Abstract
Background
To develop an algorithm based on the ocular pulse amplitude (OPA) to predict the probability of a positive temporal artery biopsy (TAB) result in the acute phase of suspected giant cell arteritis (GCA).
Methods
Unilateral TAB was performed and ipsilateral OPA measurements were taken by Dynamic Contour Tonometry. Among the clinical signs and laboratory findings tested in univariate analyses, OPA, Erythrocyte Sedimentation Rate (ESR) and thrombocyte count showed a strong association with a positive TAB result. Algorithm parameters were categorized into three groups (OPA >3.5, 2.5–3.5, and <2.5 mm Hg; ESR <25, 25–60, and >60 mm/h; thrombocyte count <250'000, 250'000–500'000, and >500'000/μl). Score values (0, 1, and 2) were attributed to each group, resulting in a total score range from 0 to 6. A univariate logistic regression analysis using the GCA diagnosis as the dependent and the total score as the independent variate was fitted and probability estimates were calculated.
Results
Thirty-one patients with suspected GCA undergoing TAB during an eighteen-month observation period were enrolled. Twenty patients showed histologically proven GCA. Four patients had score values ≤2, fourteen between 3 and 4, and thirteen of ≥5. The corresponding estimated probabilities of GCA were<7, 52.6, and >95%.
Conclusion
The present study confirms previous findings of reduced OPA levels, elevated ESR, and elevated thrombocyte counts in GCA. It indicates that a sum score based on OPA, ESR, and thrombocyte count can be helpful in predicting TAB results, especially at the upper and the lower end of the sum score range.
Similar content being viewed by others
Introduction
Giant cell arteritis (GCA) represents a diagnostic challenge for the clinician. Early diagnosis is a necessity as treatment with high-dose corticosteroids is effective and leads to prevention of progression of the potentially devastating disease.1 However, the diagnostic value of individual clinical features and optimal diagnostic procedures in patients with suspected GCA is subject of on-going discussions.2 There is recent evidence that the frequently employed American College of Rheumatology criteria should not be used to determine the presence or absence of GCA and that all patients suspected of having GCA should undergo a temporal artery biopsy (TAB).3, 4 On the other hand, TAB is a surgical procedure and not without risk and discomfort for the patient.5 To avoid unnecessary procedures, the diagnosis should be sufficiently likely to justify a biopsy. Elevated erythrocyte sedimentation rates (ESR) and elevated thrombocyte counts proved to be useful objective markers of positive TAB results, unlike many of the clinical features commonly found in patients with GCA.6, 7 In the presence of elevated acute phase reactants, new features in elderly individuals, such as unexplained pain located above the neck, should prompt us to consider the possibility of GCA and the need for TAB. A classic study showed that an abnormal temporal artery on physical examination (i.e., tender, swollen, nodular or with reduced pulse) was associated with high predictive value for a positive TAB.8 However, sensitivity of the TAB varies in different studies. Therefore, the search for additional tools that may improve the sensitivity of TAB is of main importance in patients with suspected GCA.
The ocular pulse amplitude (OPA) represents the extension of the pulsatile oscillations of the intraocular pressure during the cardiac cycle. In healthy subjects we measured values ranging from 0.9–7.2 mm Hg with a median value of 3.0 mm Hg.9 As it has been shown to be markedly reduced in GCA, it may be helpful in predicting the likelihood of positive TAB results.10, 11, 12, 13 It is the purpose of the present study to develop an algorithm based on non- or minimally invasive methods including the OPA to quantify the probability that a patient with suspected GCA will have a positive histological analysis.
Materials and methods
This was a prospective single centre cohort study performed at the Department of Ophthalmology, University Hospital of Zurich. All patients with suspected GCA between October 2007 and March 2009, consenting for both TAB and study participation, were enrolled consecutively. The indication for TAB was either made by a referring physician or by a board approved ophthalmologist of our staff.
We excluded patients with an anterior ischemic optic neuropathy, a central retinal artery occlusion or diplopia. Other exclusion criteria were steroid therapy for longer than 10 days prior to TAB, an inconclusive histological assessment of the biopsy, and inability to comply with repeated Dynamic Contour Tonometry (DCT) measurements. The study design was approved by the local ethics committee.
Diagnostic parameters
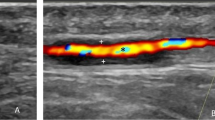
All patients were asked whether headache, scalp tenderness, jaw claudication, polymyalgia, or double vision were present. Thrombocyte counts, ESR and C—reactive protein values were also obtained. The OPA was measured by a slit lamp-mounted DCT device (PASCAL, Swiss Microtechnology AG, Port, Switzerland).14 All measurements were performed by the same two experienced ophthalmologists (PBK and CK) according to the manufacturer’s guidelines. Only readings with a quality index (‘Q’) of 1 or 2 (range: 1–5, with higher numbers indicating lower measurement quality) were considered for analysis. This was accomplished by setting the quality threshold on the device to ‘2’. For this study, the average of three consecutive readings was calculated and is referred to as the ‘OPA’ value of a given eye. Both eyes were examined but only values from the side were the biopsy was taken were used for analyses.
Reference test
In order to increase the chance of a positive biopsy, the side of the TAB (right or left temple) was chosen according to the side on which the clinical symptoms or signs were more pronounced. A specimen >1.3 cm of length before formalin fixation was harvested.15 Biopsies were regarded positive if they exhibited signs of necrotizing arteritis, characterized by a predominance of mononuclear cell infiltrates or a granulomatous process with multinucleated giant cells.3
Identifying candidate parameters for the score
Univariate analyses were performed with each of the diagnostic parameters mentioned above. Three parameters with a strong association (P≤0.05) with the presence of GCA were selected for further evaluation. (Thrombocyte counts (continuous variate; P=0.013), ESR (continuous variate; P=0.010) and OPA (continuous variate; P=0.050)).
Developing the score
The three parameters were categorized into three groups and a score value was attributed to each category as follows: OPA values >3.5 mm Hg got a score value of 0, values between 2.5 and 3.5 mm Hg got a score value of 1, and values <2.5 mm Hg were attributed a score value of 2. For ESR, values <25 mm/h obtained a score value of 0, values between 25–60 mm/h a score value of 1, and values >60 mm/h a score value of 2. For thrombocytes, the categories and corresponding values were <250'000/μl (score value 0), 250'000–500'000/μl (score value 1) and >500'000/μl (score value 2). The sum score could therefore reach values between 0 and 6 points and was calculated for each patient. A univariate logistic regression model with GCA presence as the dependent variate and the sum score as the independent variate (continuous scale) was used to estimate score-value specific probabilities of GCA presence using the following formula: P=probability of GCA=e(α+βscore)/1+ e(α+βscore), were α=intercept, β=regression coefficient for score variate.
The corresponding estimated probabilities are shown in Table 1. The area under the receiver operator curve (aROC) was estimated. Analyses were performed using the Stata 11.2 statistics software package (StataCorp LP, College Station, TX, USA).
Results
During the eighteen-month observation period 42 patients with presumed GCA presented at our department. Eleven of the 42 patients suspected of having GCA were excluded from the study because of steroid therapy for longer than 10 days prior to TAB (n=2), lack of the patient’s consent to TAB (n=1) or to the study (n=4), inability to comply with repeated IOP measurements (n=2), or due to a non-conclusive histological assessment of the biopsy (n=2).
Of the included 31 patients, 22 were female and 9 were male. Median age was 73 years (interquartile range 68–80 years). Biopsy results were positive for GCA in 20 patients (65%) and negative in 11 patients (35%). Further details are available in Table 2.
Score performance
The aROC was 0.90 (95% CI; 0.81–0.99) to predict a positive TAB result in our cohort. Four patients had scores ≤2, for fourteen patients the score was 3 or 4, and thirteen patients had a score of ≥5. The corresponding estimated probabilities of GCA presence were <7, 52.6 and >95%. The observed probabilities were 0.0% (0/4), 50.0% (7/14), and 100% (13/13), see Table 3 and Figure 1. Under the premise that a GCA probability of less than 7 percent is low enough to rule-out GCA and a probability of 95 percent is high enough to rule-in GCA, the number of correctly predicted TAB results would be 55% (17/31). Excluding the OPA information from the scoring system significantly decreased the percentage of correctly predicted TAB to 23% (7/31) (exact Mc Memar Test: P=0.02).
Relationship between score values and estimated probability of giant cell arteritis presence. The x-axis shows the sum score values and the y-axis shows the estimated probabilities from the regression model. The boxes indicate the threshold zones of rule-out (<7%) and rule-in (>95%) along with the corresponding score values. Reading example: A sum score value of 2 results in a probability of 7%.
Discussion
Our data document a strong association of reduced OPA levels with the presence of histologically proven GCA. This finding is consistent with previously published knowledge according to which the OPA represents pulsatile ocular blood flow and is reduced in the event of vascular obstruction.10, 11, 12, 13 OPA values have a dynamic diurnal rhythm that depends on intraocular pressure (discussed in16) Typically, reduced OPA values are measured in Grave’s disease, carotid artery stenosis or encircling buckles for retinal detachment which can easily be differentiated from GCA by history and routine ophthalmic examination.17, 18, 19 As measuring the OPA by DCT is a safe, fast and readily available procedure, integration into the diagnostic work-up is unproblematic in most cases.20, 21
Interestingly, in a population-based study on a series of biopsy-proven GCA, only 1 (0.4%) out of 240 patients had an ESR lower than 40 mm/1st hour, and the median ESR value was 93 mm/1st hour.22 Also, in that series, 17 (48.8%) of the 240 biopsy-proven GCA patients had platelet counts higher than greater than 400 000/mm3. This study also confirmed a strong correlation among most laboratory markers of inflammation at the time of disease diagnosis in GCA.22 Moreover, it emphasized the negative association between some laboratory parameters of inflammation, in particular the presence of anemia, and the development of severe ischemic complications in GCA.22 The present set of data also confirms the clinical lore of an association between elevated ESR and GCA. In addition, it corroborates the hypothesis that an elevated thrombocyte count is a useful marker of a positive TAB.6, 23 On the other hand, our data do not show a strong association between GCA and jaw claudication or diplopia, although a meta-analysis on 2680 patients suggests the contrary.7 This contradiction is acceptable as jaw claudication only just missed the pre-defined significance level by the smallest possible spread. On the other hand, a possible association might have been missed due to the limited number of patients. In our set of patients, the algorithm correctly predicts just over half of the TAB results if a rule-out threshold of less than 7% and a rule-in threshold of more than 95% are applied. If using a prediction model with clinical parameters only (i.e. age, female gender, headache, jaw claudication and scalp tenderness) the proportion of correctly classified patients would only have been 9/31 (29%). (Analysis not shown)
There are some noteworthy limitations of this study that need to be addressed in future research. First, it would be imprudent to implement the presented algorithm without extensive validation. Second, all parameters in the present algorithm were given equal weight. Future studies on larger numbers of patients might refine the algorithm by adjusting the effect an individual parameter exerts on the sum score. Third, the likelihood of the algorithm to correctly mirror the TAB results varies with the magnitude of the sum score. The algorithm is most efficient at the upper and lower end of the score range whereas sum scores in the mid-range (3 or 4) are clinically more difficult to interpret (Figure 1).
In conclusion, the present study confirms the association of reduced OPA levels in GCA. Furthermore, our results support the idea that an algorithm based on OPA, ESR and thrombocyte count has the potential to provide valuable assistance in the clinical management of GCA.

References
Aiello PD, Trautmann JC, McPhee TJ, Kunselman AR, Hunder GG . Visual prognosis in giant cell arteritis. Ophthalmology 1993; 100 (4): 550–555.
Landau K, Savino PJ, Gruber P . Diagnosing giant cell arteritis: is ultrasound enough? J Neuroophthalmol 2013; 33 (4): 394–400.
Hunder GG, Bloch DA, Michel BA, Stevens MB, Arend WP, Calabrese LH et al. The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum 1990; 33 (8): 1122–1128.
Murchison AP, Gilbert ME, Bilyk JR, Eagle RC Jr, Pueyo V, Sergott RC et al. Validity of the American College of Rheumatology criteria for the diagnosis of giant cell arteritis. Am J Ophthalmol 2012; 154 (4): 722–729.
Lenton J, Donnelly R, Nash JR . Does temporal artery biopsy influence the management of temporal arteritis? QJM 2006; 99 (1): 33–36.
Foroozan R, Danesh-Meyer H, Savino PJ, Gamble G, Mekari-Sabbagh ON, Sergott RC . Thrombocytosis in patients with biopsy-proven giant cell arteritis. Ophthalmology 2002; 109 (7): 1267–1271.
Smetana GW, Shmerling RH . Does this patient have temporal arteritis? JAMA 2002; 287 (1): 92–101.
Gonzalez-Gay MA, Garcia-Porrua C, Llorca J, Gonzalez-Louzao C, Rodriguez-Ledo P . Biopsy-negative giant cell arteritis: clinical spectrum and predictive factors for positive temporal artery biopsy. Semin Arthritis Rheum 2001; 30 (4): 249–256.
Kaufmann C, Bachmann LM, Robert YC, Thiel MA . Ocular pulse amplitude in healthy subjects as measured by dynamic contour tonometry. Arch Ophthalmol 2006; 124 (8): 1104–1108.
Horven I . Dynamic tonometry. IV. The corneal indentation pulse in giant cell arteritis. Acta Ophthalmol (Copenh) 1970; 48 (4): 710–718.
Horven I . Dynamic tonometry. V. Further studies of the corneal indentation pulse in temporal arteritis. Acta Ophthalmol (Copenh) 1973; 51 (3): 353–366.
Bienfang DC . Loss of the ocular pulse in the acute phase of temporal arteritis. Acta Ophthalmol Suppl 1989; 191: 35–37.
Bosley TM, Savino PJ, Sergott RC, Eagle RC, Sandy R, Gee W . Ocular pneumoplethysmography can help in the diagnosis of giant-cell arteritis. Arch Ophthalmol 1989; 107 (3): 379–381.
Bochmann F, Kaufmann C, Thiel MA . Dynamic contour tonometry versus Goldmann applanation tonometry: challenging the gold standard. Expert Rev Ophthalmol 2010; 5 (6): 743–749.
Taylor-Gjevre R, Vo M, Shukla D, Resch L . Temporal artery biopsy for giant cell arteritis. J Rheumatol 2005; 32 (7): 1279–1282.
Kim YJ, Lee KS, Lee JR, Na JH, Choi J, Han S et al. Ocular pulse amplitude as a dynamic parameter and its relationship with 24-h intraocular pressure and blood pressure in glaucoma. Exp Eye Res 2013; 115: 65–72.
Tsai CC, Kau HC, Kao SC, Lin MW, Hsu WM, Liu JH et al. Pulsatile ocular blood flow in patients with Graves' ophthalmopathy. Eye (Lond) 2005; 19 (2): 159–162.
Knecht PB, Menghini M, Bachmann LM, Baumgartner RW, Landau K . The ocular pulse amplitude as a noninvasive parameter for carotid artery stenosis screening: a test accuracy study. Ophthalmology 2012; 119 (6): 1244–1249.
Lincoff H, Stopa M, Kreissig I, Madjarov B, Sarup V, Saxena S et al. Cutting the encircling band. Retina 2006; 26 (6): 650–654.
Kaufmann C, Bachmann LM, Thiel MA . Comparison of dynamic contour tonometry with goldmann applanation tonometry. Invest Ophthalmol Vis Sci 2004; 45 (9): 3118–3121.
Punjabi OS, Kniestedt C, Stamper RL, Lin SC . Dynamic contour tonometry: principle and use. Clin Experiment Ophthalmol 2006; 34 (9): 837–840.
Gonzalez-Gay MA, Lopez-Diaz MJ, Barros S, Garcia-Porrua C, Sanchez-Andrade A, Paz-Carreira J et al. Giant cell arteritis: laboratory tests at the time of diagnosis in a series of 240 patients. Medicine (Baltimore) 2005; 84 (5): 277–290.
Lincoff NS, Erlich PD, Brass LS . Thrombocytosis in temporal arteritis rising platelet counts: a red flag for giant cell arteritis. J Neuroophthalmol 2000; 20 (2): 67–72.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Knecht, P., Bachmann, L., Thiel, M. et al. Ocular pulse amplitude as a diagnostic adjunct in giant cell arteritis. Eye 29, 860–866 (2015). https://doi.org/10.1038/eye.2015.85
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2015.85
This article is cited by
-
Neurologic manifestations of giant cell arteritis
Journal of Neurology (2022)
-
Evaluation of ocular pulse amplitude in non-arteritic anterior ischaemic optic neuropathy
BMC Ophthalmology (2017)