Abstract
Shandong Province is located in the east of China. The province is characterized by robust economic development, with a rural population accounting for 56% of the total population. However, no data are available regarding temporal changes in the prevalence, awareness, treatment and control of hypertension among this population. Three independent cross-sectional surveys were performed in 1991 (n=8359), 2002 (n=18922) and 2007 (n=20167) in the rural area population, aged 35–74 years. The sampling included a survey on blood pressure and associated risk factors. Although the rate of smoking and alcohol consumption decreased significantly from 1991 to 2007, the prevalence of overweight and obesity increased, whereas that of high-strength physical activity decreased remarkably. In 1991, 2002 and 2007, the prevalence of prehypertension was 33.8, 61.5 and 54.6%, respectively. The prevalence of hypertension was 20.4, 24.5 and 30.6%, respectively. Overall, the rate of hypertension awareness, treatment and control showed a steady increase over the 16-year period, although the control rate of hypertension is still far from being satisfactory. In conclusion, among the Chinese rural population, the prevalence of prehypertension and hypertension increased significantly from 1991 to 2007. Public health programs are required to improve this situation in Chinese rural populations.
Similar content being viewed by others
Introduction
Cardiovascular diseases are the major cause of death in most developed and some developing countries.1, 2 Hypertension is one of the most important risk factors of cardiovascular diseases, and many studies have consistently demonstrated the long-term benefits of effective control of hypertension. Although recent data showed an upward trend in the rates of hypertension awareness, treatment and control and a downward trend in the prevalence of cardiovascular diseases in most developed countries,3, 4, 5 cardiovascular diseases in developing countries are still rampant, largely because hypertension is poorly controlled.6, 7, 8
Recently some investigators have reported the prevalence and the rates of hypertension awareness, treatment and control in several Chinese populations.7, 9, 10, 11 However, owing to the large variation in geographical characteristics, dietary patterns, local lifestyles, income, education levels and health care in different regions of China, the prevalence and the rates of hypertension awareness, treatment and control in different studies may differ widely.12 Shandong Province is located in the east of China with the rural population accounting for 56% of the total population. During the past two decades, most young and middle-aged farmers in the rural areas of Shandong Province were employed by companies in neighboring cities and their daily physical activity dropped significantly. Although Shandong Province has been ranked as one of the best provinces in China with regard to economic development, public health resources are more limited in the rural area than in the urban area. No data are available regarding the temporal changes in hypertension prevalence, awareness, treatment and control rates in the rural areas of rapidly developing provinces in China. Nonetheless, these data are extremely important for evaluating the impact of economic development on health care and vice versa.
Another important issue is the prevalence and significance of prehypertension. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC-7) defined normal blood pressure as systolic blood pressure (SBP) <120 mm Hg and diastolic blood pressure (DBP) <80 mm Hg and prehypertension as SBP of 120–139 mm Hg or DBP of 80–89 mm Hg.13 In the Chinese population, prehypertension has been found to be associated with increased risk of hypertension and major cardiovascular diseases.14, 15 However, the temporal changes in prehypertension prevalence in the Chinese population are still unknown.
In an attempt to answer these questions, this study was designed to examine the evolution of the prevalence of prehypertension and hypertension as well as the rates of hypertension awareness, treatment and control over the past two decades in a Chinese rural population. To this end, we used three cross-sectional surveys performed in the same rural area of Zhangqiu County, Shandong Province, China.
Methods
Three major cross-sectional surveys of hypertension were conducted in Zhangqiu County, Shandong Province, China, according to a random, multistaged cluster sampling scheme. The sample population included 8359 (4067 men), 18 922 (8926 men) and 20 167 (7770 men) subjects (aged 35–74 years) in 1991, 2002 and 2007, respectively. Data were collected during a single clinic visit by cardiologists and specially trained nurses using standardized methods. The information collected included demographic characteristics such as age, sex, body weight, height and education, history of hypertension, cigarette smoking, alcohol consumption and administration of antihypertensive medications. The response rates for the subjects participating in the surveys of 1991, 2002 and 2007 were 93.1, 92.6 and 95.4%, respectively. Current smokers were defined as smoking at least one cigarette per day during the last year.2 Smokers were further divided into heavy smokers (⩾20 cigarettes per day) and light smokers (<20 cigarettes per day).16 Alcohol drinkers were defined as drinking alcohol at least 12 times during the previous year.17 This population was further divided into heavy drinkers (⩾30 g ethanol per day) and light drinkers (<30 g ethanol per day).18 Body weight was measured with 0.1-kg precision when the subjects were wearing light indoor clothing without shoes. Height was measured to the nearest 0.5 cm. Body mass index (BMI) was calculated as weight (kg)/height (m)2. Overweight and obesity in both men and women were defined as 25⩽BMI<30 and BMI⩾30 kg m−2, respectively, according to the World Health Organization (WHO) criteria.19 Work-related physical activity was classified as one of three categories in accordance with previously described methods:20 low strength, sitting office work; moderate strength, work including standing and walking; and high strength, work including walking and lifting, or heavy manual labor. Education levels were divided into low (years of education ⩽9) and high (years of education >9) levels.
Blood pressure in the right arm was measured between 0800 and 1200 hours using standard mercury sphygmomanometers after the subjects had been sitting quietly for 5 min. SBP and DBP were each taken as the mean of three readings. Normotension and prehypertension were defined using the JNC-7 criteria.13 Hypertension was defined as SBP⩾140 mm Hg and/or DBP⩾90 mm Hg and/or use of antihypertensive medications. Awareness of hypertension was defined as reporting a previous diagnosis of hypertension by a health-care professional. Treatment of hypertension was defined as reported use of an antihypertensive drug during the previous 2 weeks. Control of hypertension was defined as receiving drug treatment for hypertension, as well as recorded SBP <140 mm Hg and DBP <90 mm Hg.7 Participants were divided into four groups according to their ages (35–44, 45–54, 55–64 and 65–74 years).
Statistical analysis
Continuous data were reported as mean±s.d. Categorical variables were presented as frequencies and s.e. (%, s.e.). Statistical analysis involved use of SPSS for Windows (v15.0; SPSS, Chicago, IL, USA). Differences in mean values of the baseline characteristics among groups, including height, weight, SBP and DBP, were tested by one-way analysis of variance. Differences in prevalence of overweight, obesity, smoking, alcohol consumption, high-level education, high-strength physical activity, prehypertension and hypertension among groups were tested by χ2-test. BMI, blood pressure, prevalence of prehypertension, hypertension, smoking, alcohol consumption, overweight, obesity, different levels of education and physical activity as well as awareness, treatment and control rates of hypertension from the three surveys were adjusted by age and sex with data obtained during the census in China.7 In brief, the adjusted prevalence (%) was calculated as: P=∑(Pi × Ji), where Pi is the prevalence of a given epidemiological parameter in each age and sex group in this study, and Ji is the percentage of each age and sex group in the Chinese census population. The association between risk factors and hypertension was tested by logistic regression analysis, using age, BMI (categorized as BMI<25, 25⩽BMI<30 and BMI⩾30 kg m−2), sex, education, physical activity, and smoking and drinking status as independent variables. In order to clarify the impact of gender on weight-associated blood pressure, the data were stratified by gender. A P-value <0.05 was considered to be statistically significant.
Results
Temporal changes in the prevalence of prehypertension
In each survey, the prevalence of prehypertension tended to decline with increased age in both men and women (Table 1). However, prehypertension was more common in men than in women for all three surveys (36.5 vs. 31.2% in 1991; 63.4 vs. 56.3% in 2002 and 56.4 vs. 53.7% in 2007, all P<0.05, Figure 1). In both men and women, the prevalence of prehypertension increased remarkably from 1991 to 2002 and remained high from 2002 to 2007 (Figure 1). After adjustment by age and sex, the prevalence of prehypertension showed an immense surge from 33.8% in 1991 to 61.5% in 2002 and to 54.6% in 2007 (both P<0.01, Figure 1).
Age-adjusted prevalence of normotension (NT), prehypertension (PHT) and hypertension (HT) in different years and genders. (a) Prevalence of NT, prehypertension (PHT) and HT in men; (b) Prevalence of NT, PHT and HT in women; (c) Prevalence of NT, PHT and HT in all subjects. *P<0.05, **P<0.01: vs. 1991; #P<0.05, ##P<0.01: vs. 1991; □P<0.05, □□P<0.01: vs. 2002.
Temporal changes in the prevalence of hypertension
In contrast to the case of prehypertension, the prevalence of hypertension rose with increased age in both men and women in all three surveys. For most age groups, the prevalence of hypertension increased significantly from 1991 to 2007 (from 11.4% in 1991 to 15.7% in 2007 in the 35–44 year age group, from 19.9% in 1991 to 33.9% in 2007 in the 45–54 year age group and from 30.0% in 1991 to 45.9% in 2007 in the 55–64 year age group, all P<0.05), but not in the 65–74 year age group (from 45.5% in 1991 to 47.2% in 2007, P>0.05) (Table 1). The prevalence of hypertension was similar in men and women in 1991 (19.8 vs. 21.0%, P>0.05), but was higher in men than in women in 2002 (25.7 vs. 21.2%, P<0.05) and in 2007 (32.0 vs. 28.8%, P<0.05, Figure 1). However, after adjustment by age and sex, the prevalence of hypertension still exhibited a stepwise increase from 20.4% in 1991 to 24.5% in 2002 (P<0.05) and to 30.6% in 2007 (P<0.01, Figure 1).
Trends in demographic characteristics
The majority of the population in the 1991 and 2002 surveys were farmers who engaged in high-strength physical labor. In the 2007 survey, most young and middle-aged people were employed by companies in neighboring cities and towns. The demographic characteristics determined by the three surveys are shown in Table 2. The rate of cigarette smoking in these populations dropped significantly from 42.5% in 1991 to 16.3% in 2007 (P<0.01), and the rate of alcohol consumption declined significantly from 25.2% in 1991 to 18.0% in 2007 (P<0.05). The rate of high-strength physical activity decreased significantly from 75.5% in 1991 to 49.5% in 2007. In contrast, the rates of overweight, obesity and high-level education as well as body weight and SBP levels increased steadily from 1991 to 2002 and from 1991 to 2007. Thus, the prevalence of overweight and obesity increased from 19.7 and 3.5% in 1991 to 49.7 and 9.3% in 2007, respectively (all P<0.05). SBP increased from 123.1 mm Hg in 1991 to 127.9 mm Hg in 2007 (P<0.01), and DBP increased from 74.7 mm Hg in 1991 to 81.0 mm Hg in 2002 (P<0.05), but no significant difference in DBP was found between 2002 and 2007.
Association between demographic characteristics and the risk of hypertension
To study the association between demographic characteristics and the risk of hypertension, multivariate logistic regression analysis was performed on the basis of the data obtained in 2007. In comparison with the 35–44 year group, the 45–54, 55–64 and 65–74 year groups showed a stepwise increase in the risk of hypertension (Table 3). Similarly, male sex, overweight, obesity, low-strength physical activity, high alcohol consumption and heavy smoking were independently associated with hypertension. The odds ratios of these parameters were all more than 1.0 for increased risk of hypertension, which was statistically significant. However, there was no significant association between low alcohol consumption or education levels and hypertension. It is interesting to note that high-strength physical activity had an odds ratio less than 1.0, suggesting this is a protective factor against hypertension (Table 3).
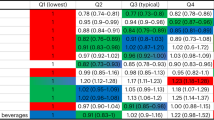
Temporal changes in the rates of hypertension awareness, treatment and control
As shown in Table 4, the rate of hypertension awareness tended to rise with increased age in both men and women, but was consistently higher in women than in men in all three surveys (16.6 vs. 13.2% in 1991, 51.1 vs. 46.4% in 2002 and 53.5 vs. 50.6% in 2007, all P<0.05, Figure 2). After adjustment by age and sex, the rate of awareness of hypertension exhibited a stepwise increase from 15.0% in 1991 to 49.0% in 2002 and to 52.4% in 2007 (both P<0.01, Figure 2).
Age-adjusted rates of hypertension awareness, treatment and control in different years and genders. (a) Rates of hypertension awareness, treatment and control in men; (b) Rates of hypertension awareness, treatment and control in women; (c) Rates of hypertension awareness, treatment and control in all subjects. *P<0.05, **P<0.01: vs. 1991; #P<0.05, ##P<0.01: vs. 1991; □P<0.05, □□P<0.01: vs. 2002.
Similar to the rate of hypertension awareness, the rate of hypertension treatment tended to increase with increased age in both men and women, but was consistently higher in women than in men in all three surveys (10.1 vs. 7.7% in 1991, 42.4 vs. 34.8% in 2002 and 39.6 vs. 36.2% in 2007, all P<0.05, Figure 2). After adjustment by age and sex, the rate of treatment for hypertension increased from 8.9% in 1991 to 38.8% in 2002 and 38.3% in 2007 (both P<0.01, Figure 2).
In contrast to the rates of hypertension awareness and treatment, the rate of hypertension control did not show any trend in changes with age, but was higher in women than in men in all three surveys (3.8 vs. 2.9% in 1991, 6.6 vs. 6.0% in 2002 and 7.6 vs. 6.7% in 2007, all P<0.05, Figure 2). After adjustment by age and sex, the rate of hypertension control increased from 3.3% in 1991 to 6.3% in 2002 and 7.3% in 2007 (both P<0.01, Figure 2).
Discussion
The major findings of this study are that in a Chinese rural area, (1) the prevalence of prehypertension increased remarkably from 1991 to 2007; (2) the prevalence of hypertension increased steadily over the 16-year period; (3) the remarkable increase in overweight and obesity and decrease in physical activity may partially explain the upward trend of prehypertension and hypertension; and (4) rates of hypertension awareness, treatment and control showed a steady increase over the 16-year period, although the rate of control of hypertension is still far from satisfactory. To the best of our knowledge, our study is the first to report temporal changes in the prevalence of prehypertension and hypertension and the rates of hypertension awareness, treatment and control in a Chinese rural area over the past two decades.
One notable finding in this study was that the prevalence of prehypertension almost doubled from 33.8% in 1991 to 61.5% in 2002. The prevalence of prehypertension in 1991 in our subjects was similar to that (34.5%) determined by a study of the Chinese population in 1991.14 However, the prevalence of prehypertension in 2002 in our study was higher than that (from 23.9 to 44.3%) in other studies conducted in China, Israel, the United States and Japan.21, 22, 23, 24 Although variations in geography, race, age and lifestyle in different studies may partially account for the differences in observed results,12, 24 the rapid increase in the prevalence of prehypertension from 1991 to 2002 in our study may be related to the more stressful workload, high-calorie and salty food, reduced physical activity and more common overweight and obesity in the rural area during the past two decades.25, 26 Although the term prehypertension is still in dispute, recent studies have found a positive correlation between prehypertension and major cardiovascular diseases in the Chinese population,14, 15 indicating that detection of prehypertension may have important clinical significance.
In this study, the prevalence of hypertension showed a steady increase from 1991 to 2007. Data from the Third Nationwide Survey of Blood Pressure Level and Hypertension27 in 1991 (age ⩾15 years) and the China National Nutrition and Health Survey7 in 2002 (age ⩾18 years) showed the prevalence to be 11.26 and 18%, respectively. However, the prevalence of hypertension showed a gradual decrease from the north to the south. Thus, the prevalence of hypertension (30.6%) reported in this study was higher than that in the southern area (from 16.0 to 23.3%),11, 12 but similar to that in the northeastern area (from 33.8 to 36.2%)10, 12 of China. In contrast, studies conducted in Europe showed reduced blood pressure over the past two decades,3, 5 whereas studies from the United States found a decreasing trend in the prevalence of hypertension before 1990, with a rise in recent years.4, 28 Thus, the trend of the prevalence of hypertension during the past two decades in the Chinese population studies is different from that in Europe or the United States.
Our results confirmed that cigarette smoking was an associated risk factor for hypertension,29 although the prevalence of smoking dropped significantly over the 16 years, in contrast to the rapid increase in the prevalence of hypertension during the same period of time. It is noteworthy that smoking of any amount is an important risk factor of hypertension and thus, completely abstaining from smoking is important to reduce the risk of hypertension. However, the association between alcohol consumption and hypertension was significant only in heavy drinkers, which was consistent with previously reported results.18 The prevalence of overweight and obesity in our study increased by 252 and 266%, respectively, from 1991 to 2007, which is similar to a previous report from China.30 Our results confirmed that overweight and obesity were independent risk factors for hypertension,31 which may explain, at least in part, why the prevalence of hypertension went up despite a decreased prevalence of smoking and alcohol consumption during the past two decades. The association between obesity and blood pressure was reportedly more prominent in women,32 but our results showed that the impact of obesity on hypertension appeared to be more significant in men than in women. Differences in body fat distribution among different races may partially account for the different impacts of gender and obesity on blood pressure.
It should be noted that the education level in the Chinese rural area under investigation was significantly improved in accordance with economic development, although a low level of education was not proven to be an independent risk factor for hypertension, contrary to the results of a study conducted in a northeast rural area in China.10 One recent survey revealed that people with less physical activity had higher blood pressure,33 and our study confirmed this finding. As most people in the Chinese rural area do not engage in regular physical activity during their leisure time, only work-related physical activity was assessed in this study. Our results showed that the rate of high-strength physical activity dropped 34.4% over the 16-year period, representing an emerging risk factor for hypertension in China.
An encouraging finding of this study was that the rate of hypertension awareness increased tremendously from 15.0% in 1991 to 49.0% in 2002 and 52.4% in 2007, the latter being significantly higher than that in a Chinese national survey (24%)7 and an Iranian study (34%),6 but relatively lower than that in a US study (63.0–68.5%)4, 28 and a Czech study (67.2%).3 These differences may reflect discrepancies in public health education and medical resources.
In accordance with temporal changes in the rate of hypertension awareness, the rate of hypertension treatment showed a substantial increase from 8.9 to 38.3% over the 16-year period. Although the latest rate of hypertension treatment obtained in this study was higher than that in the Chinese national survey in 2002 (18.7%)7 and that in a northeast rural area in China (19.8%),10 it is still lower than those reported for the United States and Europe (43.0–61.4%).3, 4, 28 It is noteworthy that the hypertension treatment rate did not improve from 2002 to 2007, meaning that more than 60% patients with hypertension did not receive any treatment.
As revealed in this study, the rate of hypertension control doubled from 1991 (3.3%) to 2002 (6.3%) and from 1991 to 2007 (7.2%). Although our study was performed in a rural area, the rate of hypertension control was still higher than that (4.56%) reported by the Chinese national survey in 20027 and that determined by a northeast rural area in China (0.90%).10 However, it is still much lower than that reported for the United States and other developed countries and regions (from 8.7 to 35.1%).3, 4, 28, 34, 35 As it is the control rate of hypertension that determines the clinical outcome of hypertensive patients, the presence of a large number of patients with uncontrolled hypertension represents a big burden to society. Further improvement in public health education and reform to the medical insurance system will be necessary to effectively control hypertension in the rural areas of China.
There were two major limitations in our study. First, our study population included only rural populations in Shandong Province and further studies should recruit both rural and urban populations to accurately capture the evolution of hypertension in China. Second, we did not collect data on serum lipid levels or other relevant laboratory results. Therefore, contribution of these factors to the prevalence of hypertension could not be analyzed.
In conclusion, in the rural area of Shandong Province, China, the prevalence of prehypertension and hypertension was still on the rise from 1991 to 2007. Remarkable increase of overweight and obesity may partially explain the situation. Although the rates of hypertension awareness, treatment and control more than doubled from 1991 to 2007, hypertension is still poorly controlled and has constituted a major socioeconomic problem in China. Enhanced public health programs are required to improve this situation among the rural population in China.
Conflict of interest
The authors declare no conflict of interest.
References
Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ . Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 2006; 367: 1747–1757.
He J, Gu D, Wu X, Reynolds K, Duan X, Yao C, Wang J, Chen CS, Chen J, Wildman RP, Klag MJ, Whelton PK . Major causes of death among men and women in China. N Engl J Med 2005; 353: 1124–1134.
Cifkova R, Skodova Z, Lanska V, Adamkova V, Novozamska E, Petrzilkova Z, Jozifova M, Plaskova M, Hejl Z, Palous D, Galovcova M . Trends in blood pressure levels, prevalence, awareness, treatment, and control of hypertension in the Czech population from 1985 to 2000/01. J Hypertens 2004; 22: 1479–1485.
Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ . Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988-1994 and 1999-2004. Hypertension 2008; 52: 818–827.
Kastarinen M, Antikainen R, Peltonen M, Laatikainen T, Barengo NC, Jula A, Salomaa V, Jousilahti P, Nissinen A, Vartiainen E, Tuomilehto J . Prevalence, awareness and treatment of hypertension in Finland during 1982–2007. J Hypertens 2009; 27: 1552–1559.
Esteghamati A, Abbasi M, Alikhani S, Gouya MM, Delavari A, Shishehbor MH, Forouzanfar M, Hodjatzadeh A, Ramezani RD . Prevalence, awareness, treatment, and risk factors associated with hypertension in the Iranian population: the national survey of risk factors for noncommunicable diseases of Iran. Am J Hypertens 2008; 21: 620–626.
Wu Y, Huxley R, Li L, Anna V, Xie G, Yao C, Woodward M, Li X, Chalmers J, Gao R, Kong L, Yang X . Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation 2008; 118: 2679–2686.
Yadav S, Boddula R, Genitta G, Bhatia V, Bansal B, Kongara S, Julka S, Kumar A, Singh HK, Ramesh V, Bhatia E . Prevalence & risk factors of pre-hypertension & hypertension in an affluent north Indian population. Indian J Med Res 2008; 128: 712–720.
Wang Z, Wu Y, Zhao L, Li Y, Yang J, Zhou B . Trends in prevalence, awareness, treatment and control of hypertension in the middle-aged population of China, 1992–1998. Hypertens Res 2004; 27: 703–709.
Dong G, Sun Z, Zheng L, Li J, Zhang X, Zhang X, Xu C, Li J, Hu D, Sun Y . Prevalence, awareness, treatment, and control of hypertension in rural adults from Liaoning Province, northeast China. Hypertens Res 2007; 30: 951–958.
Ruixing Y, Limei Y, Yuming C, Dezhai Y, Weixiong L, Muyan L, Fengping H, Jinzhen W, Guangqing Y, Zhenbiao N . Prevalence, awareness, treatment, control and risk factors of hypertension in the Guangxi Hei Yi Zhuang and Han populations. Hypertens Res 2006; 29: 423–432.
Reynolds K, Gu D, Muntner P, Wu X, Chen J, Huang G, Duan X, Whelton PK, He J . Geographic variations in the prevalence, awareness, treatment and control of hypertension in China. J Hypertens 2003; 21: 1273–1281.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL, Jones DW, Materson BJ, Oparil S, Wright Jr JT, Roccella EJ . The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289: 2560–2572.
Gu D, Chen J, Wu X, Duan X, Jones DW, Huang JF, Chen CS, Chen JC, Kelly TN, Whelton PK, He J . Prehypertension and risk of cardiovascular disease in Chinese adults. J Hypertens 2009; 27: 721–729.
Yu D, Huang J, Hu D, Chen J, Cao J, Li J, Gu D . Association between prehypertension and clustering of cardiovascular disease risk factors among Chinese adults. J Cardiovasc Pharmacol 2009; 53: 388–400.
Sharabi Y, Grotto I, Huerta M, Eldad A, Green MS . Risk factor profile for atherosclerosis among young adults in Israel—results of a large-scale survey from the young adult periodic examinations in Israel (YAPEIS) database. Eur J Epidemiol 2001; 17: 757–764.
Reilly KH, Gu D, Duan X, Wu X, Chen CS, Huang J, Kelly TN, Chen J, Liu X, Yu L, Bazzano LA, He J . Risk factors for chronic obstructive pulmonary disease mortality in Chinese adults. Am J Epidemiol 2008; 167: 998–1004.
Fuchs FD, Chambless LE, Whelton PK, Nieto FJ, Heiss G . Alcohol consumption and the incidence of hypertension: the Atherosclerosis Risk in Communities Study. Hypertension 2001; 37: 1242–1250.
World Health Organization. Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser 1995; 854: 1–452.
Hu G, Tuomilehto J, Silventoinen K, Barengo N, Jousilahti P . Joint effects of physical activity, body mass index, waist circumference and waist-to-hip ratio with the risk of cardiovascular disease among middle-aged Finnish men and women. Eur Heart J 2004; 25: 2212–2219.
Kawamoto R, Kohara K, Tabara Y, Miki T . High prevalence of prehypertension is associated with the increased body mass index in community-dwelling Japanese. Tohoku J Exp Med 2008; 216: 353–361.
Sun Z, Zheng L, Xu C, Li J, Zhang X, Liu S, Li J, Hu D, Sun Y . Prevalence of prehypertension, hypertension and, associated risk factors in Mongolian and Han Chinese populations in Northeast China. Int J Cardiol 2008; 128: 250–254.
Wang Y, Wang QJ . The prevalence of prehypertension and hypertension among US adults according to the new joint national committee guidelines: new challenges of the old problem. Arch Intern Med 2004; 164: 2126–2134.
Grotto I, Grossman E, Huerta M, Sharabi Y . Prevalence of prehypertension and associated cardiovascular risk profiles among young Israeli adults. Hypertension 2006; 48: 254–259.
Wang Z, Zhai F, Du S, Popkin B . Dynamic shifts in Chinese eating behaviors. Asia Pac J Clin Nutr 2008; 17: 123–130.
Xu F, Yin XM, Tong SL . Association between excess bodyweight and intake of red meat and vegetables among urban and rural adult Chinese in Nanjing, China. Asia Pac J Public Health 2007; 19: 3–9.
Wu X, Duan X, Gu D, Hao J, Tao S, Fan D . Prevalence of hypertension and its trends in Chinese populations. Int J Cardiol 1995; 52: 39–44.
Ong KL, Cheung BM, Man YB, Lau CP, Lam KS . Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension 2007; 49: 69–75.
Halperin RO, Gaziano JM, Sesso HD . Smoking and the risk of incident hypertension in middle-aged and older men. Am J Hypertens 2008; 21: 148–152.
Wang Y, Mi J, Shan XY, Wang QJ, Ge KY . Is China facing an obesity epidemic and the consequences? The trends in obesity and chronic disease in China. Int J Obes (Lond) 2007; 31: 177–188.
Patterson RE, Frank LL, Kristal AR, White E . A comprehensive examination of health conditions associated with obesity in older adults. Am J Prev Med 2004; 27: 385–390.
Sharabi Y, Grotto I, Huerta M, Grossman E . Susceptibility of the influence of weight on blood pressure in men versus women: lessons from a large-scale study of young adults. Am J Hypertens 2004; 17: 404–408.
Grotto I, Huerta M, Grossman E, Sharabi Y . Relative impact of socioeconomic status on blood pressure lessons from a large-scale survey of young adults. Am J Hypertens 2007; 20: 1140–1145.
Hajjar I, Kotchen TA . Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA 2003; 290: 199–206.
Whelton PK, He J, Muntner P . Prevalence, awareness, treatment and control of hypertension in North America, North Africa and Asia. J Hum Hypertens 2004; 18: 545–551.
Acknowledgements
This study was supported by the National 973 Basic Research Program of China (no. 2009CB521900), the National High-tech Research and Development Program of China (no. 2006AA02A406), the Program of Introducing Talents of Discipline to Universities (no. B07035), the State Key Program of National Natural Science of China (no. 60831003) and the Cultivation Fund of the Key Scientific and Technical Innovation Project, Ministry of Education of China (no. 704030).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Yang, J., Lu, F., Zhang, C. et al. Prevalence of prehypertension and hypertension in a Chinese rural area from 1991 to 2007. Hypertens Res 33, 331–337 (2010). https://doi.org/10.1038/hr.2009.235
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2009.235
Keywords
This article is cited by
-
Non-communicable diseases among low income adults in rural coastal communities in Eastern Sabah, Malaysia
BMC Public Health (2019)
-
Prevalence and income-related equity in hypertension in rural China from 1991 to 2011: differences between self-reported and tested measures
BMC Health Services Research (2019)
-
The burden, management rates and influencing factors of high blood pressure in a Chinese rural population: the Rural Diabetes, Obesity and Lifestyle (RuralDiab) study
Journal of Human Hypertension (2018)
-
Urban-rural disparities in hypertension prevalence, detection, and medication use among Chinese Adults from 1993 to 2011
International Journal for Equity in Health (2017)
-
Temporal trends in Prevalence, Awareness, Treatment, and Control of Hypertension from 2000 to 2010 in Chengdu, China
Scientific Reports (2017)