Abstract
Purpose
To report the occurrence of a novel mechanism of IOFB with hot, liquefied glass injury.
Methods
Retrospective case series.
Results
Two patients suffered an injury to their eye with hot, liquefied glass. The ocular findings included a single scleral entry wound with multiple glass fragments located inside the eye. Fragments were found embedded in the retina, as well as mobile on the retinal surface.
Conclusions
This distinctive mechanism involves an initial liquid state of glass causing injury, and results in multiple solidified glass IOFBs despite a single entrance wound. Though intraocular glass is typically inert, the unique characteristics of this injury may warrant a surgical approach. Surgical management proved successful in stabilizing vision and preventing further complications.
Similar content being viewed by others
Introduction
Glass IOFBs comprise 6–9% of all IOFB injuries.1 Despite the inert nature of glass, and the lack of significant ocular tissue reaction to its presence within the eye, glass IOFBs are typically surgically removed. Removal presents significant challenges to the surgeon: the size of the glass IOFB is typically larger than the entrance wound; the irregular shape of the glass IOFB often makes it difficult to grasp with forceps as well as remove; the sharpness of the edges of the glass IOFB can cause lens and retinal damage; and slippage of the glass IOFB within the eye can create further ocular injury.2
In this review, we present two unique cases of glass IOFB injuries incurred at a glass bangle factory in India. Presentation and management are described to highlight a novel mechanism of injury. This distinctive mechanism involves an initial liquid state of glass causing injury, and results in multiple solidified glass IOFBs despite a single entrance wound.
Case reports
Case 1
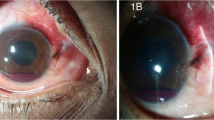
A 35-year-old male worker in a glass bangle factory sustained an injury when hot, liquid glass splashed into his right eye. On presentation to an ophthalmologist 2 days later, best-corrected visual acuity (BCVA) was 20/60 in the affected eye. Intraocular pressure was low. The examination revealed a single entrance wound in the supero-temporal sclera. There was no inflammatory reaction, however, the patient had developed a traumatic cataract. Dilated fundoscopic examination revealed 51 fragments of red glass. Some pieces were embedded in the retina with surrounding chorioretinal oedema, haemorrhage, and a flap retinal tear, while others were mobile and resting on the retinal surface (Figure 1a).
Case 2
A 30-year-old male worker in a glass bangle factory sustained a similar injury when hot, liquid glass splashed into his left eye. He presented 20 days later to an ophthalmologist with BCVA of 20/30 in the affected eye. Intraocular pressure was within normal limits and symmetrical. There was no inflammatory reaction. Dilated fundoscopic examination showed 11 fragments of green glass. Again, some pieces were embedded in the retina with surrounding chorioretinal oedema and haemorrhage. Other pieces were mobile and located on the retinal surface (Figure 2).
In both cases, the patients were not wearing protective glasses. The patients underwent surgical management to remove the IOFBs. A 20-gauge pars plana vitrectomy (PPV) with removal of IOFB, scleral buckle, endolaser, and silicone oil (SO) injection was performed in each patient (Figures 2b and c). The patient in the first case also underwent pars plana lensectomy (Figure 1c).
Follow-up was maintained for 4 years. The patient in case 1 developed an epiretinal membrane with macular pucker. He underwent a 20-gauge PPV with membrane stripping and SO removal at 4 months, with a resulting BCVA of 20/100 with an aphakic contact lens. The patient in case 2 developed cataract and underwent phacoemulsification and SO removal at 5 months, with BCVA stabilizing at 20/60.
Discussion
Glass IOFBs pose a specific challenge to the ophthalmologist, as there are pros and cons to surgical management. Glass is typically inert, and therefore will cause virtually no long-term inflammatory damage if retained. A retrospective study by Gopal et al3 showed no adverse events in eight of eight eyes where glass IOFBs were left intact. In the same study, 13/43 eyes that underwent surgical removal of the glass IOFBs experienced iatrogenic retinal breaks. Another review by Milkowski et al4 also revealed no complications with glass IOFBs left intact, even with close proximity to the optic nerve and retina.
On the other hand, complex cases with multiple glass IOFBs may yield different outcomes if not surgically removed. Mechanical complications from retained glass IOFBs can develop. Sharp edges, when moving posterior to anterior, have been reported to cause cataract, corneal oedema, and iridocyclitis.4 In addition, anterior to posterior migration can cause retinal laceration as well as trauma to the macula and subsequent visual impairment.2 As described above, liquified glass appears to solidify into many sharp glass fragments upon penetration through the scleral wall and cooling. The mechanism of glass fragmentation is unknown, but may be related to a splatter effect from the point of impact and upon entry into the eye. The numerous glass fragments resulting from these injuries heighten the risk of any potential complications.
Though protective eyewear may decrease the occurrence of such injuries, optimal management when they do occur is debatable. Based on this series, surgical management of similar cases can result in good, sustainable outcomes.

References
Ghoraba H . Posterior segment glass intraocular foreign bodies following car accident or explosion. Graefe’s Arch Clin Exp Ophthalmol 2002; 240: 524–528.
Ray S, Friberg T, Beatty R, Loewenstein J . Late posterior migration of glass intraocular foreign bodies. Arch Ophthalmol 2004; 122: 923–926.
Gopal L, Banker AS, Deb N, Badrinath SS, Sharma T, Parikh SN et al. Management of glass intraocular foreign bodies. Retina 1998; 18 (3): 213–220.
Milkowski S . Rare case of spontaneous migration of intraocular glass foreign body 21 years after injury. Wiad Lek 1978; 31 (15): 1065–1069.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ittiara, S., Sanduja, N., Chiranand, P. et al. Hot, liquid glass injury as a novel mechanism for intraocular foreign body. Eye 26, 1145–1149 (2012). https://doi.org/10.1038/eye.2012.140
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2012.140