction, evaluated either as a continuous variable or as categorical dipping/non-dipping status, is an independent correlate of increased central aortic stiffness in patients with RH. This association is observed in both the reduced and the reverted dipping patterns, but not in the extreme dipping pattern. This study also found that, beyond aging and BP levels (ambulatory PP was the best correlated BP variable), well-known determinants of increased arterial stiffness, a high fasting glycemia (or diabetes), a low HDL-cholesterol and an increased UAER are also independently associated with aortic stiffness. This is the first study investigating the correlates of central arterial stiffness in patients with RH, an important and prevalent subgroup of general hypertensive patients9 with a very high cardiovascular-risk profile.10, 11
Few studies have examined the relationships between the nocturnal BP decline, dipping patterns and central arterial stiffness. When studied, the findings have been conflicting. The first study to address this issue,23 which evaluated 106 untreated hypertensive individuals, found that aortic PWV was an independent predictor of the nocturnal SBP reduction. Similarly, three other studies24, 25, 26 reported significant associations between the non-dipping pattern and arterial stiffness. The largest study,25 evaluating 314 untreated hypertensives, reported a significant association only with the reverted dipping pattern. Two other studies27, 28 did not find any correlation between the dipping pattern and arterial stiffness, probably because they only evaluated the nocturnal BP decline as dipping/non-dipping categories, which has poor reproducibility.29 Recently, two other cross-sectional studies,30, 31 the largest31 using 622 treated and untreated hypertensives, also found no associations between the continuous nocturnal BP reduction and aortic PWV using multivariate analysis. The conflicting results could either be due to the different hypertensive populations evaluated (number of patients, treated or untreated, resistant or non-resistant, influence of different antihypertensive medications) or the different methods of evaluation (number of BP measurements during the night time period; fixed or variable nocturnal period, definitions of abnormal dipping patterns; and different measures of arterial stiffness) or both.
The pathogenesis underlying this association between a blunted nocturnal BP reduction and increased aortic stiffness has not been elucidated. Although a causal relationship cannot be inferred from a cross-sectional design study, we can generate some hypotheses. A low nocturnal BP decrease is associated with higher night time SBP and PP, which may be particularly deleterious to aortic structure and function. Conversely, both conditions may be linked by common pathogenetic mechanisms, such as nocturnal autonomic imbalance favoring sympathetic overactivity,25, 32 or low-grade chronic systemic inflammation.33, 34 More importantly, a blunted nocturnal BP decrease has been consistently shown to be a predictor of worse cardiovascular outcome.16, 17 Our results suggest that an increased central arterial stiffness may be one of the underlying physiopathological mechanisms involved in this worse cardiovascular prognosis. These important issues should be addressed in future prospective studies that use serial determinations of aortic PWV to determine whether a blunted nocturnal BP reduction is actually associated with increasing aortic stiffness during follow-up. Furthermore, studies must investigate whether any therapeutic intervention to reverse non-dipping patterns would be able to improve aortic stiffness, thus reducing cardiovascular morbidity and mortality.
The other independent correlates of increased arterial stiffness observed in this study—aging, BP levels, fasting glycemia, HDL-cholesterol and microalbuminuria—have all been described earlier.35, 36 The impact of fasting glycemia and HDL-cholesterol levels probably reflect the influence of metabolic syndrome on central arterial stiffness.37 In particular, the independent association between increased aortic stiffness and microalbuminuria, a marker of glomerular (and probably systemic) endothelial dysfunction/damage, links microvascular damage with large artery dysfunction and deserves further discussion. This association has been reported earlier both in diabetic38 and non-diabetic hypertensive patients.39 Increased aortic stiffness may damage microcirculation by the transmission of increased pulsatile pressure to microvascular beds.2 Such transduction would be especially deleterious in high-flow low-resistance vascular beds present in the kidneys and the brain.40 Alternatively, microvascular dysfunction may damage large elastic arteries by an inward remodeling, in which altered vasodilatation of the microcirculation enhances pulse wave reflections and central PP.2 Finally, both microcirculation and large artery damage may have common pathogenetic mechanisms yet to be discovered.2
This study has some limitations. First, being a cross-sectional study, causal inferences regarding the observed associations are precluded. Second, sleep apnea syndromes, a secondary cause of hypertension associated with a blunted nocturnal BP fall, were not routinely investigated. Hence, the presence of sleep apnea may be a confounder of the relationship between nocturnal BP reduction and aortic stiffness, which we could not account for. We routinely investigated the presence of renovascular hypertension and primary hyperaldosteronism, and excluded these patients from this report. Third, this study enrolled only patients with RH, which is a common but generally understudied subgroup of general hypertensives.9 Therefore, our results may not be generalized to other hypertensive individuals.
In conclusion, this study involving a large group of RH patients shows that a blunted nocturnal BP decline and non-dipping patterns are independently correlated with increased aortic stiffness. Other independent correlates are older age, a widened ambulatory PP, high fasting glycemia, low HDL-cholesterol levels and increased microalbuminuria. This suggests that RH patients with increased aortic stiffness may be at a particularly high cardiovascular risk, as all the correlates are well-known markers of adverse cardiovascular outcome. Prospective studies are necessary to investigate both the cardiovascular prognostic value and the physiopathological mechanisms underlying the relationships between circadian BP variability and arterial stiffness.
Conflict of interest
The authors declare no conflict of interest.
References
Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, Pannier B, Vlachopoulos C, Wilkinson I, Struijker-Boudier H . Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 2006; 27: 2588–2605.
Laurent S, Boutouyrie P . Recent advances in arterial stiffness and wave reflection in human hypertension. Hypertension 2007; 49: 1202–1206.
Blacher J, Guerin AP, Pannier B, Marchais SJ, Safar ME, London GM . Impact of aortic stiffness on survival in end-stage renal disease. Circulation 1999; 99: 2434–2439.
Laurent S, Boutouyrie P, Asmar R, Gautier I, Laloux B, Guize L, Ducimetiere P, Benetos A . Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension 2001; 37: 1236–1241.
Boutouyrie P, Tropeano AI, Asmar R, Gautier I, Benetos A, Lacolley P, Laurent S . Aortic stiffness is an independent predictor of primary coronary events in hypertensive patients: a longitudinal study. Hypertension 2002; 39: 10–15.
Cruickshank K, Riste L, Anderson SG, Wright JS, Dunn G, Gosling RG . Aortic pulse wave velocity and its relationship to mortality in diabetes and glucose intolerance: an integrated index of vascular function? Circulation 2002; 106: 2085–2090.
Mattace-Raso FU, van der Cammen TJ, Hofman A, van Popele NM, Bos ML, Schalekamp MA, Asmar R, Reneman RS, Hoeks AP, Breteler MM, Witteman JC . Arterial stiffness and risk of coronary heart disease and stroke: the Rotterdam study. Circulation 2006; 113: 657–663.
Willum-Hansen T, Staessen JA, Torp-Pedersen C, Rasmussen S, Thijs L, Ibsen H, Jeppesen J . Prognostic value of aortic pulse wave velocity as index of arterial stiffness in the general population. Circulation 2006; 113: 664–670.
Calhoun DA, Jones D, Textor S, Goff DC, Murphy TP, Toto RD, White A, Cushman WC, White W, Sica D, Ferdinand K, Giles TD, Falkner B, Carey RM . Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension 2008; 51: 1403–1419.
Redon J, Campos C, Narciso ML, Rodicio JL, Pascual JM, Ruilope LM . Prognostic value of ambulatory blood pressure monitoring in refractory hypertension: a prospective study. Hypertension 1998; 31: 712–718.
Salles G, Cardoso C, Muxfeldt E . Prognostic influence of office and ambulatory blood pressures in resistant hypertension. Arch Intern Med 2008; 168: 2340–2346.
Muxfeldt ES, Bloch KV, Nogueira AR, Salles GF . Twenty-four hour ambulatory blood pressure monitoring pattern of resistant hypertension. Blood Press Monit 2003; 8: 181–185.
Muxfeldt ES, Bloch KV, Nogueira Ada R, Salles GF . True resistant hypertension: is it possible to be recognized in the office? Am J Hypertens 2005; 18: 1534–1540.
Hermida RC, Ayala DE, Calvo C, López JE, Mojón A, Fontao MJ, Soler R, Fernández JR . Effects of time of day of treatment on ambulatory blood pressure pattern of patients with resistant hypertension. Hypertension 2005; 46: 1053–1059.
Pickering TG . Arterial stiffness as a cause of resistant hypertension? J Clin Hypertens 2007; 9: 390–395.
Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M, Matsubara M, Hashimoto J, Hoshi H, Araki T, Tsuji I, Satoh H, Hisamichi S, Imai Y . Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J Hypertens 2002; 20: 2183–2189.
Boggia J, Li Y, Thijs L, Hansen TW, Kikuya M, Björklund-Bodegård K, Richart T, Ohkubo T, Kuznetsova T, Torp-Pedersen C, Lind L, Ibsen H, Imai Y, Wang J, Sandoya E, O'Brien E, Staessen JA, International Database on Ambulatory blood pressure monitoring in relation to Cardiovascular Outcomes (IDACO) investigators. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet 2007; 370: 1219–1229.
Muxfeldt ES, Fiszman R, Castelpoggi CH, Salles GF . Ambulatory arterial stiffness index or pulse pressure: which correlates better with arterial stiffness in resistant hypertension? Hypertens Res 2008; 31: 607–613.
Morisky DE, Green LW, Levine DM . Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care 1986; 24: 67–74.
Jones CR, Taylor K, Chowienczyk P, Poston L, Shennan AH . A validation of the Mobil O Graph (version 12) ambulatory blood pressure monitor. Blood Press Monit 2000; 5: 233–238.
Asmar R, Benetos A, Topouchian J, Laurent P, Pannier B, Brisac AM, Target R, Levy BI . Assessment of arterial distensibility by automatic pulse wave velocity: validation and clinical application studies. Hypertension 1995; 26: 485–490.
Guidelines for the management of arterial hypertension. The task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2007; 28: 1462–1536.
Asmar R, Scuteri A, Topouchian J, Brisac AM, Maldonado J, Cloarec L, Safar M . Arterial distensibility and circadian blood pressure variability. Blood Press Monit 1996; 1: 333–338.
Lekakis JP, Zakopoulos NA, Protogerou AD, Papaioannou TG, Kotsis VT, Pitiriga VC, Tsitsirikos MD, Stamatelopoulos KS, Papamichael CM, Mavrikakis ME . Arterial stiffness assessed by pulse wave analysis in essential hypertension: relation to 24-h blood pressure profile. Int J Cardiol 2005; 102: 391–395.
Jerrard-Dunne P, Mahmud A, Feely J . Circadian blood pressure variation: relationship between dipper status and measures of arterial stiffness. J Hypertens 2007; 25: 1233–1239.
Shinohata R, Nakatsu T, Yuki Y, Nishitani A, Mashima K, Toyonaga S, Ogawa H, Hirohata S, Usui S, Kitawaki T, Kusachi S . Association of augmentation index of radial pressure wave form with diurnal variation pattern of blood pressure in untreated patients with essential hypertension. J Hypertens 2008; 26: 535–543.
Grandi AM, Broggi R, Jessula A, Laurita E, Cassinerio E, Piperno F, Bertolini A, Guasti L, Venco A . Relation of extent of nocturnal blood pressure decrease to cardiovascular remodeling in never-treated patients with essential hypertension. Am J Cardiol 2002; 89: 1193–1196.
Tsioufis C, Tzioumis K, Dimitriadis K, Chatzis D, Skiadas I, Michailidis A, Toutouzas P, Kallikazaros I, Stefanadis C . Nondipping status does not attenuate the conjugated estrogen-induced improvement in aortic stiffness in postmenopausal women with untreated hypertension. Am J Hypertens 2005; 18: 607–611.
Cuspidi C, Michev I, Meani S, Severgnini B, Fusi V, Corti C, Salerno M, Valerio C, Magrini F, Zanchetti A . Reduced nocturnal fall in blood pressure, assessed by two ambulatory blood pressure monitorings and cardiac alterations in early phases of untreated essential hypertension. J Hum Hypertens 2003; 17: 245–251.
Schillaci G, Parati G, Pirro M, Pucci G, Mannarino MR, Sperandini L, Mannarino E . Ambulatory arterial stiffness index is not a specific marker of reduced arterial compliance. Hypertension 2007; 49: 986–991.
Jerrard-Dunne P, Mahmud A, Feely J . Ambulatory arterial stiffness index, pulse wave velocity and augmentation index—interchangeable or mutually exclusive measures? J Hypertens 2008; 26: 529–534.
Sayk F, Becker C, Teckentrup C, Fehm H-L, Struck J, Wellhoener JP, Dodt C . To dip or not to dip. On the physiology of blood pressure decrease during nocturnal sleep in healthy humans. Hypertension 2007; 49: 1070–1076.
Von Känel R, Jain S, Mills PJ, Nelesen RA, Adler KA, Hong S, Perez CJ, Dimsdale JE . Relation of nocturnal blood pressure dipping to cellular adhesion, inflammation and hemostasis. J Hypertens 2004; 22: 2087–2093.
Mahmud A, Feely J . Arterial stiffness is related to systemic inflammation in essential hypertension. Hypertension 2005; 46: 1118–1122.
Yamashina A, Tomiyama H, Arai T, Hirose K, Koji Y, Hirayama Y, Yamamoto Y, Hori S . Brachial-ankle pulse wave velocity as a marker of atherosclerotic vascular damage and cardiovascular risk. Hypertens Res 2003; 26: 615–622.
Mitchell GF, Guo CY, Benjamin EJ, Larson MG, Keyes MJ, Vita JA, Vasan RS, Levy D . Cross-sectional correlates of increased aortic stiffness in the community. The Framingham heart study. Circulation 2007; 115: 2628–2636.
Schillaci G, Pirro M, Vaudo G, Mannarino MR, Savarese G, Pucci G, Franklin SS, Mannarino E . Metabolic syndrome is associated with aortic stiffness in untreated essential hypertension. Hypertension 2005; 45: 1078–1082.
Smith A, Karalliedde J, De Angelis L, Goldsmith D, Viberti G . Aortic pulse wave velocity and albuminuria in patients with type 2 diabetes. J Am Soc Nephrol 2005; 16: 1069–1075.
Kohara K, Tabara Y, Tachibana S, Nakura J, Miki T . Microalbuminuria and arterial stiffness in a general population: the Shimanami Health Promoting Program (J-SHIPP) study. Hypertens Res 2004; 27: 471–477.
O'Rourke MF, Safar ME . Relationship between aortic stiffening and microvascular disease in brain and kidney. Cause and logic of therapy. Hypertension 2005; 46: 200–204.
Acknowledgements
G Salles and C Cardoso have research grants from the Brazilian National Research Council (CNPq) and from the Research Support Foundation of Rio de Janeiro State (FAPERJ). FINEP-PETROBRAS also provided financial support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Castelpoggi, C., Pereira, V., Fiszman, R. et al. A blunted decrease in nocturnal blood pressure is independently associated with increased aortic stiffness in patients with resistant hypertension. Hypertens Res 32, 591–596 (2009). https://doi.org/10.1038/hr.2009.71
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2009.71
Keywords
This article is cited by
-
Nocturnal systolic blood pressure dipping and progression of chronic kidney disease
Hypertension Research (2024)
-
Is there any true distinction in extreme dipping versus nondipping or dipping phenotype regarding hypertension-mediated organ damage in newly diagnosed and never-treated hypertensive patients?
Journal of Human Hypertension (2022)
-
Nocturnal blood pressure dipping is similar in rheumatoid arthritis patients as compared to a normal population
Zeitschrift für Rheumatologie (2019)
-
Hemoglobin A1c and C-reactive protein are independently associated with blunted nocturnal blood pressure dipping in obesity-related prediabetes
Hypertension Research (2018)
-
Arterial (Aortic) Stiffness in Patients with Resistant Hypertension: from Assessment to Treatment
Current Hypertension Reports (2017)