Abstract
Background/objective:
To assess the relationship between maternal stress and distress in pregnancy and 5–8 years postpartum and child nutritional status.
Subjects/methods:
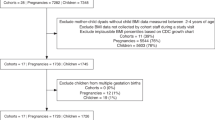
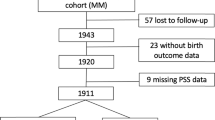
Longitudinal cohort study carried out in Jundiai city, Southeast Brazil, involving 409 women followed throughout pregnancy to 5–8 years postpartum, and respective children. Measures of stress and distress were obtained three times in pregnancy (at gestational ages lower than 16 weeks, from 20 to 26 weeks and from 30 to 36 weeks) and 5–8 years postpartum by the Perceived Stress Scale (PSS), General Health Questionnaire (GHQ) and the State-Trait Anxiety Inventories (STAI). The nutritional status of the children was assessed by the World Health Organization body mass index (BMI) z-score for age. The relationship between child BMI z-score for age and scores of the PSS, GHQ and STAI was evaluated by multivariate linear regression, controlling for confounding variables.
Results:
BMI z-score for age of the children was negatively associated with maternal scores of the PSS 5–8 years postpartum and scores of the GHQ in the second trimester of pregnancy. BMI of the children was positively associated with maternal BMI and birthweight (R2=0.13). There was −0.04 (confidence interval −0.07 to −0.9 × 10−2) decrease in child BMI per score unit of the PSS increase, and −0.09 (confidence interval −0.18 to −0.6 × 10−3) decrease in child BMI per score unit of the GHQ increase.
Conclusions:
This study detected a relationship between maternal mental and nutritional status and child nutritional status, implying that if the mother is not physically or mentally well, her capacity for caring for her child may be impaired.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
World Health Organization-WHO. The Global Burden of Disease. WHO: Geneva, Switzerland, 2008.
Hoffman S, Hatch C . Stress, social support and pregnancy outcome: a reassessment based on recent research. Paediatr Perinat Epidemiol 1996; 10: 380–405.
Marcus SM . Depression during pregnancy: rates, risks and consequences. Can J Clin Pharmacol 2009; 16: e15–e22.
Brummelte S, Galea LAM . Depression during pregnancy and postpartum: Contribution of stress and ovarian hormones. Prog Neuropsychopharmacol Biol Psychiatry 2010; 34: 766–776.
Benner A, Gerber LM, Sheikh J . Prevalence of psychiatric disorders and associated risk factors in women during their postpartum period: a major public health problem and global comparison. Int J Womens Health 2012; 4: 191–200.
Parker KJ, Schatzberg AF, Lyons DM . Neuroendocrine aspects of hypercortisolism in major depression. Horm Behav 2003; 43: 60–66.
Austin MP, Hadzi-Pavlovic D, Priest SR, Reilly N, Wilhelm K, Saint K et al. Depressive and anxiety disorders in the postpartum period: how prevalent are they and can we improve their detection? Arch Womens Ment Health 2010; 13: 395–401.
Surkan PJ, Kawachi I, Peterson KE . Childhood overweight and maternal depressive symptoms. J Epidemiol Community Health 2008; 62: e11.
Santos DS, Santos DN, Silva RCR, Hasselmann MH, Barreto L . Maternal mental common disorders and malnutrition in children: a case-control study. Soc Psychiatry Psychiatr Epidemiol 2011; 46: 543–548.
Grote NK, Bridge JA, Gavin AR, Melville IL, Iyengar S, Katon WJ . A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry 2010; 67: 1012–1024.
Gundersen C, Lohman BJ, Garasky S, Stewart S, Eisenmann J . Food security, maternal stressors, and overweight among low income US children: results from the National Health and Nutrition Examination Survey (1999–2002). Pediatrics 2008; 122: e529–e540.
Ajslev TA, Andersen CS, Ingstrup KG, Nohr EA, Sorensen TIA . Maternal postpartum distress and childhood overweight. PloS ONE 2010; 5: e11136.
Avan B, Richter LM, Ramchandani PG, Norris SA, Stein A . Maternal postnatal depression and children's growth and behaviour during the early years of life: exploring the interaction between physical and mental health. Arch Dis Child 2010; 95: 690–695.
Duarte CS, Shen S, Wu P, Must A . Maternal depression and child BMI: longitudinal findings from a US sample. Pediatr Obes 2012; 2: 124–133.
Rondó PHC, Ferreira RF, Nogueira F, Ribeiro MCN, Lobert H, Artes R . Maternal psychological stress and distress as predictors of low birth weight, prematurity and intrauterine growth retardation. Eur J Clin Nutr 2003; 57: 266–272.
Cohen S, Kamarck T, Mermelstein R . A global measure of perceived stress. J Health Soc Behav 1983; 24: 385–396.
Goldberg DP The Detection of Psychiatric Illness by Questionnaire. Oxford University Press: London, UK, 1972.
Mari JJ, Williams P . A comparison of the validity of two psychiatric screening questionnaires (GHQ-12 and SRQ-20) in Brazil, using relative operating characteristic (ROC) analysis. Psychol Med 1985; 15: 651–659.
Spielberger CD, Gorsuch RI, Lushene RE STAI Manual for the State - Trait Anxiety Inventory. Consulting Psychologist Press: Palo Alto, CA, USA, 1970.
Capurro H, Konishezky S, Fonseca D, Caldeyro-Barcia R . A simplified method for diagnosis of gestational age in the newborn infant. J Pediatr 1978; 93: 120–122.
World Health Organization- WHO. Consultation on Obesity. Obesity: preventing and managing the global epidemic. WHO: Geneva, Switzerland, 2000.
de Onis M, Onyango AW, Borghi E, Siyan A, Nishida C, Siekmann J . Development of a WHO growth reference for school-aged children and adolescents. Bull WHO 2007; 85: 660–667.
Jelliffe DB, Jelliffe EFP (eds). Community Nutritional Assessment, With Special Reference To Less Technically Developed Countries 2nd edn. Oxford University Press: London, UK, 1989.
Patel V, De Souza N, Rodrigues M . Post-natal depression and infant growth and development in low income countries: a cohort study from Goa, India. Arch Dis Child 2003; 88: 34–37.
Harpham T, Huttly S, De Silva M, Abramsky T . Maternal mental health and child nutritional status in four developing countries. J Epidemiol Community Health 2005; 59: 1060–1064.
Rahman A, Iqbal Z, Bunn J, Lovel H, Harrington R . Impact of maternal depression on infant nutritional status and illness: a cohort study. Arch Gen Psychiatry 2004; 61: 946–952.
Stewart RC, Umar E, Kauye F, Bunn J, Vokhiwa M, Fitzgerald M . Maternal common mental disorder and infant growth - a cross-sectional study from Malawi. Matern Child Nutr 2008; 4: 209–219.
Surkan PJ, Kawachi I, Ryan LM, Berkman LF, Carvalho Vieira LM, Peterson KE . Maternal depressive symptoms, parenting self-efficacy, and child growth. Am J Public Health 2007; 97: 125–132.
Milgrom J, Skouteris H, Worotniuk T, Henwood A, Bruce L . The association between ante- and postnatal depressive symptoms and obesity in both mother and child: a systematic review of the literature. Womens Health Issues 2012; 3: e319–e328.
Ertel KA, Koenen KC, Rich-Edwards JW, Gillman MW . Antenatal and postpartum depressive symptoms are differentially associated with early childhood weight and adiposity. Paediatr Perinat Epidemiol 2010; 24: 179–189.
Taveras EM, Gillman MW, Kleinman K, Rich-Edwards JW, Rifas-Shiman SL . Racial/ethnic differences in early-life risk factors for childhood obesity. Pediatrics 2010; 125: 686–695.
Stewart RC . Maternal depression and infant growth: a review of recent evidence. Matern Child Nutr 2007; 3: 94–107.
Tomlinson M, Cooper PJ, Stein A, Swartz L, Molteno C . Post-partum depression and infant growth in a South African peri-urban settlement. Child Care Health Dev 2006; 32: 81–86.
Patel V, Prince M . Maternal psychological morbidity and low birth weight in India. Br J Psychiatry 2006; 188: 284–285.
Amorim RJM, Lima MC, Lira PIC, Emond AM . Does low birthweight influence the nutritional status of children at school age? A cohort study in northeast Brazil. Matern Child Nutr 2011; 7: 295–306.
Bjeland M, Lien N, Bergh IH, Grydeland M, Anderssen SA, Klepp K-I et al. Overweight and waist circumference among Norwegian 11-year-olds and associations with reported parental overweight and waist circumference: The HEIA study. Scand J Public Health 2010; 38: 19–27.
Mc Donald CM, Baylin A, Arsenault JE, Mora-Plazas M, Vilamor E . Overweight is more prevalent than stunting and is associated with socioeconomic status, maternal obesity, and a snacking dietary pattern in school children from Bogotá, Colombia. J Nutr 2009; 139: 370–376.
Rosengranz RR, Bauer A, Dzewaltowski DA . Mother-daughter resemblance in BMI and obesity-related behaviors. Int J Adolesc Med Health 2010; 22: 477–489.
Lourenço BH, Villamor E, Augusto RA, Cardoso MA . Influence of early life factors on body mass index trajectory during childhood: a population-based longitudinal analysis in the Western Brazilian Amazon. Matern Child Nutr 2012, e-pub ahead of print 1 October 2012 doi:10.1111/mcn.12005.
Paffer AT, Ferreira HS, Cabral Junior CR, Miranda CT . Prevalence of common mental disorders in mothers in the semiarid region of Alagoas and its relationship with nutritional status. Sao Paulo Med J 2012; 130: 84–91.
Patel V, Rodrigues M, DeSouza N . Gender, poverty, and post-natal depression: a study of mothers in Goa, India. Am J Psychiatry 2002; 159: 43–47.
Rondó PHC, Souza MR . Maternal distress and intended breastfeeding duration. J Psychosom Obstet Gynecol 2007; 28: 55–60.
Engle PL . Maternal mental health, program and policy implications. Am J Clin Nutr 2009; 89: 963S–966S.
Patel V, Chowdhary N, Rahman A, Verdeli H . Improving access to psychological treatments: lessons from developing countries. Behav Res Ther 2011; 49: 523–528.
Acknowledgements
We thank Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP), São Paulo, Brazil, for financing this study (grants: 1998/00321-0; 2004/04109-8), and the field workers Rosemary F Ferreira, Alessandra L Santos and Josimara F Moura.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Authors contributions
PHCR designed the study protocol, secured funding, and participated in the statistical analysis, interpretation of data and writing of the paper. GR participated in the statistical analysis and interpretation of data. JOL and JAP collected data, and participated in the interpretation of data and writing of the paper. All authors approved the final version of the paper.
Rights and permissions
About this article
Cite this article
Rondó, P., Rezende, G., Lemos, J. et al. Maternal stress and distress and child nutritional status. Eur J Clin Nutr 67, 348–352 (2013). https://doi.org/10.1038/ejcn.2013.28
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ejcn.2013.28
Keywords
This article is cited by
-
The relation between prenatal stress, overweight and obesity in children diagnosed according to BMI and percentage fat tissue
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity (2022)
-
The effect of nutrition and reproductive health education of pregnant women in Indonesia using quasi experimental study
BMC Pregnancy and Childbirth (2021)
-
Common mental disorders in mothers of children attending out-patient malnutrition clinics in rural North-western Nigeria: a cross-sectional study
BMC Public Health (2021)
-
Nutritional status and prey energy density govern reproductive success in a small cetacean
Scientific Reports (2021)
-
Home-based intervention for non-Hispanic black families finds no significant difference in infant size or growth: results from the Mothers & Others randomized controlled trial
BMC Pediatrics (2020)