Abstract
A reduction in the blood pressure decline at night (<10% from daytime systolic blood pressure (SBP)) during 24-h ambulatory blood pressure monitoring (ABPM) (‘non-dipping pattern’) is associated with cardiovascular morbidity. Our aim was to evaluate whether ABPM characteristics are associated with metabolic abnormalities in subjects without known hypertension or type 2 diabetes mellitus (T2DM). This is a cross-sectional population-based study on middle-aged subjects (n=462). Two distinct definitions of metabolic syndrome (MetS) were used: National Cholesterol Education Program-Third Adult Treatment Panel (NCEP-ATPIII) and International Diabetes Federation (IDF) criteria. Results suggested that subjects characterized by non-dipping in 24 h ABPM were more obese (P=0.014). After adjustment for body mass index, age and sex, non-dippers had higher very-low-density lipoprotein (VLDL)-cholesterol (P=0.003), total (P=0.029)—and VLDL-triglycerides (P=0.026) and oral glucose tolerance test 2 h blood glucose (P=0.027) compared with dippers. Non-dipping status was more common among subjects with MetS (P⩽0.01), impaired glucose tolerance (IGT) (P<0.05) and in those with the combination of IGT–T2DM (P⩽0.01) than among those without these abnormalities. ABPM non-dipping status was an independent predictor of IGT in multivariate models (P<0.05). With respect to MetS components, high triglycerides (P⩽0.005) and low high density lipoprotein-cholesterol (P<0.05) were associated with a non-dipping pattern. The percentage decline in blood pressure from day to night decreased with the number of metabolic abnormalities (P=0.012). In conclusion, ABPM non-dipping status is an independent predictor of glucose intolerance. It is also associated with several other metabolic abnormalities. Whether non-dipping pattern is causally related to these metabolic aberrations remains to be explored in a future prospective follow-up of this cohort.
Similar content being viewed by others
Introduction
Metabolic syndrome (MetS)1, 2 and non-dipping pattern of blood pressure (that is, when nocturnal systolic blood pressure falls by <10% from the daytime systolic blood pressure values) during 24-h ambulatory blood pressure monitoring (ABPM)3 are two factors which both increase the risk for cardiovascular disease. A non-dipping pattern in ABPM has been reported to be more common in subjects with the MetS in some studies4, 5, 6 although this relationship has not been detected in others.7 In addition, an increase in the prevalence of non-dipping has been observed with the increasing number of MetS components.8 Obesity and nocturnal volume-dependent hypertension have been postulated to be some of5 the factors involved in the pathophysiology of non-dipping pattern in MetS. Earlier data have also provided evidence that there might be an inter-relationship between MetS, enhanced sodium sensitivity of the blood pressure and non-dipping pattern.9
Little is known about the relationship between the circadian profile of blood pressure, dipping pattern and insulin, as well as glucose metabolism in subjects without any known metabolic diseases. Therefore, we investigated the possible association between 24-h blood pressure profile and glucose tolerance status, MetS, as well as its components in a large population-based cohort (n=462) without diagnosed hypertension or diabetes.
Methods
Study population
This study is part of the OPERA (Oulu Project Elucidating Risk of Atherosclerosis) project, which has been described previously.10 In this study, we used the control population from OPERA consisting of 462 (236 female and 226 male) subjects. The OPERA study was approved by the Ethical Committee of the Faculty of Medicine, University of Oulu, and was compatible with the Declaration of Helsinki. Informed consent was obtained from each subject.
We used two distinct new definitions of MetS: National Cholesterol Education Program-Third Adult Treatment Panel (NCEP-ATPIII) and International Diabetes Federation (IDF) criteria.
The NCEP-ATPIII (2005)11 requires the existence of, at least, three of the following risk factors: elevated blood pressure (⩾130/85 mm Hg or drug treatment), increased fasting blood glucose (⩾5.6 mmol l−1, low high-density lipoprotein (HDL)-cholesterol (<1.03 mmol l−1 in men and <1.29 mmol l−1 in women), high triglycerides (⩾1.7 mmol l−1) and abdominal obesity (waist circumference >102 cm in men and >88 cm in women).
According to the IDF definition,12 for persons to be defined as having the MetS, they must have: Central obesity (defined as a condition with waist circumference ⩾94 cm for Europid men and ⩾80 cm for Europid women) plus any two of the following four factors: elevated serum triglyceride level (⩾1.7 mmol l−1) reduced serum HDL-cholesterol level (<1.03 mmol l−1 in males and <1.29 mmol l−1 in females) (or specific treatment for these lipid abnormalities) raised blood pressure (systolic blood pressure ⩾130 mm Hg or diastolic blood pressure ⩾85 mm Hg), or treatment of previously diagnosed hypertension, impaired fasting glycemia (fasting plasma glucose ⩾5.6 mmol l−1), or previously diagnosed type 2 diabetes mellitus (T2DM).
Blood pressure measurements. The office blood pressure (BP) was measured using an automatic oscillometric recorder (Dinamap model 18465X, Criticon, Ascot, UK) when the subjects were seated for at least 5 min. After that BP was measured three times at 1-min intervals. The mean of the second and third measurements was used for the analysis.13
The fully automatic SpaceLabs 90207 oscillometric unit (SpaceLabs, Redmond, Washington, USA) was used for recording ABPM. The unit was set to record a measurement every 15 min from 0400 hours till midnight and every 20 min from midnight till 0400 hours. The accuracy and reproducibility of the BP readings obtained using this device have been established previously.14 The proper positioning of the cuff in each case was ensured by means of the similarity (difference <5 mm Hg) between four SpaceLabs BP measurements and four auscultatory readings using a Y-connector. The subjects were asked to relax their arm during the measurement. Fewer than 3% of the BP readings were rejected as artefacts based on of the criteria described earlier.15
A reduction in systolic blood pressure from daytime to night-time of less than 10% was considered to represent a non-dipping pattern. In addition to dipping status, we also considered the percentage decline in BP from day to night7 ((daytimeBP mean-night-time mean)/daytime BP mean) × 100) as a continuous variable.
Laboratory measurements. All the laboratory test samples were obtained after an overnight fast. Plasma was separated from venous blood and stored at 4°C. Most of the laboratory analyses were carried out within two days after the blood sampling. Subsequently, plasma was stored at 20°C for further analyses. The routine clinical laboratory tests were carried out in the Central Laboratory of Oulu University Hospital, and the lipid and lipoprotein analyses in the Research Laboratory of the Department of Internal Medicine.
After fasting blood had been drawn, the subjects were given a 75-g glucose load, after which blood insulin and glucose levels were determined at 60 and 120 min. The venous blood glucose concentration was determined with the glucose dehydrogenase method and the plasma insulin concentration with the double radioimmunoassay method (AIA-PACK IRI, Tosoh, Tokyo, Japan). Plasma lipids and lipoproteins were analyzed as mentioned previously.13
T2DM and impaired glucose tolerance (IGT) were determined according to the World Health Organization (WHO) criteria.16 A person was regarded as diabetic if his/her fasting blood glucose was ⩾6.1 mmol l−1 and/or 2-h glucose level in oral glucose tolerance test (OGTT) was ⩾10.0 mmol l−1, or if he/she was using diabetes medication (oral or insulin). A subject had IGT if he/she had a fasting blood glucose <6.1 mmol l−1 and his/her 2-h blood glucose in OGTT was ⩾ 6.7 mmol l−1 and <10.0 mmol l−1. Insulin sensitivity was assessed using fasting plasma insulin concentrations and a quantitative insulin sensitivity check index (QUICKI=1/[log (fasting insulin)+log (fasting glucose)]).17
Statistical methods
All statistical tests were made with the SPSS 16 software package (SPSS Inc., Chicago, IL, USA). To normalize the distribution, a logarithm transformation was applied to very low-density lipoprotein (VLDL)-cholesterol, total- and VLDL-triglycerides, fasting and 2-h blood glucose values. The means of continuous variables measured between the categorical variables were compared by the analysis of variance and analysis of covariance with adjustments. The χ2 test was used for evaluating frequencies. P-value <0.05 was considered statistically significant. When we tested the association of dipping status with fasting and 2-h glucose and quick index, subjects with T2DM were excluded. This study cohort included 22 subjects with T2DM.
Logistic regression was used for the prediction of the probability MetS or IGT/T2DM occurrence (grouping variables). The independent discriminatory power of each risk factor was assessed by logistic regression analysis. When MetS was considered, age, sex, smoking habits and dipper status were included in equations. In the case of IGT/T2DM, age, sex, smoking habits, waist, body mass index (BMI) and dipper status were included.
Results
Baseline characteristics of subjects showing a dipping or non-dipping pattern in ambulatory blood pressure monitoring
Non-dipper subjects were older, more obese and had higher VLDL-cholesterol levels, and lower HDL-cholesterol levels and higher total and VLDL-triglyceride levels compared with dippers (Table 1). They were more insulin resistant (that is, had a lower Quick Index) and their 2-h glucose value in OGTT was higher than the corresponding values in dippers. Insulin values during OGTT did not differ between non-dippers and dippers (data not shown). However, non-dippers had lower daytime but higher night-time blood pressure values. As a high BMI was strongly associated with non-dipping status, we included adjustment for BMI in addition to age and sex. The results of the latter analysis revealed that of the above associations, statistical significance remained intact for VLDL-cholesterol (P=0.003), total- (P=0.029) and VLDL-triglycerides (P=0.026), 2-h blood glucose (P=0.027) and for the differences in the ABPM parameters.
The prevalences of dippers and non-dippers in subjects with and without MetS or IGT/T2DM
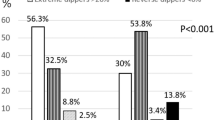
The prevalences of MetS according to IDF and NCEP-ATPIII criteria were 23.3 and 18.1%, respectively. Figure 1 shows the prevalences of subjects with non-dipping and dipping patterns in ABPM monitoring in relation to the independent clinical features of MetS and MetS according to IDF criteria as a cluster. The prevalence of non-dippers was higher than dippers among the subjects with high triglycerides (P⩽0.005) and low HDL-cholesterol (P<0.05), and those with MetS as a cluster per se (P⩽0.01). Similar associations were observed when MetS was defined using the NCEP-ATPIII criteria (data not shown).
The prevalences of subjects with non-dipping and dipping patterns in ABPM monitoring in relation to the independent clinical features of MetS and MetS according to IDF criteria as a cluster are shown. *Statistical significance defined as P<0.05. **Statistical significance defined as P⩽0.01. ***Statistical significance defined as P⩽0.005. ABPM, ambulatory blood pressure monitoring; IDF, International Diabetes Federation.
The percentage decline in BP from day to night (((daytime BP mean−night-time mean)/daytime BP mean) × 100) was reduced in conjunction with the increase in the number of metabolic abnormalities ((P=0.012) (Figure 2). These trends were seen when the two criteria of MetS were used (NCEP-ATPIII (Figure 2) or IDF (data not shown)).
Percentage decline in BP from day to night (((daytime BP mean−night-time mean)/daytime BP mean) × 100) in relation to the number of NCEP-ATPIII criteria of MetS met. Number of subjects is shown in parenthesis. BP, blood pressure; NCEP-ATPIII, National Cholesterol Education Program-Third Adult Treatment Panel.
The prevalence of non-dippers was higher than dippers in the subjects with IGT (P<0.05) and those with the combination of IGT/T2DM (P⩽0.01) (Figure 3).
The prevalences of subjects with non-dipping and dipping patterns in ABPM monitoring in relation to the glucose tolerance status are shown. Statistical significances defined as in Figure 1. ABPM, ambulatory blood pressure monitoring.
ABPM characteristics in subjects with and without MetS
After adjustment for confounding factors (age, sex, smoking habits and alcohol consumption) subjects with MetS were found to have higher ABPM day- and night-time systolic and diastolic values (Table 2). ABPM heart rate during both day- and night-time was higher in the subjects with MetS. After further adjustment for BMI, all the statistical significances disappeared (data not shown).
ABPM characteristics in subjects with and without IGT/T2DM
After adjustment for confounding factors (age, BMI, sex, smoking and alcohol consumption) subjects with IGT/T2DM showed higher ABPM day- and night-time systolic and night-time diastolic values (Table 3).
Logistic regression models of the MetS and IGT/T2DM
We investigated contributing factors to MetS (according to the IDF criteria) and IGT/T2DM by logistic regression models. Non-dipping status was significantly associated with MetS (P=0.011) simultaneously with sex. The results did not change significantly, if the NCEP-ATPIII criteria for defining MetS were used. When the adjustment for BMI was included, non-dipping status was no longer associated with MetS (data not shown).
Furthermore, non-dipping was associated with the presence of IGT/T2DM (P=0.036) in addition to age, sex, smoking habits and waist circumference (Table 4). The inclusion of BMI into the model did not change the significant predictive value of non-dipping status for impaired glucose tolerance (P<0.05).
Discussion
This study indicates that a non-dipping pattern of blood pressure is more common among subjects with MetS. The major, new, finding of this study suggest ABPM non-dipping status to be an independent predictor of glucose intolerance. It has been shown previously that the diurnal–nocturnal differences in blood pressure are smaller among T2DM patients than in controls.18, 19 A reduction in the actions of insulin may be one of the important physiological defects underlying the abnormal circadian rhythm of blood pressure in patients with T2DM and other related diseases.20 Non-dipper hypertensive patients have been shown to be more insulin resistant and glucose intolerant than dipper hypertensive patients.21 Interestingly, insulin resistance is associated with abnormal control of blood pressure and sympathetic activation even in the healthy offspring of T2DM patients.22
Our study cohort included subjects who did not have any previously known abnormality in glucose tolerance but the OGTT revealed that 17% of them showed impaired glucose regulation. Majority of them were in the pre-diabetes state and only a few of them were T2DM patients. In accordance with our results, a recent study, in which insulin sensitivity was not measured, reported that normotensive subjects with impaired glucose tolerance experience more often a non-dipping pattern of blood pressure than those with normal glucose tolerance.23 Our non-dipper subjects were more insulin resistant but they had also more general adiposity such that the effect of non-dipping status on insulin sensitivity was diluted after adjustment for BMI. Thus, obesity is perhaps the most important factor leading to insulin resistance in the subjects with the non-dipping pattern of blood pressure. However, obesity per se does not seem to explain the diurnal–nocturnal differences in blood pressure in subjects with impaired glucose tolerance. Evidence for this proposal is the higher daytime systolic as well as night-time values of both systolic and diastolic blood pressure in those subjects with impaired, in comparison with those with normal glucose, regulation even after adjustment for BMI and other conventional risk factors. In addition, non-dippers had higher 2-h glucose values for OGTT and a higher prevalence of IGT than dippers after adjustment for total adiposity. The role of pancreatic β-cell dysfunction as a link between the non-dipping status and glucose intolerance, as proposed in one study,21 remains undefined in this study.
The heart rate during the whole day was higher in the subjects with MetS, who were also more often non-dippers, supporting the belief that these individuals have elevated sympathetic tone. Stimulation of sympathetic activity has been reported to be able to antagonize insulin-mediated glucose uptake in skeletal muscle.24 In non-dippers, the sympathetic tone is believed to be increased at night, suggesting that they have nocturnal autonomic dysfunction.25 Obese patients have increased prevalence of non-dipping status,26 and in this study, non-dippers had a higher BMI. Obesity is strongly associated with hyperinsulinemia and it may act in concert with the sympathetic nervous system to elevate blood pressure.27 After further adjustment for BMI, all the statistical significances of the ABPM parameters in the prediction of MetS disappeared. Therefore, excessive adiposity is undoubtedly one of the crucial factors associated with ABPM abnormalities among subjects with MetS.
MetS is associated with an increased risk for developing diabetes.28 Non-dipping blood pressure has been reported to be more common in subjects with the MetS in some earlier studies,5, 6, 29 in addition to this study. Adiposity influences all the features of the MetS and the associations of non-dipping status with HDL-cholesterol, as well as with MetS as a cluster observed in our study were dependent on the amount of body fat. However, associations of high VLDL-cholesterol and -triglycerides and total triglycerides with non-dipping status were independent of total adiposity. Hypertriglyceridemia, a high level of VLDL and a low level of HDL cholesterol characterize the type of dyslipidemia associated with IGT, T2DM and MetS.28 The fundamental defect is believed to be the overproduction of large VLDL particles, which initiates a sequence of lipoprotein changes.30 The mechanism behind the increase of triglyceride-rich particles among non-dippers remains unclear in our study, as it was not related to the obesity or the associated insulin resistance. It has been shown previously that the levels of plasma free fatty acids correlate with glucose tolerance independently of total adiposity.31 Therefore, increased blood glucose levels among non-dippers may trigger a reduced catabolism of lipoproteins rich in triglycerides by lipoprotein lipase and an increase in their fasting and postprandial levels.
In conclusion, our findings demonstrate that ABPM non-dipping status is an independent predictor of glucose intolerance. In addition, non-dipping is related to obesity and associated insulin resistance, plasma lipid abnormalities as well as the combined occurrence of metabolic abnormalities. The use of a single 24-h ABPM is the major limitation of this study. Prospective studies are needed to clarify whether a non-dipping pattern is predictive of more severe metabolic abnormalities.
Conflict of interest
The authors declare no conflict of interest.
References
Isomaa B, Almgren P, Tuomi T, Forsén B, Lahti K, Nissén M, Taskinen MR, Groop L . Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 2001; 24: 683–689.
Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, Salonen JT . The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA 2002; 288: 2709–2716.
Cuspidi C, Meani S, Valerio C, Fusi V, Zanchetti A . Nocturnal non-dipping pattern in untreated hypertensives at different cardiovascular risk according to the 2003 ESH/ESC guidelines. Blood Press 2006; 15: 37–44.
Hassan MO, Jaju D, Albarwani S, Al-Yahyaee S, Al-Hadabi S, Lopez-Alvarenga JC, Rizvi SG, Comuzzie AG, Bayoumi RA . Non-dipping blood pressure in the metabolic syndrome among Arabs of the Oman family study. Obesity (Silver Spring) 2007; 15: 2445–2453.
Tartan Z, Uyarel H, Kasikcioglu H, Alper AT, Ozay B, Bilsel T, Gul M, R, N . Metabolic syndrome as a predictor of non-dipping hypertension. Tohoku J Exp Med 2006; 210: 57–66.
Hermida RC, Chayán L, Ayala DE, Mojón A, Domínguez MJ, Fontao MJ, Soler R, Alonso I, Fernández . Association of metabolic syndrome and blood pressure nondipping profile in untreated hypertension. Am J Hypertens 2009; 22: 307–313.
Cuspidi C, Meani S, Fusi V, Severgnini B, Valerio C, Catini E, Sala C, Magrini F, Zanchetti A . Is the nocturnal fall in blood pressure reduced in essential hypertensive patients with metabolic syndrome? Blood Press 2004; 13: 230–235.
Vyssoulis GP, Karpanou EA, Kyvelou SM, Adamopoulos DN, Deligeorgis AD, Spanos PG, Pietri PG, Cokkinos DF, Stefanadis CI . Nocturnal blood pressure fall and metabolic syndrome score in hypertensive patients. Blood Press Monit 2007; 12: 351–356.
Uzu T, Kimura G, Yamauchi A, Kanasaki M, Isshiki K, Araki S, Sugiomoto T, Nishio Y, Maegawa H, Koya D, Haneda M, Kashiwagi A . Enhanced sodium sensitivity and disturbed circadian rhythm of blood pressure in essential hypertension. J Hypertens 2006; 24: 1627–1632.
Rantala AO, Kauma H, Lilja M, Savolainen MJ, Reunanen A, Kesäniemi YA . Prevalence of the metabolic syndrome in drug-treated hypertensive patients and control subjects. J Intern Med 1999; 245: 163–174.
Grundy SM, Hansen B, Smith Jr SC, Cleeman JI, Kahn RA, American Heart Association, National Heart, Lung, and Blood Institute, American Diabetes Association. Clinical management of metabolic syndrome: report of the American Heart Association/National Heart, Lung, and Blood Institute/American Diabetes Association conference on scientific issues related to management. Circulation 2004; 109: 551–556.
Alberti KG, Zimmet P, Shaw J . IDF Epidemiology task force consensus group. The metabolic syndrome—a new worldwide definition. Lancet 2005; 366: 1059–1062.
Huikuri HV, Ylitalo A, Pikkujämsä SM, Ikäheimo MJ, Airaksinen KE, Rantala AO, Lilja M, Kesäniemi YA . Heart rate variability in systemic hypertension. Am J Cardiol 1996; 77: 1073–1077.
O’Brien E, Coats A, Owens P, Petrie J, Padfield P, Littler WA, de Swiet M, Mee F . Use and interpretation of ambulatory blood pressure monitoring: recommendations of the British Hypertension Society. BMJ 2000; 320: 1128–1134.
Ylitalo A, Airaksinen KEJ, Tahvanainen KUO, Kuusela TA, Ikäheimo MJ, Rantala A, Lilja M, Huikuri HV . Baroreflex sensitivity in drug-treated systemic hypertension. Am J Cardiol 1997; 80: 1369–1372.
Alberti KG, Zimmet PZ . Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 1998; 15: 539–553.
Katz A, Nambi SS, Mather K, Baron AD, Follmann DA, Sullivan G, Quon MJ . Quantitative insulin sensitivity check index: a simple, accurate method for assessing insulin sensitivity in humans. J Clin Endocrinol Metab 2000; 85: 2402–2410.
Kondo K, Matsubara T, Nakamura J, Hotta N . Characteristic patterns of circadian variation in plasma catecholamine levels, blood pressure and heart rate variability in Type 2 diabetic patients. Diabet Med 2002; 19: 359–365.
Perk G, Mekler J, Ben Ishay D, Bursztyn M . Non-dipping in diabetic patients: insights from the siesta. J Hum Hypertens 2002; 16: 435–438.
Nakano S, Kitazawa M, Tsuda S, Himeno M, Makiishi H, Nakagawa A, Kigoshi T, Uchida K . Insulin resistance is associated with reduced nocturnal falls of blood pressure in normotensive, nonobese type 2 diabetic subjects. Clin Exp Hypertens 2002; 24: 65–73.
Chen JW, Jen SL, Lee WL, Hsu NW, Lin SJ, Ting CT, Chang MS, Wang PH . Differential glucose tolerance in dipper and non-dipper essential hypertension: the implications of circadian blood pressure regulation on glucose tolerance in hypertension. Diabetes Care 1998; 21: 1743–1748.
Frontoni S, Bracaglia D, Baroni A, Pellegrini F, Perna M, Cicconetti E, Ciampittiello G, Menzinger G, Gambardella S . Early autonomic dysfunction in glucose-tolerant but insulin-resistant offspring of type 2 diabetic patients. Hypertension 2003; 41: 1223–1227.
Li L, Soonthornpun S, Chongsuvivatwong V . Association between circadian rhythm of blood pressure and glucose tolerance status in normotensive, non-diabetic subjects. Diabetes Res Clin Pract 2008; 82: 359–363.
Lembo G, Capaldo B, Rendina V, Iaccarino G, Napoli R, Guida R, Trimarco B, Saccá L . Acute noradrenergic activation induces insulin resistance in human skeletal muscle. Am J Physiol 1994; 266: E242–E247.
Kohara K, Nishida W, Maguchi M, Hiwada K . Autonomic nervous function in non-dipper essential hypertensive subjects. Evaluation by power spectral analysis of heart rate variability. Hypertension 1995; 26: 808–814.
Kotsis V, Stabouli S, Bouldin M, Low A, Toumanidis S, Zakopoulos N . Impact of obesity on 24-h ambulatory blood pressure and hypertension. Hypertension 2005; 45: 602–607.
Corry DB, Tuck ML . Obesity, hypertension, and sympathetic nervous system activity. Curr Hypertens Rep 1999; 1: 119–126.
Cornier MA, Dabelea D, Hernandez TL, Lindstrom RC, Steig AJ, Stob NR, Van Pelt RE, Wang H, Eckel RH . The metabolic syndrome. Endocr Rev 2008; 29: 777–822.
Vyssoulis G, Karpanou E, Adamopoulos D, Kyvelou SM, Gymnopoulou E, Cokkinos D, Stefanadis C . Nocturnal blood pressure fall and metabolic syndrome score in patients with white coat hypertension. Blood Press Monit 2008; 13: 251–256.
Adiels M, Olofsson SO, Taskinen MR, Borén J . Overproduction of very low-density lipoproteins is the hallmark of the dyslipidemia in the metabolic syndrome. Arterioscler Thromb Vasc Biol 2008; 28: 1225–1236.
Pouliot MC, Després JP, Nadeau A, Tremblay A, Moorjani S, Lupien PJ, Thériault G, Bouchard C . Associations between regional body fat distribution, fasting plasma free fatty acid levels and glucose tolerance in premenopausal women. Int J Obes 1990; 14: 293–302.
Acknowledgements
We acknowledge the excellent technical assistance of, Ms Helena Kalliokoski, Ms Saija Kortetjärvi, Ms Sirpa Rannikko and Ms Liisa Mannermaa. This study was supported by the Medical Council of the Academy of Finland and the Finnish Foundation for Cardiovascular Research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ukkola, O., Vasunta, RL. & Kesäniemi, Y. Non-dipping pattern in ambulatory blood pressure monitoring is associated with metabolic abnormalities in a random sample of middle-aged subjects. Hypertens Res 32, 1022–1027 (2009). https://doi.org/10.1038/hr.2009.137
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2009.137
Keywords
This article is cited by
-
Non-dipping blood pressure pattern is associated with cardiovascular events in a 21-year follow-up study
Journal of Human Hypertension (2024)
-
Chronotherapy for Hypertension
Current Hypertension Reports (2018)
-
Cardioprotective effects of SGLT2 inhibitors are possibly associated with normalization of the circadian rhythm of blood pressure
Hypertension Research (2017)
-
Nondipping Pattern and Carotid Atherosclerosis in a Middle-Aged Population: OPERA Study
American Journal of Hypertension (2012)