Abstract
Waldenstrom macroglobulinemia (WM) is a B-cell lymphoplasmacytic lymphoma characterized by monoclonal immunoglobulin M protein in the serum and infiltration of bone marrow with lymphoplasmacytic cells. Asymptomatic patients can be observed without therapy. First-line therapy should consist of the monoclonal anti-CD20 antibody, rituximab, given typically in combination with other agents. We prefer dexamethasone, rituximab, cyclophosphamide (DRC) as initial therapy for most patients with symptomatic WM. Other reasonable options are bortezomib, rituximab, dexamethasone (BoRD) or bendamustine plus rituximab (BR). All of these regimens are associated with excellent response and tolerability. Initial therapy is usually administered for 6 months, followed by observation. Response to therapy is assessed using the standard response criteria developed by the International Working Group on Waldenstrom macroglobulinemia. Relapse is almost inevitable in WM but may occur years after initial therapy. In symptomatic patients relapsing more than 1–2 years after initial therapy, the original treatment can be repeated. For relapse occurring sooner, an alternative regimen is used. In select patients, high-dose chemotherapy followed by autologous hematopoietic cell transplantation may be an option at relapse. Options for therapy of relapsed WM besides regimens used in the front-line setting include ibrutinib, purine nucleoside analogs (cladribine, fludarabine), carfilzomib and immunomodulatory agents (thalidomide, lenalidomide).
Similar content being viewed by others
Introduction
Waldenstrom macroglobulinemia (WM) is defined as a B-cell lymphoplasmacytic lymphoma, characterized by monoclonal immunoglobulin M protein in the serum and infiltration of bone marrow with lymphoplasmacytic cells.1 A majority of patients with WM have a recurrent mutation of the MYD88 gene (MYD88 L265P).2, 3 The highest incidence of WM occurs among older individuals, with a median age at diagnosis in the 60s.1, 4 Although approximately 25% of patients are asymptomatic at the time of diagnosis, most patients present with symptoms attributable to tumor burden, including anemia, pancytopenia, organomegaly, neuropathy, amyloidosis, cryoglobulinemia, night sweats and symptomatic hyperviscosity.5, 6, 7 The focus of this paper is on the prognosis and treatment of WM.8, 9
Prognosis
WM is a fairly indolent, chronic disease in most patients. The median survival has varied in studies, from 5 years to nearly 11 years.10 The main causes of death because of WM include disease progression, transformation to high-grade lymphoma or complications of therapy. However, owing to the advanced age of these patients, many will die of unrelated causes.5 Mortality is linked to the development of symptoms; the mortality of asymptomatic patients is similar to that of the general population, whereas it is significantly higher in symptomatic patients.11, 12 No studies have demonstrated a survival benefit of treating asymptomatic patients, nor are there data to suggest delaying therapy until symptoms develop adversely affects response to treatment.1, 11, 13 Furthermore, following a surveillance approach can maintain the patient’s quality of life, and limit exposure to chemotherapy and its potential side effects.8 The decision between surveillance and treatment remains a clinical one; however, use of prognostic models may help guide the decision between more aggressive therapy vs avoidance of therapy-related complications and preservation of quality of life.1, 9
Several staging systems have been proposed to risk stratify patients with WM and to aid in prognosis (Table 1).10, 14, 15 Dhodapkar and colleagues14 developed a three-parameter staging system for WM based on the results of a multicenter clinical trial conducted by the Southwest Oncology Group. This model uses hemoglobin concentration, β2-microglobulin levels and serum immunoglobulin (Ig) M level to classify patients into four prognostic groups with significantly different 5-year survival rates. As the model was developed in the setting of a clinical trial, it is unclear how prognosis would differ for patients who are not candidates for clinical trials including patients with poor performance status. On the basis of another study of 337 symptomatic patients with WM, a prognostic model was created at the Mayo Clinic consisting of age >65 and presence of organomegaly.15 Having neither of these factors conferred a 10-year estimated survival rate of 57%. One factor was associated with 16% 10-year survival, and the presence of both factors was associated with 5% survival at 10 years. The addition of elevated β2-microglobulin ⩾4 mg/l was associated with a threefold increased risk of death. Of note, the prognostic significance of serum IgM levels and organomegaly has varied in different studies, whereas age is consistently a poor prognostic indicator.
Given the wide selection of new treatments available for WM, a standardized scoring system has been developed recently, known as the International prognostic scoring system for Waldenstrom macroglobulinemia (IPSSWM), to help guide treatment based on prognosis in symptomatic patients10 (Table 1). Using multivariate analysis, five variables were identified which were associated with adverse outcomes: age >65, hemoglobin ⩽11.5, platelet ⩽100 000/microliter, β2–microglobulin >3 mg/l and serum monoclonal protein concentration >70 g/l. The low-risk group is defined as having no more than one of these characteristics, excluding age >65, and is associated of an average 5-year survival of 87%. Intermediate risk patients have two of the above characteristics or age >65, and is associated with 5-year survival of 68% on average. Finally, the high-risk group has three or more adverse characteristics, with a 5-year survival of 36%.
On the basis of a prospective study of 72 patients, von Willebrand factor antigen level was identified as a prognostic factor in WM.16 High levels were associated with poor prognosis that did not improve with disease control. Low levels on the other hand were associated with increased bleeding risk but improved with lowering of serum IgM levels.
Treatment
WM is incurable with currently available therapies. Treatment is instead focused on symptom-control and prevention of end-organ damage.1, 8, 9 There is no standard therapy for WM, but rather various drugs that have been shown to be effective either alone or in combinations (Tables 2 and 3).17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27 Asymptomatic patients should be followed with surveillance, while symptomatic patients should be considered for treatment. The severity of symptoms dictates the intensity of the treatment regimen, however, several factors, such as age, cytopenias, need for quick disease control and potential candidacy for stem cell transplant, should be considered. Care should be given to avoid treatments that may compromise stem-cell collection in patients who are candidates for autologous hematopoietic cell transplantation (HCT).
Treatment of hyperviscosity
Hyperviscosity is a clinical emergency. Manifestations are the result of shear forces which cause venous damage, and include visual changes resulting from retinal flame-shaped hemorrhages, epistaxis, gingival bleeding, headaches and dizziness; more severe manifestations include stupor and coma. Hyperviscosity syndrome occurs when the serum viscosity is >4 (viscosity of water is 1), which corresponds to serum IgM of at least roughly 4000 mg/dl. Immediate management is the removal of IgM from systemic circulation, via plasmapheresis. Transfusion with red blood cells should be avoided prior to plasmapheresis to avoid increasing serum viscosity. Although there are no randomized trials on the use of plasmapheresis in managing hyperviscosity, total plasma exchange (roughly 3–4 l in an adult, replaced with albumin rather than plasma) is repeated daily until normal serum viscosity is achieved and symptoms are relieved. Plasmapheresis does not alter the disease course, therefore, after plasmapheresis is complete, chemotherapy should be initiated. This approach also helps avoid potential loss of drugs that may be bound to protein in the serum.
Single-agent therapy
Rituximab
As all WM cells express CD-20, it is generally agreed upon that first-line therapy should consist of monoclonal anti-CD20 antibody, rituximab, alone or preferably in combination. 9 As it may take several months to achieve the maximum response to rituximab, it is a poor choice as single-agent therapy in patients in whom a rapid response is needed, or in patients with IgM levels above 3 g/dl. However, in selected patients, it has been shown to reduce neurologic symptoms, improve cytopenias and bone marrow involvement, while still being fairly well tolerated without damaging stem cells.17, 28, 29, 30 Of note, there may be a paradoxical increase in monoclonal protein levels after starting rituximab therapy, termed the 'rituximab flare' which may persist for up to 4 months.8 This does not indicate treatment failure, but plasmapheresis may be necessary to avoid the development of hyperviscosity. A prospective trial randomized 69 patients with lymphoplasmacytic lymphoma, 48 of whom met criteria for WM, to receive rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone (CHOP) vs rituximab plus CHOP (R-CHOP).18 The R-CHOP group as a whole had significantly higher overall response rate as compared with the CHOP group, (94 vs 67%), as well as in the WM subgroup (91 vs 60%). R-CHOP was also associated with a significantly longer time to treatment failure (median 63 months vs 22 months) which also carried over to the WM subgroup. No major difference in treatment-associated toxicity was observed between the two groups. A phase II trial of single-agent rituximab in 69 patients with WM (34 untreated, 35 previously treated) was undertaken, which showed an objective response in 27.5% and minor response in 24.6% of patients.17 Single-agent rituximab is a reasonable treatment option for minimally symptomatic, low-risk patients with only moderate hematologic compromise (hemoglobin 10–11 g/dl or platelets 100 000–120 000/l), as well as patients with IgM-associated neuropathy, or hemolytic anemia which is refractory to corticosteroids.8 Rituximab plus additional agents is preferred for patients with severe cytopenias (hemoglobin <10 g/dl or platelets <100 000/l), constitutional symptoms or symptoms of hyperviscosity. Although the combination of rituximab plus another agent has been shown to attain a high response rate more rapidly, it is unclear whether it confers prolonged survival. In patients who are rituximab-naïve and respond to rituximab-containing regimens, maintenance rituximab has been shown to improve overall and progression-free survival, although it is also associated with higher rates of infection, and is generally not recommended.1, 8, 31
Bortezomib
The Waldenstrom Macroglobulinemia Clinical Trials Group (WMCTG) conducted a multicenter study investigating the use of bortezomib, a reversible proteasome inhibitor, in the management of WM.32 The results of this study showed an overall response rate of 85%, with median duration to response of only 1.4 months. The most common side effect was sensory neuropathy, which resolved or improved in almost all patients after cessation of therapy. Of note, discordance between serum IgM levels and bone marrow response has been observed in bortezomib therapy, necessitating bone marrow biopsy or computed tomography scans to monitor response to therapy.33
Alkylating agents
Of the alkylating agents, oral chlorambucil is the most commonly used agent, resulting in at least a partial response in >50% of patients.6 Therapy continues until symptoms resolve and serum IgM concentration plateaus. Alkylating agents have been associated with the development of secondary leukemias and myelodysplasia. Chlorambucil should be avoided in patients who are considered candidates for stem cell transplantation.
Combination therapy
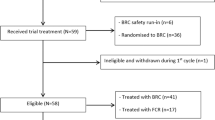
Multiple rituximab-containing regimens, which lack stem-cell toxicity, are available: dexamethasone, rituximab, cyclophosphamide (DRC); bortezomib, rituximab with or without dexamethasone; bendamustine with rituximab (BR). We prefer any of these three regimens for front-line therapy (Figure 1). The primary factors influencing selection among the available regimens are drug toxicities and individual patient characteristics. For example, in a patient with peripheral neuropathy, DRC may be preferred because of the high incidence of neuropathy associated with bortezomib. In patients with bulky disease, BR may be preferred for rapid control. The major studies supporting the use of these and other commonly used combinations in WM is presented below.
Dexamethasone, rituximab and cyclophosphamide (DRC)
In a phase-II trial of symptomatic, treatment-naïve patients with WM, DRC was associated with an 83% overall response rate and 7% complete response rate.21 Two-year overall survival was 81%, with progression-free survival of 67%. The toxicity profile was mild, mainly consisting of nausea, alopecia, neutropenia and mild infusion reactions to rituximab.
Bortezomib, rituximab and dexamethasone
In two separate phase-II trials of symptomatic, previously untreated patients with WM, BRD was associated with 85%34 and 96%20 overall response rates, respectively. However, in one of the studies, there was a 27% discontinuation rate because of drug toxicity.34 The most common toxicity reported was peripheral neuropathy, occurring in 46% of patients in the study by Dimopoulos and colleagues,34 and 69% in the study conducted by Treon and colleagues.20 In patients with myeloma, bortezomib neuropathy has been markedly abrogated by the use of weekly subcutaneous bortezomib rather than the twice weekly intravenous schedule.35, 36, 37 On the basis of these data, we recommend weekly subcutaneous bortezomib for patients with WM as well, similar to current recommendations in myeloma.38
Bendamustine plus rituximab
Bendamustine is a nitrogen mustard which bears structural similarities to alkylating agents as well as purine analogs. A phase II trial of BR in 63 patients (including 17 with WM/lymphoplasmacytic lymphoma) with relapsed/refractory low-grade or mantle cell lymphoma showed overall response rate of 90% and complete response rate of 60%.19 Median progression-free survival was 24 months. The most common side effect was leukopenia, with grade 3 and 4 severity occurring in 16%. Treon et al.39 studied the outcome of 30 patients with relapsed/refractory WM treated with BR. The overall response rate (very good partial response and partial response) was 83.3% including some patients who were intolerant to rituximab and received bendamustine alone. Treatment was generally well-tolerated although prolonged myelosuppression was noted in some of the patients who had previously received nucleoside analog therapy. A prospective study of previously untreated indolent Non-Hodgkin lymphoma/Mantle Cell lymphoma randomized patients to receive BR or R-CHOP.40 Among the 41 WM patients included in the study, both arms showed 95% response rates, with longer progression-free survival in the BR arm vs R-CHOP (69.5 months vs 28.1). There were also lower rates of adverse events observed in the BR arm vs R-CHOP.
Purine nucleoside analogs
Nucleoside analogs have significant activity in the treatment of WM. However, these agents should be avoided as initial therapy in patients who may be candidates for HCT as they are toxic to stem cells and may compromise the ability to harvest stem cells for transplant.
Fludarabine and cladribine are two purine nucleoside analogs, which have been found to be effective in WM, either alone or in combinations.41, 42, 43 The combination of purine nucleoside analogs with rituximab improves response rates with little added toxicity, and may be ideal especially when rapid disease control is needed.23, 44 A phase III trial comparing chlorambucil and fludarabine in treatment of >300 patients with WM showed improved progression-free survival and longer duration of response with fludarabine use.45 As a single agent, fludarabine is associated with > 50% survival at 8 years in patients with one risk factor, and >30% survival in those with two risk factors.14 Rituximab plus fludarabine has an overall response rate of >95%. Severe toxicities associated with fludarabine include neutropenia and thrombocytopenia, as well as a future predisposition to develop myelodysplasia and lymphomas/leukemias.23, 46 Alternatively, combination cladribine with rituximab was associated with similar overall response rates (90%), but was generally better-tolerated producing milder cytopenias.24 An Italian study of 43 patients with symptomatic WM treated with fludarabine/cyclophosphamide/rituximab showed an overall response rate of 79%.22 Severe neutropenia (grade 3–4) was seen in 88% of patients, but was prolonged in 44% of patients.
Other drugs
Alemtuzumab
Alemtuzumab is a monoclonal antibody against CD52, a glycoprotein found on WM lymphoplasmacytic cells as well as mast cells, and stimulates growth and survival of WM lymphoplasmacytic cells. WMCTG conducted a multicenter study using alemtuzumab to treat 27 patients with WM.47 Overall response rate was 75%, with cytopenias occurring commonly among patients who had been treated previously.
Lenalidomide
Immunomodulatory agents have been combined with monoclonal antibodies in an effort to improve disease response in WM while avoiding the side effects of chemotherapy. Two such agents are thalidomide, and lenalidomide, its more potent derivative. The combination of lenalidomide with rituximab was studied in 16 symptomatic patients with WM who were naïve to both agents and 12 of whom were previously untreated.48 The overall response rate was 50%, with a minor response rate of 25%, both inferior to a study of thalidomide/rituximab by the same authors.27 The median time to progression among the responders was 18.9 months. Anemia also developed in >80% of the study patients, despite dose reductions of lenalidomide, and resulted in premature discontinuation and cessation of further enrollment. Hematocrit levels improved after lenalidomide cessation in the 12 evaluable patients.
Thalidomide
A phase-II trial of thalidomide with rituximab in patients with symptomatic WM was undertaken in 35 patients who had not been treated with either drug previously.27 Results showed an overall response rate of 72%. Neuropathy was a major side effect, necessitating dose reductions in all patients in the trial.
Ibrutinib
Ibrutinib is an irreversible and selective inhibitor of Bruton's tyrosine kinase, a signaling molecule in the B-cell antigen receptor cascade which has been implicated in many B-cell malignancies. Advani et al.49 studied the outcome of ibrutinib therapy in 56 patients with relapsed/refractory B-cell malignancies, including 4 with WM. Among the 50 evaluable patients, a 60% response rate was observed (partial response and complete response), with median progression-free survival of 13.6 months in all patients. The maximum-tolerated dose was not reached, and no dose-limiting adverse events were observed. Most adverse events were low-grade (1 or 2) and easily manageable if not reversible. In a separate phase II study, 63 patients with symptomatic relapsed/refractory WM were treated with ibrutinib.26 Overall investigator-assessed response rate was 81%, while 57% achieved at least a major response. The response rate as assessed by an Independent Review Committee was 62% (95% confidence interval, 48.8, 73.9). The median time to achieve a response was 1.2 months. The most common side effects with ibrutinib are low blood counts, gastrointestinal symptoms, rash, muscle spasms and fatigue. Ibrutinib was approved by the Food and Drug Administration for the treatment of WM in 2015.
Carfilzomib
Carfilzomib is a proteasome inhibitor, which unlike bortezomib, is considered neuropathy-sparing. A phase II trial of 31 patients with symptomatic WM, previously treated with rituximab or bortezomib, were treated with carfilzomib, rituximab and dexamethasone.25 Overall response rate of 87% was observed. The most common toxicities included hyperglycemia secondary to dexamethasone, and elevated serum lipase, both of which were asymptomatic and reversible. Grade 1–2 peripheral neuropathy was seen in 19% of patients.
Approach to initial therapy
There are no good data from randomized trials to guide the choice of initial therapy in WM among modern regimens. Initial therapy for WM is usually given for approximately 6 months, and then patients are observed. We prefer DRC as the initial treatment regimen as it is convenient, effective and does not compromise the ability to collect stem cells (Figure 1).8 Two reasonable alternative options would be bortezomib, rituximab, dexamethasone and BR. The choice of initial therapy varies according to cost and drug availability in various countries. In WM patients with mild anemia as the main criterion for initiating therapy who have IgM levels less than 3 gm/dl, single-agent rituximab may be a reasonable option for initial therapy.8, 17 However, it will take many months for a decrease in IgM levels to occur with rituximab alone. Ibrutinib has been recently approved for the treatment of WM in the United States, but there are limited data in the front-line setting. In patients who are not considered candidates for transplantation, additional options include a purine nucleoside analog such as cladribine.
Response to therapy
Many of the initial studies on treatment of WM used different criteria for response to therapy, making it difficult to compare results. A standardized response criterion to measure the effect of treatment has been created by the International Working Group on Waldenstrom macroglobulinemia.50, 51 Patients are evaluated prior to each cycle of treatment to assess response to therapy. Complete response is defined as the disappearance of serum and urine monoclonal protein (assessed by immunofixation), normal serum IgM level, resolution of lymphadenopathy and organomegaly, lack of histologic bone marrow involvement, and absence of signs and symptoms attributable to WM. This must be confirmed 6 weeks later with a second immunofixation. Very good partial response is at least 90% reduction in serum IgM, resolution of lymphadenopathy and organomegaly, and resolution of symptoms. Partial response requires between 50 and 90% reduction in serum monoclonal IgM, at least 50% reduction in adenopathy and organomegaly, with no new signs or symptoms of active disease. Minor response requires between 25 and 50% reduction in serum monoclonal IgM without new signs or symptoms of active disease. Progressive disease is defined as two measurements showing at least 25% increase in serum monoclonal IgM, or progression of anemia/thrombocytopenia/leukopenia, adenopathy/organomegaly or increase in symptoms attributed to WM. Finally, stable disease are those which do not meet the criteria for minor response or progressive disease. 'Major response' includes complete response, very good partial response or partial response. Resolution of organomegaly must be confirmed by imaging. After completion of treatment, patients should undergo surveillance every 3 months for the first year, then every 6 months. This evaluation should include a complete history and physical exam, complete blood count, and measurement of monoclonal IgM in the serum or urine. Imaging should only be obtained if indicated by symptoms.
Management of relapsed disease
Relapse is associated with an increase in the IgM monoclonal protein in the serum along with associated symptoms of WM. In many patients, the IgM protein level may not be as high at relapse as it was at the time of initial diagnosis, even when the tumor burden and symptoms are similar.8 Unfortunately, given that WM is incurable, almost all patients will relapse after initial therapy.
In patients who achieve an initial major response, the decision to resume therapy should be based on recurrence of cytopenias or symptoms, rather than monoclonal protein levels alone. Type of therapy used at the time of relapse is determined by the response to initial therapy (Figure 2). In symptomatic patients relapsing >1–2 years after initial therapy, the original treatment can be repeated. On the other hand, for relapse occurring <1–2 years after initial treatment, an alternative regimen is used. The regimens listed on Table 2 can be tried in a sequential manner as appropriate. Besides regimens used in the front-line setting, the other options for therapy in previously treated patients include ibrutinib, lenalidomide and chlorambucil.
Stem cell transplantation
Select patients, who have good performance status and whose disease is chemo-sensitive at the time of transplant, may be candidates for high-dose chemotherapy followed by autologous HCT at first relapse.52 Studies have shown good outcomes with autologous HCT in previously treated and treatment-naïve patients.53 In the European Group for Blood and Marrow Transplantation (EBMT) study, autologous HCT was generally well tolerated, with non-relapse mortality of approximately 4% at 1 year. 54 The 5-year progression-free and overall survival rates were 39.7% and 68.5%, respectively. Similar results have been reported by other groups.9 Although good outcomes can still be seen in patients who have received multiple previous lines of therapies, and those who are considered refractory to therapy at the time of transplant, both of these factors do adversely affect expected outcomes.
Allogenic stem cell transplant has also been evaluated.55 In a study of 86 patients by the Lymphoma Working Party of the EBMT, the non-relapse mortality at 3 years was 33% for myeloablative and 23% for non-myeloablative allogeneic transplantation. The 5-year progression-free and overall survival rates were 56% and 62%, respectively, for myeloablative transplantation and 49% and 64%, respectively, for non-myeloablative transplantation. At present, it is preferable to consider allogeneic transplantation in patients with WM mainly in the setting of clinical trials.
Future directions
Major advances have occurred in the diagnosis and treatment of WM, including several new options for therapy. We now need comparative clinical trials to determine the optimal choice of therapy in the front-line setting, role of transplantation and the sequence of treatments. For example, the approval of ibrutinib for WM is exciting, but we need studies in the front-line setting to determine the role of this agent relative to other commonly used regimens in WM. As WM generally has a chronic indolent course, care should be exercised in picking treatments that do not disrupt quality of life. It is therefore important that future studies compare treatment options using patient-reported quality of life outcome measures in addition to standard metrics of depth and duration of response. Finally, we need additional studies to determine the role of the MYD88 L265P mutation in pathogenesis, especially with regard to the role in transformation of IgM MGUS to WM.
References
Gertz MA . Waldenstrom macroglobulinemia: 2013 update on diagnosis, risk stratification, and management. Am J Hematol 2013; 88: 703–711.
Treon SP, Xu L, Yang G, Zhou Y, Liu X, Cao Y et al. MYD88 L265P somatic mutation in Waldenstrom's macroglobulinemia. N Engl J Med 2012; 367: 826–833.
Treon SP, Cao Y, Xu L, Yang G, Liu X, Hunter ZR . Somatic mutations in MYD88 and CXCR4 are determinants of clinical presentation and overall survival in Waldenstrom macroglobulinemia. Blood 2014; 123: 2791–2796.
Castillo JJ, Olszewski AJ, Cronin AM, Hunter ZR, Treon SP . Survival trends in Waldenstrom macroglobulinemia: an analysis of the Surveillance, Epidemiology and End Results database. Blood 2014; 123: 3999–4000.
Garcia-Sanz R, Montoto S, Torrequebrada A, de Coca AG, Petit J, Sureda A et al. Waldenstrom macroglobulinaemia: presenting features and outcome in a series with 217 cases. Br J Haematol 2001; 115: 575–582.
Dimopoulos MA, Kyle RA, Anagnostopoulos A, Treon SP . Diagnosis and management of Waldenstrom's macroglobulinemia. J Clin Oncol 2005; 23: 1564–1577.
Castillo JJ, Ghobrial IM, Treon SP . Biology, prognosis, and therapy of waldenstrom macroglobulinemia. Cancer Treat Res 2015; 165: 177–195.
Ansell SM, Kyle RA, Reeder CB, Fonseca R, Mikhael JR, Morice WG et al. Diagnosis and management of Waldenstrom macroglobulinemia: Mayo stratification of macroglobulinemia and risk-adapted therapy (mSMART) guidelines. Mayo Clin Proc 2010; 85: 824–833.
Dimopoulos MA, Kastritis E, Owen RG, Kyle RA, Landgren O, Morra E et al. Treatment recommendations for patients with Waldenstrom macroglobulinemia (WM) and related disorders: IWWM-7 consensus. Blood 2014; 124: 1404–1411.
Morel P, Duhamel A, Gobbi P, Dimopoulos MA, Dhodapkar MV, McCoy J et al. International prognostic scoring system for Waldenstrom macroglobulinemia. Blood 2009; 113: 4163–4170.
Gobbi PG, Baldini L, Broglia C, Goldaniga M, Comelli M, Morel P et al. Prognostic validation of the international classification of immunoglobulin M gammopathies: a survival advantage for patients with immunoglobulin M monoclonal gammopathy of undetermined significance? Clin Cancer Res 2005; 11: 1786–1790.
Baldini L, Goldaniga M, Guffanti A, Broglia C, Cortelazzo S, Rossi A et al. Immunoglobulin M monoclonal gammopathies of undetermined significance and indolent Waldenstrom's macroglobulinemia recognize the same determinants of evolution into symptomatic lymphoid disorders: proposal for a common prognostic scoring system. J Clin Oncol 2005; 23: 4662–4668.
Alexanian R, Weber D, Delasalle K, Cabanillas F, Dimopoulos M . Asymptomatic Waldenstrom's macroglobulinemia. Semin Oncol 2003; 30: 206–210.
Dhodapkar MV, Jacobson JL, Gertz MA, Rivkin SE, Roodman GD, Tuscano JM et al. Prognostic factors and response to fludarabine therapy in patients with Waldenstrom macroglobulinemia: results of United States intergroup trial (Southwest Oncology Group S9003). Blood 2001; 98: 41–48.
Ghobrial IM, Fonseca R, Gertz MA, Plevak MF, Larson DR, Therneau TM et al. Prognostic model for disease-specific and overall mortality in newly diagnosed symptomatic patients with Waldenstrom macroglobulinaemia. Br J Haematol 2006; 133: 158–164.
Hivert B, Caron C, Petit S, Charpy C, Fankam-Siaka C, Lecocq S et al. Clinical and prognostic implications of low or high level of von Willebrand factor in patients with Waldenstrom macroglobulinemia. Blood 2012; 120: 3214–3221.
Gertz MA, Rue M, Blood E, Kaminer LS, Vesole DH, Greipp PR . Multicenter phase 2 trial of rituximab for Waldenstrom macroglobulinemia (WM): an Eastern Cooperative Oncology Group Study (E3A98). Leuk Lymphoma 2004; 45: 2047–2055.
Buske C, Hoster E, Dreyling M, Eimermacher H, Wandt H, Metzner B et al. The addition of rituximab to front-line therapy with CHOP (R-CHOP) results in a higher response rate and longer time to treatment failure in patients with lymphoplasmacytic lymphoma: results of a randomized trial of the German Low-Grade Lymphoma Study Group (GLSG). Leukemia 2009; 23: 153–161.
Rummel MJ, Al-Batran SE, Kim SZ, Welslau M, Hecker R, Kofahl-Krause D et al. Bendamustine plus rituximab is effective and has a favorable toxicity profile in the treatment of mantle cell and low-grade non-Hodgkin's lymphoma. J Clin Oncol 2005; 23: 3383–3389.
Treon SP, Ioakimidis L, Soumerai JD, Patterson CJ, Sheehy P, Nelson M et al. Primary therapy of Waldenstrom macroglobulinemia with bortezomib, dexamethasone, and rituximab: WMCTG clinical trial 05-180. J Clin Oncol 2009 Aug 10; 27: 3830–3835.
Dimopoulos MA, Anagnostopoulos A, Kyrtsonis MC, Zervas K, Tsatalas C, Kokkinis G et al. Primary treatment of Waldenstrom macroglobulinemia with dexamethasone, rituximab, and cyclophosphamide. J Clin Oncol 2007; 25: 3344–3349.
Tedeschi A, Benevolo G, Varettoni M, Battista ML, Zinzani PL, Visco C et al. Fludarabine plus cyclophosphamide and rituximab in Waldenstrom macroglobulinemia: an effective but myelosuppressive regimen to be offered to patients with advanced disease. Cancer 2012; 118: 434–443.
Treon SP, Branagan AR, Ioakimidis L, Soumerai JD, Patterson CJ, Turnbull B et al. Long-term outcomes to fludarabine and rituximab in Waldenstrom macroglobulinemia. Blood 2009; 113: 3673–3678.
Laszlo D, Andreola G, Rigacci L, Fabbri A, Rabascio C, Mancuso P et al. Rituximab and subcutaneous 2-chloro-2'-deoxyadenosine combination treatment for patients with Waldenstrom macroglobulinemia: clinical and biologic results of a phase II multicenter study. J Clin Oncol 2010; 28: 2233–2238.
Treon SP, Tripsas CK, Meid K, Kanan S, Sheehy P, Chuma S et al. Carfilzomib, rituximab, and dexamethasone (CaRD) treatment offers a neuropathy-sparing approach for treating Waldenstrom's macroglobulinemia. Blood 2014; 124: 503–510.
Treon SP, Tripsas CK, Yang G, Cao Y, Xu L, Hunter Z et al. A prospective multicenter study of the Bruton’s tyrosine kinase inhibitor ibrutinib in patients with relapsed or refractory Waldenstrom’s macroglobulinemia. Blood 2013; 122: 251.
Treon SP, Soumerai JD, Branagan AR, Hunter ZR, Patterson CJ, Ioakimidis L et al. Thalidomide and rituximab in Waldenstrom macroglobulinemia. Blood 2008; 112: 4452–4457.
Treon SP, Agus TB, Link B, Rodrigues G, Molina A, Lacy MQ et al. CD20-directed antibody-mediated immunotherapy induces responses and facilitates hematologic recovery in patients with Waldenstrom's macroglobulinemia. J Immunother 2001; 24: 272–279.
Treon SP, Emmanouilides C, Kimby E, Kelliher A, Preffer F, Branagan AR et al. Extended rituximab therapy in Waldenstrom's macroglobulinemia. Ann Oncol 2005; 16: 132–138.
Weide R, Heymanns J, Koppler H . The polyneuropathy associated with Waldenstrom's macroglobulinaemia can be treated effectively with chemotherapy and the anti-CD20 monoclonal antibody rituximab. Br J Haematol 2000; 109: 838–841.
Treon SP, Hanzis C, Manning RJ, Ioakimidis L, Patterson CJ, Hunter ZR et al. Maintenance rituximab is associated with improved clinical outcome in rituximab naive patients with Waldenstrom macroglobulinaemia who respond to a rituximab-containing regimen. Br J Haematol 2011; 154: 357–362.
Treon SP, Hunter ZR, Matous J, Joyce RM, Mannion B, Advani R et al. Multicenter clinical trial of bortezomib in relapsed/refractory Waldenstrom's macroglobulinemia: results of WMCTG Trial 03-248. Clin Cancer Res 2007; 13: 3320–3325.
Dimopoulos MA, Gertz MA, Kastritis E, Garcia-Sanz R, Kimby EK, Leblond V et al. Update on treatment recommendations from the Fourth International Workshop on Waldenstrom's Macroglobulinemia. J Clin Oncol 2009; 27: 120–126.
Dimopoulos MA, Garcia-Sanz R, Gavriatopoulou M, Morel P, Kyrtsonis MC, Michalis E et al. Primary therapy of Waldenstrom macroglobulinemia (WM) with weekly bortezomib, low-dose dexamethasone, and rituximab (BDR): long-term results of a phase 2 study of the European Myeloma Network (EMN). Blood 2013; 122: 3276–3282.
Palumbo A, Bringhen S, Rossi D, Cavalli M, Ria R, Gentilini S et al. Overall survival benefit for bortezomib-melphalan-prednisone-thalidomide followed by maintenance with bortezomib-thalidomide (VMPT-VT) versus bortezomib-melphalan-prednisone (VMP) in newly diagnosed multiple myeloma patients. ASH Annual Meeting Abstracts 2012; 120: 200.
Mateos MV, Oriol A, Martinez-Lopez J . Bortezomib/melphalan/prednisone (VMP) versus Bortezomib/Thalidomide/Prednisone (VTP) as induction therapy followed by maintenance treatment with Bortezomib/Thalidomide (VT) versus Bortezomib/Prednisone (VP): A randomised trial in elderly untreated patients with multiple myeloma older than 65 years. Lancet Oncol 2010; 11: 934–941.
Moreau P, Pylypenko H, Grosicki S, Karamanesht I, Leleu X, Grishunina M et al. Subcutaneous versus intravenous administration of bortezomib in patients with relapsed multiple myeloma: a randomised, phase 3, non-inferiority study. Lancet Oncol 2011; 12: 431–440.
Rajkumar SV . Multiple myeloma: 2014 Update on diagnosis, risk-stratification, and management. Am J Hematol 2014; 89: 998–1009.
Treon SP, Hanzis C, Tripsas C, Ioakimidis L, Patterson CJ, Manning RJ et al. Bendamustine therapy in patients with relapsed or refractory Waldenstrom's macroglobulinemia. Clin Lymphoma Myeloma Leuk 2011; 11: 133–135.
Rummel MJ, Niederle N, Maschmeyer G, Banat GA, von Grunhagen U, Losem C et al. Bendamustine plus rituximab versus CHOP plus rituximab as first-line treatment for patients with indolent and mantle-cell lymphomas: an open-label, multicentre, randomised, phase 3 non-inferiority trial. Lancet 2013; 381: 1203–1210.
Tamburini J, Levy V, Chaleteix C, Fermand JP, Delmer A, Stalniewicz L et al. Fludarabine plus cyclophosphamide in Waldenstrom's macroglobulinemia: results in 49 patients. Leukemia 2005; 19: 1831–1834.
Laurencet FM, Zulian GB, Guetty-Alberto M, Iten PA, Betticher DC, Alberto P . Cladribine with cyclophosphamide and prednisone in the management of low-grade lymphoproliferative malignancies. Br J Cancer 1999; 79: 1215–1219.
Van Den Neste E, Louviaux I, Michaux JL, Delannoy A, Michaux L, Sonet A et al. Phase I/II study of 2-chloro-2'-deoxyadenosine with cyclophosphamide in patients with pretreated B cell chronic lymphocytic leukemia and indolent non-Hodgkin's lymphoma. Leukemia 2000; 14: 1136–1142.
Tam CS, Wolf M, Prince HM, Januszewicz EH, Westerman D, Lin KI et al. Fludarabine, cyclophosphamide, and rituximab for the treatment of patients with chronic lymphocytic leukemia or indolent non-Hodgkin lymphoma. Cancer 2006; 106: 2412–2420.
Leblond V, Johnson S, Chevret S, Copplestone A, Rule S, Tournilhac O et al. Results of a randomized trial of chlorambucil versus fludarabine for patients with untreated Waldenstrom macroglobulinemia, marginal zone lymphoma, or lymphoplasmacytic lymphoma. J Clin Oncol 2013; 31: 301–307.
Carney DA, Westerman DA, Tam CS, Milner A, Prince HM, Kenealy M et al. Therapy-related myelodysplastic syndrome and acute myeloid leukemia following fludarabine combination chemotherapy. Leukemia 2010; 24: 2056–2062.
Treon SP, Soumerai JD, Hunter ZR, Patterson CJ, Ioakimidis L, Kahl B et al. Long-term follow-up of symptomatic patients with lymphoplasmacytic lymphoma/Waldenstrom macroglobulinemia treated with the anti-CD52 monoclonal antibody alemtuzumab. Blood 2011; 118: 276–281.
Treon SP, Soumerai JD, Branagan AR, Hunter ZR, Patterson CJ, Ioakimidis L et al. Lenalidomide and rituximab in Waldenstrom's macroglobulinemia. Clin Cancer Res 2009; 15: 355–360.
Advani RH, Buggy JJ, Sharman JP, Smith SM, Boyd TE, Grant B et al. Bruton tyrosine kinase inhibitor ibrutinib (PCI-32765) has significant activity in patients with relapsed/refractory B-cell malignancies. J Clin Oncol 2013; 31: 88–94.
Weber D, Treon SP, Emmanouilides C, Branagan AR, Byrd JC, Blade J et al. Uniform response criteria in Waldenstrom's macroglobulinemia: consensus panel recommendations from the Second International Workshop on Waldenstrom's Macroglobulinemia. Semin Oncol 2003; 30: 127–131.
Owen RG, Kyle RA, Stone MJ, Rawstron AC, Leblond V, Merlini G et al. Response assessment in Waldenstrom macroglobulinaemia: update from the VIth International Workshop. Br J Haematol 2013; 160: 171–176.
Gertz MA, Reeder CB, Kyle RA, Ansell SM . Stem cell transplant for Waldenstrom macroglobulinemia: an underutilized technique. Bone Marrow Transplant 2011; 47: 1147–1153.
Usmani S, Sexton R, Crowley J, Barlogie B . Autologous stem cell transplantation as a care option in Waldenstrom's macroglobulinemia. Clin Lymphoma Myeloma Leuk 2011; 11: 139–142.
Kyriakou C, Canals C, Sibon D, Cahn JY, Kazmi M, Arcese W et al. High-dose therapy and autologous stem-cell transplantation in Waldenstrom macroglobulinemia: the Lymphoma Working Party of the European Group for Blood and Marrow Transplantation. J Clin Oncol 2010; 28: 2227–2232.
Kyriakou C, Canals C, Cornelissen JJ, Socie G, Willemze R, Ifrah N et al. Allogeneic stem-cell transplantation in patients with Waldenstrom macroglobulinemia: report from the Lymphoma Working Party of the European Group for Blood and Marrow Transplantation. J Clin Oncol 2010; 28: 4926–4934.
Acknowledgements
This work is supported in part by grants CA 107476 and CA 168762 from the National Cancer Institute, Rockville, MD, USA.
Author Contributions
AO and SVR conceived of the paper, researched the literature and wrote the manuscript. All authors reviewed and approved the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Oza, A., Rajkumar, S. Waldenstrom macroglobulinemia: prognosis and management. Blood Cancer Journal 5, e394 (2015). https://doi.org/10.1038/bcj.2015.28
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bcj.2015.28
This article is cited by
-
Early progression is associated with worse survival in patients with Waldenström’s macroglobulinemia
Holistic Integrative Oncology (2024)
-
Waldenström Macroglobulinemia: Clinico-pathological Profile and Treatment Outcomes of Patients from a Tertiary Care Centre of North India
Indian Journal of Hematology and Blood Transfusion (2021)
-
Incidence, prevalence, mortality, and causes of death in Waldenström macroglobulinemia: a nationwide, population-based cohort study
BMC Cancer (2020)
-
MYD88 and CXCR4 Mutation Profiling in Lymphoplasmacytic Lymphoma/Waldenstrom’s Macroglobulinaemia
Indian Journal of Hematology and Blood Transfusion (2019)
-
Waldenstrom macroglobulinemia cells devoid of BTKC481S or CXCR4WHIM-like mutations acquire resistance to ibrutinib through upregulation of Bcl-2 and AKT resulting in vulnerability towards venetoclax or MK2206 treatment
Blood Cancer Journal (2017)