Abstract
Aim
To report the clinical settings and factors predicting outcomes in scleral tears with concurrent retained intraocular foreign bodies
Methods
All cases with scleral and corneoscleral wounds with retained intraocular foreign bodies (RIOFB) from January 2014 to January 2021 were retrospectively analysed. Favourable anatomic outcome was defined as presence of globe integrity, attached retina, absence of hypotony and active inflammation at last visit. Favourable functional outcome was defined as final visual acuity (VA) > 20/200.
Results
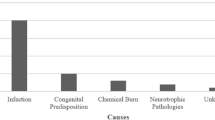
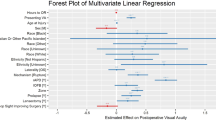
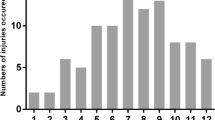
Total 139 eyes were included. Mean age was 30.66 ± 13.32 years (median 29 years, IQR 17). Penetrating trauma accounted for 87.1%, rupture for 5.8%, perforation for 7.2%. In 5.8% of the eyes the injury involved zone I extending till Zone II while in 66.9% it involved Zone II and in 27.3% in Zone III. Snellen visual acuity at presentation was logMAR 2.97 ± 1.01 and at last visit was logMAR 2.38 ± 1.45 (p < 0.0001). Time between presentation and repair was 13.93 ± 19.56 h (median 7.6 h, IQR 17.17). Favourable functional outcome was seen in 34.5% eyes and 2/3rd achieved favourable anatomic outcome. Absence of endophthalmitis (OR = 6.25, p = 0.003) and ability to remove the foreign body (OR = 7.05, p = 0.003) were associated with a favourable anatomic outcome. Better presenting Snellen visual acuity (OR = 2.77, p = 0.003), manifest scleral tear (OR = 3.36, p = 0.04), and absence of endophthalmitis (OR = 50, p = 0.0009) were associated with a favourable functional outcome.
Conclusion
A third of the cases achieved favourable visual outcome while 2/3rd achieved favourable anatomic outcome. Absence of endophthalmitis is an important factor predicting both.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
$259.00 per year
only $14.39 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
All data from the study have been quoted in the results section of the manuscript.
References
Kuhn F, Morris R, Witherspoon CD, Heimann K, Jeffers JB, Treister G. A standardized classification of ocular trauma. Ophthalmology. 1996;103:240–3.
Loporchio D, Mukkamala L, Gorukanti K, Zarbin M, Langer P, Bhagat N. Intraocular foreign bodies: A review. Surv Ophthalmol. 2016;61:582–96.
Vingopoulos F, Wang Y, Grob S, Li CYL, Eliott D, Kim LA, et al. Open Globe Injury with Intraocular Foreign Body. J Vitreoretin Dis. 2021;5:288–94.
Greven CM, Engelbrecht NE, Slusher MM, Nagy SS. Intraocular foreign bodies: management, prognostic factors, and visual outcomes. Ophthalmology. 2000;107:608–12.
Rozon JP, Lavertu G, Hébert M, You E, Bourgault S, Caissie M, et al. Clinical Characteristics and Prognostic Factors of Posterior Segment Intraocular Foreign Body: Canadian Experience from a Tertiary University Hospital in Quebec. J Ophthalmol. 2021;2021:9990290.
Liu Y, Wang S, Li Y, Gong Q, Su G, Zhao J. Intraocular Foreign Bodies: Clinical Characteristics and Prognostic Factors Influencing Visual Outcome and Globe Survival in 373 Eyes. J Ophthalmol. 2019;2019:5208092.
Mukkamala LK, Soni N, Zarbin MA, Langer PD, Bhagat N. Posterior Segment Intraocular Foreign Bodies: A 10-Year Review. Ophthalmol Retin. 2017;1:272–7.
Liang Y, Liang S, Liu X, Liu D, Duan J. Intraocular Foreign Bodies: Clinical Characteristics and Factors Affecting Visual Outcome. J Ophthalmol. 2021;2021:9933403.
Al-Omran AM, Abboud EB, Abu El-Asrar AM. Microbiologic spectrum and visual outcome of posttraumatic endophthalmitis. Retin Philos Pa. 2007;27:236–42.
Kuhn F, Maisiak R, Mann L, Mester V, Morris R, Witherspoon CD. The Ocular Trauma Score (OTS). Ophthalmol Clin N. Am. 2002;15:163–5.
Yaşa D, Erdem ZG, Demircan A, Demir G, Alkın Z. Prognostic value of ocular trauma score for open globe injuries associated with metallic intraocular foreign bodies. BMC Ophthalmol. 2018;18:194.
Brown IA. Intraocular foreign bodies. Nature of injury. Int Ophthalmol Clin. 1968;8:147–52.
Kuhn F, Pieramici DJ. Ocular Trauma - Principles and Practice. 1st ed. New York: Thieme; 2002.
Yeh S, Ralle M, Phan IT, Francis PJ, Rosenbaum JT, Flaxel CJ. Occult intraocular foreign body masquerading as panuveitis: inductively coupled mass spectrometry and electrophysiologic analysis. J Ophthalmic Inflamm Infect. 2011;2:99–103.
Kuhn F, Morris R, Witherspoon CD. Birmingham Eye Trauma Terminology (BETT): terminology and classification of mechanical eye injuries. Ophthalmol Clin North Am. 2002;15:139–43.
Pieramici DJ, Sternberg P, Aaberg TM, Bridges WZ, Capone A, Cardillo JA, et al. A system for classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification Group. Am J Ophthalmol. 1997;123:820–31.
Vashist P, Senjam SS, Gupta V, Gupta N, Kumar A. Definition of blindness under National Programme for Control of Blindness: Do we need to revise it? Indian J Ophthalmol. 2017;65:92–96.
GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the Global Burden of Disease Study. Lancet. Glob Health. 2021;9:e130–143.
Relhan N, Jalali S, Nalamada S, Dave V, Mathai A. Traumatic endophthalmitis presenting as isolated retinal vasculitis and white-centered hemorrhages: Case report and review of literature. Indian J Ophthalmol. 2012;60:317–9.
Jonas JB, Knorr HL, Budde WM. Prognostic factors in ocular injuries caused by intraocular or retrobulbar foreign bodies. Ophthalmology. 2000;107:823–8.
Mayer CS, Reznicek L, Baur ID, Khoramnia R. Open Globe Injuries: Classifications and Prognostic Factors for Functional Outcome. Diagnostics. 2021;11:1851.
Valmaggia C, Baty F, Lang C, Helbig H. Ocular injuries with a metallic foreign body in the posterior segment as a result of hammering: The Visual Outcome and Prognostic Factors. Retina. 2014;34:1116–22.
Chronopoulos A, Ong JM, Thumann G, Schutz JS. Occult globe rupture: diagnostic and treatment challenge. Surv Ophthalmol. 2018;63:694–9.
Jung HC, Lee SY, Yoon CK, Park UC, Heo JW, Lee EK. Intraocular Foreign Body: Diagnostic Protocols and Treatment Strategies in Ocular Trauma Patients. J Clin Med. 2021;10:1861.
Ma J, Wang Y, Zhang L, Chen M, Ai J, Fang X. Clinical characteristics and prognostic factors of posterior segment intraocular foreign body in a tertiary hospital. BMC Ophthalmol. 2019;19:17.
Keil JM, Zhao PY, Durrani AF, Azzouz L, Huvard MJ, Dedania VS, et al. Endophthalmitis, Visual Outcomes, and Management Strategies in Eyes with Intraocular Foreign Bodies. Clin Ophthalmol Auckl NZ. 2022;16:1401–11.
Williams DF, Mieler WF, Abrams GW, Lewis H. Results and prognostic factors in penetrating ocular injuries with retained intraocular foreign bodies. Ophthalmology. 1988;95:911–6.
Lieb DF, Scott IU, Flynn HW, Miller D, Feuer WJ. Open globe injuries with positive intraocular cultures: factors influencing final visual acuity outcomes. Ophthalmology. 2003;110:1560–6.
Ozturk T, Cetin Dora G, Ayhan Z, Kaya M, Arikan G, Yaman A. Etiology and Visual Prognosis in Open Globe Injuries: Results of A Tertiary Referral Center in Turkey. Sci Rep. 2019;9:17977.
Yeh S, Colyer MH, Weichel ED. Current trends in the management of intraocular foreign bodies. Curr Opin Ophthalmol. 2008;19:225–33.
He Y, Zhang L, Wang F, Zhu M, Wang Y, Liu Y. Timing influence on outcomes of vitrectomy for open-globe injury: A Prospective Randomized Comparative Study. Retin Philos Pa. 2020;40:725–34.
Colyer MH, Weber ED, Weichel ED, Dick JSB, Bower KS, Ward TP, et al. Delayed intraocular foreign body removal without endophthalmitis during Operations Iraqi Freedom and Enduring Freedom. Ophthalmology. 2007;114:1439–47.
Thach AB, Ward TP, Dick JS 2nd, Bauman WC, Madigan WP Jr, Goff MJ, et al. Intraocular foreign body injuries during Operation Iraqi Freedom. Ophthalmology. 2005;112:1829–33.
Funding
Hyderabad Eye Research Foundation.
Author information
Authors and Affiliations
Contributions
VPD conceived the idea of the manuscript, VPD, AVD and SRR collected and analysed the data, VPD, SRR, AVD and RA drafted and finalized the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ramamurthy, S.R., Das, A.V., Agrawal, R. et al. Management of scleral tears with concurrent intraocular foreign bodies and factors affecting outcomes. Eye 38, 297–302 (2024). https://doi.org/10.1038/s41433-023-02679-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-023-02679-6