Abstract
In 1993, the first effective enzyme replacement therapy for a genetic disease, Ceredase (Genzyme Corporation, Cambridge, MA), was approved for use in patients with Gaucher disease. Over the next 13 years, enzyme replacement therapy became clinically available for the treatment of Fabry disease, mucopolysaccharidosis Type I, mucopolysaccharidosis Type II, mucopolysaccharidosis Type VI, and glycogen storage disease Type II. The development of enzyme replacement therapy to treat lysosomal storage diseases has resulted in an increasing number of genetic patients undergoing weekly or biweekly intravenous enzyme replacement therapy and an expanded role of the genetics team to include comprehensive care involving therapeutic intervention for lysosomal storage diseases. This article describes the development of two outpatient genetics-based infusion centers: the Northshore Genetics Infusion Clinic as part of the Children's Hospital of Wisconsin Lysosomal Diseases Treatment Center in conjunction with the Medical College of Wisconsin and the Emory Lysosomal Storage Disease Center for Genetic Infusions in the Emory University Department of Human Genetics.
Similar content being viewed by others
Main
In 1993, the first effective enzyme replacement therapy (ERT) for a genetic disease, Ceredase (Genzyme Corporation, Cambridge, MA), was approved for use in patients with Gaucher disease. Over the next 13 years, ERT became clinically available for the treatment of Fabry disease (2003), mucopolysaccharidosis Type I (2003), mucopolysaccharidosis Type VI (2005), mucopolysaccharidosis Type II (2006), and glycogen storage disease Type II (2006). The development of ERT to treat lysosomal storage diseases (LSDs) has resulted in an increasing number of genetic patients undergoing weekly or biweekly intravenous ERT and an expanded role of the genetics team to include comprehensive care involving therapeutic intervention for LSDs. The expanded role moves geneticists and genetic counselors beyond the traditional diagnostic role and into that of an interventionist. The interventionist genetics team leads discussions about the timing of treatment initiation, the limitations of ERT, the management of infusion-related reactions, the placement of ports or other access devices, the psychosocial implications of frequent intravenous infusions, and conduction of specialist appointments. The clinical complexity of the management and infusion of patients has only become more complicated as ERT has become available for more genetic diseases.
The Genetics Center at the Children's Hospital of Wisconsin (CHW) provides care for adults, teens, and children with genetic disorders and birth defects. The CHW Lysosomal Disease Treatment Center (CHW LDTC) was organized within the Genetics Center in 2003 to manage and treat the significant number of existing Fabry patients (15) and to aid in diagnosing their family members. After FDA approval of Fabrazyme in April 2003, we and our current patients and their affected family members were eager to begin using this new medication. It became apparent that our CHW Infusion Center would not be able to provide infusions to adults, primarily those with Medicare, because of poor reimbursement for the medication and infusion costs. Because the hospital is designated as an official children's hospital, it receives only a fraction of typical reimbursement by Medicare. In addition, several regional adult medical facilities were found to be unwilling to provide Fabrazyme to the ever-increasing patient population because of its new FDA-approved status, its high cost, and their lack of infusion chairs to accommodate our patient numbers.
When considering the experience of infusing the first Fabry patients within the CHW system, it quickly became apparent that reimbursement was not equal to the time spent coordinating infusions. The drawbacks of the initial noncentralized system are described well by the strengths, weaknesses, opportunities, and threats (SWOT) analysis seen in Table 1. Based on their experiences, the CHW LDTC center moved quickly and was able to offer treatment to adults in an off-site genetics-based infusion center since its opening in October 2003, just 6 months after FDA approval of Fabrazyme.
Since 2003, the CHW LDTC has expanded to provide comprehensive care and treatment for a variety of patients with LSDs. The center includes three medical geneticists and three genetic counselors in an academic setting. Individuals from Wisconsin (WI) and neighboring Michigan and Illinois comprise the patient population of 71, which includes individuals with the following LSDs: Fabry (51), Gaucher Type I (6), mucopolysaccharidosis Type I (2), mucopolysaccharidosis Type II (2), mucopolysaccharidosis Type III (7), metachromatic leukodystrophy (3), and mucopolysaccharidosis Type IV (2). None of these patients are currently ventilated. The CHW infusion center now infuses 9 patients who represent 7.8% of their LSD patient population. The genetics team at CHW found the genetics-based infusion center to be helpful not only to provide treatment to patients who live locally, but also to use as a safe and experienced site to initiate treatment for new patients throughout the referral area. The remainder of the patient population is infused at local infusion centers or through home infusions.
The Division of Medical Genetics within the Emory Department of Human Genetics provides care for children, adolescents, and adults with genetic disorders, metabolic conditions, and birth defects. The Emory Lysosomal Storage Disease Center (ELSDC) was established in 1993 within the Division of Medical Genetics to provide diagnostic, evaluation, management, and treatment services for patients affected by lysosomal storage disorders. In 1993, the only FDA-approved ERT available was Ceredase for the treatment of Gaucher disease. Most patients began receiving infusions at local ambulatory outpatient oncology infusion centers then moved to home infusions when stable. As no one in this population was ventilated and Gaucher disease symptoms responded so well to ERT, home infusions were an excellent option. In 2003, the rapid increase in the number of patients being offered ERT placed a strain on the ambulatory infusion centers, and they began to tightly restrict the times and dates for which a patient would be infused. In addition, the facilities had difficulties rescheduling patients who missed infusions, managing drug inventory so that the ERT would be available on the patients' infusion day, and correctly billing the patient's insurance so that they would be accurately reimbursed for the drug cost and infusion services. In addition, the ELSDC genetics team found that they were spending significant portions of their days scheduling infusions, providing the ambulatory infusion centers with a new set of orders for each infusion, checking drug supply to ensure it would be available for an infusion date, and working with patients to resolve billing issues. All of these coordinating activities were not billable as they were performed when the patient was not in clinic. The team quickly determined that a genetic infusion center would be an important addition to the center. The decision to create the Emory Center for Genetic Infusions was made in the fall of 2003. The risks and benefits considered during this process are well described by the SWOT analysis seen in Table 1.
Since 2003, the ELSDC center has expanded to include one medical geneticist, five genetic counselors, one nurse coordinator, and one infusion nurse in an outpatient academic setting. The center's main patient population includes individuals from Georgia (GA), South Carolina, Tennessee, Alabama, and Florida. The current patient population includes around 202 individuals with the following LSDs: Fabry (103), Gaucher Type I (54), Gaucher Type III (1), mucopolysaccharidosis Type I (12), mucopolysaccharidosis Type II (10), mucopolysaccharidosis Type IV (4), mucopolysaccharidosis Type VI (2), Niemann Pick Type B (1), Niemann Pick Type C (2), infantile onset Pompe (4), late onset Pompe (4), late onset Tay Sachs (1), metachromatic leukodystrophy (2), fucosidosis (1), GM1 gangliosidosis (1), and mucolipidosis Type II (1). Currently, one of the infantile onset Pompe patients is ventilated; one later onset MPS II patients and one GM1 gangliosidosis patient have tracheotomies. Medically stable children, adolescents, and adults undergoing ERT have been offered treatment in the genetics-based infusion center since its opening in September of 2005. The infusion center now infuses 26 patients who represent 13% of their LSD patient population. Given the wide geographic catchment areas represented in the Emory LSDC patient population, only local patients (within ∼3 hr of the center) begin infusions in the ELSDC infusion center and then move to home infusions or closer centers after they are stable.
EVALUATING FINANCIAL MODELS
The first critical step in creating an infusion center is the development of a financial model that considers current institutional relationships, regulations (federal, state, and local) governing ERT infusions, size and demographics of the existing patient population, cost of the medications, use of pharmaceutical distributors to provide ERT medications, reimbursement for medications and services, infusion provision space, facility fees, staff costs and availability, contracted rates for reimbursement at each institution, and the ability to expand in future. If a projected financial model determines that an infusion center would not be profitable or would only break even, it would make poor financial sense to move forward.
In developing financial models, the WI and GA centers used both internal resources and external information available on outpatient, physician office-based intravenous infusion centers in hematology/oncology, rheumatology, and neurology.1–3
The WI group developed their center primarily for adult LSD patients, including uninsured patients and those with Medicare and Medicaid. The center projected that it would have eight initial infusion patients. Given the poor reimbursement for ERT drug for adults by Medicare due to its designation as a children's hospital, it was determined that all ERT should be delivered either through a pharmaceutical distributor for patients with commercial insurance or purchased by the academic center directly from the manufacturer for patients with Medicare and Medicaid. Through utilization of existing space and staffing at an off-site location, start-up costs were minimal (Table 2).
The GA center initially planned to infuse 12 medically stable LSD patients of all ages with several different insurance plans. None of these patients was ventilated or had a tracheotomy, but the center decided that any such individuals seeking infusion treatments who were medically stable could be infused at the center. Given the expanding patient population and likelihood of FDA approval of ERT for other LSDs, the center was created to handle a larger patient load. Unlike the WI center, the GA center was unable to accept Medicare patients, and most patients had Medicaid or private insurance. The financial model created by the GA center focused on careful financial review of each patient's insurance, the institutions' managed care contracts, and profit margins for each drug based upon the average wholesale price of the medication (Fig. 1). If a patient's financial calculation projects a profit, drug is purchased directly from the supplying pharmaceutical company and billed by the center to the patient. If an individual's calculation is projected to lose money, the drug is ordered through a distributor, as they purchase the drug at a reduced cost from the manufacturer. It was determined that Cerezyme has a very low average wholesale price and would always be ordered through a distributor.
See Table 2 for the estimated start up costs for the GA center. The main start-up costs included purchase of infusion chairs and pumps. Other durable supply costs were minimal. During the first 3 months of operation, the GA center had ∼$348,000 in ERT expenses: however, it was quickly realized that accounts payable was paying each invoice on receipt rather than using the negotiated time delay between invoice date and payment due. If the invoices have been held and paid in the third month of operation, most of the cost of the ERT medications would have been covered by the incoming payments. In the third month of operations, a system of invoice payment based on the negotiated terms with the companies was instituted to allow time for payments to be received by the center. The improved system decreased the amount of funds required to be in reserve for medication costs.
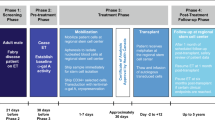
The WI and GA centers decided to provide care for individuals beginning ERT treatment and needing close monitoring for at least 6 months before giving the patient the option to transfer to home infusions or an outpatient infusion center nearer to them, if such an option were available. The 6-month infusion initiation period allows for monitoring of infusion reactions and adjustment of the premedication regimen and infusion rate, if necessary to combat reactions. The expectation was that some patients would prefer to be infused at the centralized infusion center and would choose to stay there beyond the point of stabilization. In this model, however, new patients are important to the continued profitability of the centers.
After developing financial models, both centers used the SWOT analysis to analyze the utility of the genetics-based infusion center and validate the business plan further. The SWOT analysis suggested that, despite a few challenges, an infusion center was a financially viable method of satisfying unmet patient need at Emory (see Table 1).
CREATING THE GENETICS-BASED INFUSION CENTER
When the genetics center teams determined that the genetics-based infusion center model would meet patient needs and be profitable, start-up funds were designated by the departments, and responsibilities were distributed among the involved team members.
Infusion space
The two centers took different approaches for the development of infusion space. To decrease time and costs until start up of a new clinic, the WI group found underused space in an existing clinic area, and infusions occurred during a day when the clinic space was not being used. The GA group was in the process of relocating to a designated genetic building and was able to design an infusion space in a dedicated location. In this case, the infusion center team met with architects to design and furnish the space specifically for the genetics-based infusion center. This decision to renovate an existing space increased the time to the opening of the infusion center. Both spaces had essential components that included: infusion space for chairs or beds, triage space, an entertainment/waiting area, a drug preparation area, and access to bathrooms. Given the length of infusions (5–8 hr in some patients), close attention to entertainment options and sleeping space was particularly important to the effective development of the centers.
Equipment
Basic equipment needed for genetics-based infusion centers was obtained through standard medical suppliers. The equipment required includes infusion chairs, infusion pumps, catheters, correct intravenous tubing with extensions, intravenous poles, dressings, vital signs monitoring equipment, locking refrigerator with backup power, gloves, needles, syringes, saline (500, 250, 100 mL bags), binders (to hold standing orders, billing slips, and related patient paperwork), and medications and supplies to manage complications (crash kit, automated external defibrillator, antihistamines, corticosteroids, epinephrine, intravenous fluids, etc.). As seen in Table 2, start-up supply costs, not including ERT, were ∼$50,000 for the GA center and slightly less for the WI center as they used existing chairs and chose to rent pumps at $80 per pump per month for the infusions.
Staffing
The WI and the GA group were able to use existing staff within their billing departments to submit claims and billing. The WI billing staff was a single individual within the academic center administration. The GA billing occurred through the existing staff in the Emory Genetics Laboratory billing team, located in the same building as the infusion center. Charge slips were developed as collaboration between the billing staff and the ELSDC team. The cost of these billing services was included in the overhead paid to each of the center's departments. It was important that the designated billing person be very familiar with the codes, claims, and payments used in the infusion center.
The WI group employed two shared nurses from the hospital and two geneticists from within their genetics center to infuse patients and to provide medical supervision. Nurses were trained in the correct procedure for reconstitution and administration of medications. An outpatient clinic manager became the infusion center coordinator who scheduled and monitored staff and ordered supplies for the infusion clinic. The current genetic counselors provided case management by initiating and tracking insurance authorizations, scheduling and facilitating genetics and specialty clinic visits, and assisting with patients' transitions to home infusion or local infusion centers.
The GA group hired a home infusion nurse with pediatric and adult experience for infusions and employed existing nurses, phlebotomists, and physicians as needed. The GA center also created a part-time infusion center coordinator position that was filled by an existing genetic counselor that was familiar with the patients, scheduling, billing system, medications, and ordering systems.
Billing
The WI and GA groups chose to use the standard CMS 1500 form. To maximize reimbursement, a physician needed to be on site during all infusions and document their direct supervision in the patient's record. In addition, special attention was paid to insurance issues before treatments. Prior authorizations and referrals were obtained to cover the entire group of physicians, applicable current procedural terminology (CPT) codes, and the medications.
In both centers, three methods were used for obtaining the medication. First, patients who had no insurance were directed to enroll in nonprofit and pharmaceutical needs-based programs that provided funding for infusions and medications such as Patient Services Incorporated and the National Organization of Rare Disorders. Second, it was determined that many patients with pharmaceutical benefits should have their ERT medication supplied by specialty pharmacies that had contracted with their insurance carriers. Because most patients with LSDs require lifelong treatment, saving medical benefit dollars for them is a priority. Because most insurance carriers will allow payment for the medication through either their pharmaceutical or medical benefits, the WI group opted to use the pharmaceutical option whenever possible. The GA group followed a plan of analyzing each patient's insurance situation individually and using a distributor for any patient with a very low (or negative) profit margin. Lastly, the GA practice purchased medication directly from the pharmaceutical company for patients enrolled in Medicare Part B or those whose private insurance would adequately cover the cost of purchasing the medication. Before purchasing drug directly from a pharmaceutical company, the group negotiated with the pharmaceutical companies to establish the optimal time between invoice and payment due date. A gap of 60 to 90 days between drug invoicing and payment allows an opportunity to receive insurance payments before the drug payment is due, particularly if electronic billing is used. These terms can reduce the amount of funds needed to purchase drugs during the start-up period. However, it is still important to keep payments in reserve in case insurance payments are delayed.
To justify staff usage, both teams determined the appropriate set of CPT-4 codes used for physician billing, set a price for each CPT-4 code that would allow the practice to cover its costs, developed a billing document specific to enzyme replacement infusion therapy, and entered the patient appointment data into a centralized billing system after each infusion. Care was taken to monitor any CPT billing coding changes from year to year (for example, a sample of current infusion CPT codings being used are: 90765-intravenous infusion, for therapy, prophylaxis, or diagnosis, initial, up to 1 hour, and 90766-intravenous infusion, for therapy, prophylaxis, or diagnosis, initial, each additional hour, up to 8 hours). In addition, careful attention was paid to setting the price for any ERT purchased directly from the pharmacy company so as to obtain fair reimbursement without disproportionate cost to patient insurance. To track the charges and payments for both the physician and medication components, monthly billing reports were generated, as well as quarterly profit and loss statements. Any quarterly changes in Medicare and Medicaid coding and billing requirements were followed closely.
Center procedures and emergency plan
The first step in developing center procedures involved determining the schedule of patient infusions and number of days per week available for infusions. The WI genetics-based infusion center decided to provide two seatings of four patients each during a single day of infusion. The two seatings were possible as the eight patients were affected by Fabry disease and had a standard infusion of 4 hours each. The GA center originally determined that two 10-hour infusion days with two or more seatings would provide adequate time for infusions, but later expanded to 3 days to meet the increased demand for infusions. The infusion schedule of the GA patients was complicated by the differing lengths of infusions depending on the patient's condition and stability. For example, several Gaucher patient infusions took 1½ hours, whereas adult onset Pompe patients or Fabry patients being treated for infusion associated reactions took up to 8 hours.
A detailed procedure was developed to effectively schedule, check in, infuse, monitor, provide follow-up for, maintain patient confidentiality of, and bill patients. This procedure also included an emergency plan. Both centers are outpatient facilities with a crash cart and external defibrillator on site, but would need to call an ambulance for further treatment. A trial run of center procedures and emergency plans was scheduled before the centers began infusing patients.
Validation of enhanced patient care and satisfaction
Although no long-term formal surveys were provided to the patients to assess their satisfaction with the genetics-based infusion centers, a set of facility questionnaires, informal telephone-based surveys, individual comments, and an accounting of patient compliance with infusions were collected to assess patient impressions of the centers.
In GA, patient infusion compliance was excellent as measured over the first 6 months at the genetic infusion center. In the first cohort of 12 infused patients, 33% (4/12) patients missed no infusions, 42% (5/12) missed only one infusion, and 25% (3/12) missed two infusions. Within that cohort, three individuals were infused every week. In some patients, this data are in stark contrast to the compliance record of their infusions at the outpatient cancer center. As an extreme example, one GA patient only received four infusions in 6 months at the outpatient oncology center (30% compliance), but at the genetics-based infusion center only missed two infusions in 6 months, (84% compliance).
In WI, the center reported an excellent compliance rate with an average of only one infusion missed on average per patient in the first year of operations. The WI patients were very satisfied as they would not have been able to be treated with ERT at all without the WI genetics infusion center.
The genetics-based infusion centers provided increased patient satisfaction. Over the years of operations, patients have provided verbal and written comments at both centers, stating their positive impression of their infusion location. An informal survey of the first 12 individuals infused at the GA infusion center found that 75% (9/12) were “extremely satisfied” with their infusions at the genetic infusion center and the remaining 25% were “very satisfied.” The same 12 individuals most frequently reported that their increased satisfaction was related to ease of scheduling and rescheduling infusions, frequent contact with the genetics team, and having the same experienced infusion nurse performing infusions at each visit. Another top reason for increased patient satisfaction was the enjoyment of spending time with other patients in an informal support group setting. Two Emory infusion patients (one early onset Pompe disease and one Fabry disease) even returned from home therapy to the genetics-based infusion center, because they preferred the infusion center to home therapy.
The WI group found similar results among their patients: (6/6) of the initial patients reported being extremely satisfied or very satisfied with the genetics-based infusion center. Spontaneous patient use of the infusion center as an informal support group was stronger in the initial eight patients who were Fabry males of similar background than the current, more heterogeneous population. Of the current heterogeneous population, however, all rated the opportunity of speaking to other patients as one of the three most important benefits, in addition to their appreciation for nursing skill at placing IVs and nursing experience with ERT.
From the patient and provider prospective, the genetics-based infusion centers also provided enhanced patient care as patients could easily be seen by the genetics team during their infusions. Additionally, the fixed infusion schedule increased ease in scheduling labs, critical assessments, and specialist evaluations before or after the infusions.
Lessons learned
Although the main focus of the article has been the initial development of the infusion centers, over the course of the 3–5 years that the centers have operated, there have been several key lessons learned. The first lesson is that the financial model for purchasing drug directly from the supplier can be positively impacted if the infusion center is located in a 340B hospital that can be given 340B pricing on drugs. The 340B Drug Pricing Program is part of Public Law 102–585, the Veterans Health Care Act of 1992, which is codified as Section 340B of the Public Health Service Act. In essence, section 340B limits the cost of covered outpatient drugs to certain federal grantees, federally qualified health center look-alikes, and qualified disproportionate share hospitals. Significant savings on pharmaceuticals may be seen by those entities that participate in this program.
Another critical lesson is that precertification, referrals, and reimbursement must be tracked extremely closely for insurance issues. For example, as new ERT drugs are approved, they are billed using a nonspecific HCPCS Code (“J-code”) J3490 until CMS assigns a specific code. Code J3490 is a nonspecific code, and most insurance companies will not automatically pay for the code or the related infusion costs. To obtain reimbursement, detailed lists of infusion dates, times, and information about the medication (including NDC number) must be forwarded to the insurance with each claim.
A final lesson is to remember to account for overhead charges. Overhead is highly variable depending on the infusion center's operating costs and its location in an institution. “Hidden” charges such as overhead impact the final net profit of the center and can make the difference between profit and loss.
CONCLUSIONS
The combined experiences of the CHW LDTC and the ELSDC demonstrate that genetics-based infusion centers can be designed to fit each institution's specific needs while providing an elegant solution to the problems faced with a decentralized infusion program. Ultimately, the genetics-based infusion centers enhanced patient care, increased patient satisfaction, provided a combined treatment and support group function, allowed easier follow-up and care of patients, strengthened the relationship between the patients and the genetic team, attracted new patients, and provided some financial support for clinical genetic services.
In both centers, the break-even point was reached at ∼18 months after opening, and the centers' financial model was validated (see Figs. 2 and3). Although some adjustment of billing costs and drug purchase was required to adapt to changes in patient population, the financial model of projection in both centers proved to be a fair estimate. We have demonstrated that profits have continued in the following years.
References
Baker JJ, Leovic TM, O'Connor CA, Pierce CA . Relocating rheumatology patients to a new infusion center at Duke: a case study. Health Care Manag 2003; 22: 159–169.
Baker JJ, Bray M, Seashore B . Reclassifying infusion therapy space at the University of Arizona: a case study. Health Care Manag 2003; 22: 203–210.
Rossman HS, Lawson S . Setting up a neurology-based infusion center: rationale and guidelines. Appl Neurol 2005; 1: D1–D8.
Acknowledgements
The Wisconsin group acknowledges the work of the infusion nurses, Karin Thao-Vang, Lynn Monfre, and Kris Smith, the billing specialists Rachel Cowan and Pamela Dorna, and the Children's Hospital of Wisconsin Genetics Center staff and management. The Georgia group acknowledges the hard work of the billing and operations team, Brian Burns, Carol Holman, Ken Loud, Sade Loye, and Latasha Alexander, the infusion nurse, Trudi Holbrook, and the Emory lysosomal storage disease team.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure: The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Laney, D., White, A., Rhead, W. et al. Creating genetics-based infusion centers: a case study of two models. Genet Med 10, 626–632 (2008). https://doi.org/10.1097/GIM.0b013e31818050a2
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1097/GIM.0b013e31818050a2