Abstract
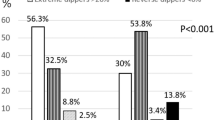
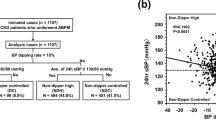
Dipping phenomena is defined as nocturnal BP fall >10% during 24-h ambulatory blood pressure (BP) monitoring (ABPM) which carries a favorable cardiovascular risk (CVR) prognosis due to reduced 24-h hypertension burden. To date, extreme dipping phenotype (defined as BP decrease ≥20%) has led to controversial prognostic results regarding CVR. We aimed to explore hypertension-mediated organ damage (HMOD) in extreme dippers compared to the other dipping phenotypes (nondipping, dipping). From 490 consecutive patients with newly diagnosed never-treated arterial hypertension (mean age 51 ± 11 years, 294 males) subjected to 24-h ABPM, we studied 52 extreme dippers, 52 age- and gender-matched nondippers, and 52 age- and gender-matched dippers. All patients were subjected to arterial stiffness (PWV), 24-h microalbumin levels, carotid intima-media thickness (cIMT), diastolic dysfunction (E/Ea), and left ventricular mass index (LVMI) evaluation. ANOVA analysis found no differences regarding HMOD between groups. Multiple regression analysis revealed the following independent direct relationships between: (i) office SBP and PWV in nondippers (β = 0.35, p = 0.01) and extreme dippers (β = 0.49, p < 0.001), (ii) office SBP and E/Ea in extreme dippers (β = 0.39, p = 0.007), (iii) 24-h diurnal and nocturnal SBP and E/Ea in dippers (β = 0.40, p = 0.004, β = 0.39, p = 0.005, and β = 0.40, p = 0.004, respectively), and (iv) 24-h and nocturnal SBP and LVMI in nondippers (β = 0.29, p = 0.04 and β = 0.36, p = 0.009, respectively). In the early phases of untreated-arterial hypertension disease, extreme dipping phenotype in middle-aged hypertensives does not imply an adverse or favorable prognosis regarding the incidence of HMOD either as continuous variables or as abnormal HMOD compared to other dipping phenotypes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension and the European Society of Cardiology: ESH/ESC task force for the management of arterial hypertension. J Hypertens 2018;36:2284–309.
O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, et al. European society of hypertension working group on blood pressure monitoring. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–68.
Mancia G, Verdecchia P. Clinical value of ambulatory blood pressure: evidence and limits. Circ Res. 2015;116:1034–45.
Pickering TG. The clinical significance of diurnal blood pressure variations. Dippers nondippers Circulation. 1990;81:700–2.
Verdecchia P. Prognostic value of ambulatory blood pressure: current evidence and clinical implications. Hypertension. 2000;35:844–51.
O’Flynn AM, Dolan E, Curtin RJ, O’Brien E, Perry IJ, Kearney PM. Night-time blood pressure and target organ damage: a comparative analysis of absolute blood pressure and dipping status. J Hypertens. 2015;33:2257–64.
Kotruchin P, Hoshide S, Kario K. Carotid atherosclerosis and the association between nocturnal blood pressure dipping and cardiovascular events. J Clin Hypertens. 2018;20:450–5.
Cuspidi C, Tadic M, Sala C, Gherbesi E, Grassi G, Mancia G. Extreme dipping: is the cardiovascular risk increased? An unsolved issue. J Hypertension. 2019;37:1917–26.
Metoki H, Ohkubo T, Kikuya M, Asayama K, Obara T, Hashimoto J, et al. Prognostic significance for stroke of a morning pressure surge and a nocturnal blood pressure decline the Ohasama Study. Hypertension. 2006;47:149–54.
Pierdomenico SD, Pierdomenico AM, Coccina F, Lapenna D, Porreca E. Circadian blood pressure changes and cardiovascular risk in elderly-treated hypertensive patients. Hypertens Res. 2016;39:805–11.
Kario K, Matsuo T, Kobayashi H, Imiya M, Matsuo M, Shimada K. Relation between nocturnal fall of blood pressure and silent cerebrovascular damage in elderly hypertensives: advanced silent cerebrovascular damage in extreme-dippers. Hypertension. 1996;27:130–5.
Kario K, Pickering TG, Matsuo T, Hoshide S, Schwartz JE, Shimada K. Stroke prognosis and abnormal nocturnal blood pressure falls in older hypertensives. Hypertension. 2001;38:852–7.
Rodrigues JCL, Amadu AM, Dastidar AG, Harries I, Burchell AE, Ratcliffe LEK, et al. Nocturnal dipping status and left ventricular hypertrophy: a cardiac magnetic resonance imaging study. J Clin Hypertens (Greenwich). 2018;20:784–93.
Jerrarrd-Dunne P, Mahmud A, Feely J. Circadian blood pressure variation: relationship between dipper status and measures of arterial stiffness. J Hypertens. 2007;25:1233–9.
Amah G, Ouardani R, Pasteur-Rousseau A, Voicu S, Safar ME, Kubis N, et al. Extreme-dipper profile, increased aortic stiffness and impaired subendocardial viability in hypertension. Am J Hypertens. 2017;30:417–26.
Lekakis JP, Zakopoulos NA, Protogerou AD, Papaioannou TG, Kotsis VT, Pitiriga VC, et al. Arterial stiffness assessed by pulse wave analysis in essential hypertension: relation to 24-h blood pressure profile. Int J Cardiol. 2005;102:391–5.
Cuspidi C, Facchetti R, Quarti-Trevano F, Dell’Oro R, Tadic M, Gherbesi E, et al. Clinical correlates and subclinical cardiac organ damage in different extreme dipping patterns. J Hypertens. 2020;38:858–63.
Georgianos PI, Agarwal R. Can We Mend the Broken Clock by Timing Antihypertensive Therapy Sensibly? Clin J Am Soc Nephrol. 2020;15:1513–5.
Lekakis JP, Ikonomidis I, Protogerou AD, Papaioannou TG, Stamatelopoulos K, Papamichael CM, et al. Arterial wave reflection is associated with severity of extracoronary atherosclerosis in patients with coronary artery disease. Eur J Cardiovasc Prev Rehabil. 2006;13:236–42.
Devereux R, Reichek N. Echocardiographic assessment of left ventricular mass in man. Circulation. 1977;55:613–8.
Ikonomidis I, Lekakis J, Papadopoulos C, Triantafyllidi H, Paraskevaidis I, Georgoula G, et al. Incremental value of pulse wave velocity in the determination of coronary microcirculatory dysfunction in never-treated patients with essential hypertension. Am J Hypertens. 2008;21:806–13.
Van Bortel LM, Laurent S, Boutouyrie P, Chowienczyk P, Cruickshank JK, De Backer T, et al. Artery Society; European Society of Hypertension Working Group on Vascular Structure and Function; European Network for Noninvasive Investigation of Large Arteries. Expert consensus document on the measurement of aortic stiffness in daily practice using carotid-femoral pulse wave velocity. J Hypertension. 2012;30:445–8.
Cuspidi C, Caffi G, Dell’Oro R, Tadic M, Sala C, Grassi G, et al. Extreme dipping: Always means nocturnal hypotension? Am J Hypertens. 2019;32:842–7.
Salles GF, Reboldi G, Fagard RH, Cardoso CRL, Pierdomenico SD, Verdecchia P. Prognostic Effect of the Nocturnal Blood Pressure Fall in Hypertensive Patients: The Ambulatory Blood Pressure Collaboration in Patients With. Hypertension (ABC-H) Meta-Anal Hypertension. 2016;67:693–700.
Palatini P, Verdecchia P, Beilin LJ, Eguchi K, Imai Y, Kario K, et al. Association of Extreme Nocturnal Dipping With Cardiovascular Events Strongly Depends on Age. Hypertension. 2020;75:324–30.
Benomo Y, Spears M, Boustred C, May M, Anderson SG, Benjamin EJ, et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. JACC. 2014;63:636–46.
Asmar R, Scuteri A, Topouchian J, Brisac AM, Maldonado J, Cloarec L, et al. Arterial distensibility and circadian blood pressure variability. Blood Press Monit. 1996;4:333–8.
Castelpoggi CH, Pereira VS, Fiszman R, Cardoso C, Muxfeldt ES, Salles G. A blunted decrease in nocturnal blood pressure is independently associated with increased aortic stiffness in patients with resistant hypertension. Hypertens Res. 2009;32:591–6.
Tadic M, Cuspidi C, Celic V, Pencic B, Mancia G, Grassi G, et al. The prognostic effect of circadian blood pressure pattern on long-term cardiovascular outcome is independent of left ventricular remodeling. J Clin Med. 2019;12:2126.
Verdecchia P, Schillaci G, Gatteschi C, Benemio G, Boldrini F, Porcellati C. Circadian blood pressure changes and left ventricular hypertrophy in essential hypertension. Circ. 1990;81:528–36.
Marinakis AG, Vyssoulis GP, Michaelides AP, Karpanou EA, Cokkinos DV, Toutouzas PK. Impact of abnormal nocturnal blood pressure fall on vascular function. Am J Hypertens. 2003;16:209–13.
Ivanovic BA, Tadic MV, Celic VP. To dip or not to dip? The unique relationship between different blood pressure patterns and cardiac function and structure. J Hum Hypertens. 2013;27:62–70.
Vasunta RL, Kesäniemi YA, Ylitalo A, Ukkola O. Non-dipping pattern and carotid atherosclerosis in a middle-aged population: OPERA Study. Am J Hypertens. 2012;25:60–6.
Myers MG, Kaczorowski J, Dolovich L, Tu K, Paterson JM. Cardiovascular risk in hypertension in relation to achieved blood pressure using automated office blood pressure measurement. Hypertension. 2016;68:866–72.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41371_2021_491_MOESM2_ESM.doc
Correlation between systolic blood pressure (24h ABPM and office) and hypertension mediated organ damage in several dipping phenotypes
Rights and permissions
About this article
Cite this article
Triantafyllidi, H., Birmpa, D., Schoinas, A. et al. Is there any true distinction in extreme dipping versus nondipping or dipping phenotype regarding hypertension-mediated organ damage in newly diagnosed and never-treated hypertensive patients?. J Hum Hypertens 36, 51–60 (2022). https://doi.org/10.1038/s41371-021-00491-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-021-00491-x
This article is cited by
-
Extreme dipping and target organ damage: is there any relationship?
Journal of Human Hypertension (2021)