
Credit: Stuart Bebb/Wolfson College Archives
Anthony (Tony) Epstein, co-discoverer of the Epstein–Barr virus (EBV), was the founding father of research into the part that viruses play in the development of human cancers. Today, seven types of viral infection — more than one of which can be prevented by vaccination — are known to cause specific cancers in people. Collectively, virus-associated tumours account for up to 15% of cancer cases globally each year. Yet, when Epstein began his research in the early 1960s, the concept of a link between viruses and human cancer was deeply unfashionable. Epstein’s discovery has had an enormous influence on the direction of cancer research, from underlying mechanisms to new prospects for prevention.
Epstein was born in London in 1921 and educated at St Paul’s School. He then attended Trinity College in Cambridge, UK, followed by medical training at Middlesex Hospital Medical School in London. After taking house-surgeon jobs in London and Cambridge, he served for two years in the Royal Army Medical Corps before specializing in pathology at the Bland Sutton Institute at the Middlesex Hospital. There, he developed his interest in tumour viruses and began researching the Rous sarcoma virus. Many years earlier, Peyton Rous at The Rockefeller University in New York City had shown that this virus causes cancer in chickens.
In 1956, Epstein spent a year at the Rockefeller, working in the laboratory of cell biologist George Palade, who pioneered the use of electron microscopy to study the structure of cells. That technique allowed Epstein to visualize viral infections in cells and was the key to his subsequent discovery of EBV.
How cancer hijacks the nervous system to grow and spread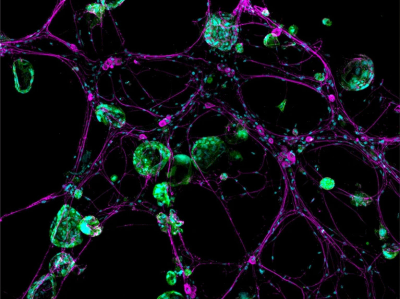
In 1961, Denis Burkitt, a little-known surgeon at Makerere College in Kampala, gave a talk at Middlesex Hospital entitled ‘The Commonest Children’s Cancer in Tropical Africa: A Hitherto Unrecognised Syndrome’. Intrigued by the title, Epstein attended and was transfixed. Burkitt described not only the tumour’s unusual anatomical presentation, typically in the jaw of young children, but also its geographical restriction to equatorial Africa. Epstein wondered whether a virus — possibly passed on by an insect bite, similar to the transmission of the malarial parasite — could be linked to the tumour.
Over the next two years, the pair collaborated closely. Burkitt sent fresh biopsies of the tumour (later named Burkitt lymphoma) in culture fluid by plane from Kampala to London for Epstein to analyse. Discouragingly, cell-culture assays to detect known viruses were consistently negative. Under the electron microscope, the cells showed no sign of infection. Fragments of the tumour failed to grow in culture.
After more than 20 attempts, in December 1963, a biopsy sample arrived late in the day, delayed by fog at London Heathrow airport. Unusually, the fluid was cloudy. This was not due to bacterial contamination, as feared, but to free-floating tumour cells. This tumour was the first to grow in culture, producing a cell line named EB1; E after Epstein, and B after his research assistant Yvonne Barr.
Within weeks, there were enough cells for analysis using an electron microscope. In the first image, one of the cells contained herpesvirus-like particles. Epstein sent EB1 cells to the virology laboratory at the Children’s Hospital in Philadelphia, Pennsylvania, where Werner and Gertrude Henle tested them using human sera with defined patterns of reactivity against known human herpesviruses. The pattern against EB1 cells was different, proving that the virus was unique. The Henles dubbed it the Epstein–Barr virus, after the cell line’s name.
Forget lung, breast or prostate cancer: why tumour naming needs to change
It took decades of work by Epstein’s lab and many others before EBV was unequivocally recognized as the first human tumour virus. The virus proved to be widespread in all populations, and Burkitt lymphoma’s paradoxical link to Africa was later explained: malarial infection promotes EBV’s causative role in this type of tumour. The Henles went on to show that EBV causes infectious mononucleosis (glandular fever), and the virus is now causally linked to at least six types of human tumour, together accounting for around 200,000 new cancer cases worldwide each year.
Not long after his discovery, Epstein moved to the University of Bristol, UK, where he was a professor of pathology, accompanied by pathologist Bert Achong, his colleague at Middlesex. There, he built what became a model multidisciplinary department, integrating basic research in virology, immunology and oncology with medical and veterinary pathology practice. He also established a ground-breaking undergraduate course in cellular pathology, with final-year research projects open to science, medical and veterinary students, a base from which many successful research careers were launched. All of this work was way ahead of its time.
Tony received many honours. Elected a fellow of the Royal Society in 1979, he served as the society’s foreign secretary for five years from 1986, and was knighted in 1991. However, those of us who worked closely with him remember not this rather formal public persona, but a colleague who was an engaging conversationalist, with a ready wit and command of language. Writing papers with him was an unforgettable experience! As both researcher and mentor, his greatest virtues were absolute clarity of thought and commitment to a long-term vision.
Nowhere was his foresight more evident than when, as early as the 1970s, he established an animal model of EBV-induced lymphomas in New World monkeys as a testbed for his long-term goal of EBV vaccine development. Remarkably, he lived long enough to see this vision become reality (at least two candidates are now in clinical trials), following a resurgence of interest in vaccinology in our post-COVID-19 world.

 Forget lung, breast or prostate cancer: why tumour naming needs to change
Forget lung, breast or prostate cancer: why tumour naming needs to change
 How cancer hijacks the nervous system to grow and spread
How cancer hijacks the nervous system to grow and spread
 Cervical cancer kills 300,000 people a year — here’s how to speed up its elimination
Cervical cancer kills 300,000 people a year — here’s how to speed up its elimination
 The future of precision cancer therapy might be to try everything
The future of precision cancer therapy might be to try everything
 Smoking scars the immune system for years after quitting
Smoking scars the immune system for years after quitting
 Harald zur Hausen, virologist who linked viruses to cancer (1936–2023)
Harald zur Hausen, virologist who linked viruses to cancer (1936–2023)







