Abstract
Cartilage-hair hypoplasia (CHH) is an autosomal recessive disorder that presents with pleiotropic manifestations including impaired skeletal growth and cellular immunity. It is most prevalent among two founder populations, the Old Order Amish in the USA and the Finns. The gene has been localized to 9p13 by linkage analysis and linkage disequilibrium mapping. A statistically significant deficiency of affected members resulting in a lower than expected segregation ratio has been reported in the Amish, but was not found in a previous study in Finnish CHH families. Reduced penetrance was the mechanism suggested in the Amish, but could not be verified by haplotype analyses performed after the assignment of the CHH gene. Here we have carried out segregation analysis of 101 Finnish CHH families, but again, evidence of a significant deficiency of affected members was not found. Nevertheless, among 54 uniplex families, 2 patients with CHH and uniparental disomy (UPD) for chromosome 9 were discovered. UPD might contribute to low segregation ratios by increasing the number of families with only 1 affected individual. These observations show that UPD may occur in an unexpectedly high number of the patients and should be taken into account in the genetic counselling and prenatal diagnostics of CHH families.
Similar content being viewed by others
Introduction
Cartilage-hair hypoplasia (CHH) is an autosomal recessive chondrodysplasia resulting in a severe growth failure. Other main clinical features include impaired hair growth, cellular immunity and erythropoiesis, and, in some patients, aganglionic megacolon [1, 2]. CHH is particularly frequent among the Old Order Amish in the USA [1] and the Finns [3]. The gene maps to 9p21–p13 and is very closely linked to marker D9S163 [4–6].
A statistically significant deficiency of affected members (72 observed vs. 98 ± 6.8 expected by the ‘a priori’ correction method) resulting in a lower than expected segregation ratio (i.e. <0.25) has been reported in the Amish CHH series [1]. However, segregation analysis of 83 Finnish families (105 affected children observed, 111 ± 5 expected [3]) failed to show a corresponding deficiency of affected members. In the Amish series, many possible explanations including prenatal death of some homozygotes and nonrandom chromosome segregation were considered, but reduced penetrance (70%) was suggested as the most likely mechanism. After the CHH locus had been assigned to proximal 9p and several closely linked polymorphic markers had been identified [4, 5], it became possible to search for reduced penetrance by determining the haplotypes of unaffected siblings in multiplex families. We studied 66 clinically unaffected siblings from Finnish and Amish families and found none haploidentical with affected sibs. Therefore we previously suggested that barring rare crossovers the deficiency of affected children in CHH families is most probably not due to reduced penetrance nor to underdiagnosis of mildly manifesting individuals [5].
This study was initially prompted by the observation of a child with CHH and uniparental disomy (UPD) for chromosome 9 in a Finnish family counselled for prenatal diagnostics. UPD is a state where both homologues of a chromosome pair are inherited from a single parent [7], and it may contribute to low segregation ratios by increasing the number of families with only one affected child: in UPD families occurrence of more than one affected child is very unlikely when only one parent carries the defective mutation. We performed segregation analysis in an extended series of Finnish CHH families and turned to uniplex families in order to look for more UPD cases. Although segregation analysis of 101 families still failed to give evidence of a statistically significant deficiency of affected members, the study of 54 uniplex families revealed 1 additional patient with CHH and UPD for chromosome 9. We conclude that UPD seems to occur in an unexpectedly high number of the Finnish CHH patients and should be taken into account in the genetic counselling of CHH families.
Subjects and Methods
Diagnostic Criteria
The principal clinical manifestation of CHH is severe growth failure. Other main clinical features include impaired hair growth, cellular immunity and erythropoiesis, and, in some patients, aganglionic megacolon [1, 2]. The diagnosis is based on these clinical features and on metaphyseal irregularities of the growth plates in childhood radiographs [8].
Patients
Altogether 68 Finnish CHH families with 84 affected individuals were studied. There were 54 uniplex families. Among the affected members in uniplex families, 4 unrelated individuals homozygous for a number of markers in the vicinity of the CHH gene were found.
Patient A was a daughter of healthy unrelated parents (maternal and paternal ages at birth were 30 and 31 years, respectively) and had one unaffected sister. She was born at 36 weeks of gestation, measuring 36.5 cm in length and 1,900 g in weight. At the age of 2 years her growth was severely impaired (−8.6 SD below normal mean; below 10th percentile on CHH-specific growth curves [8]). Hair was extremely thin, sparse, and light in color, and she had mild relative lymphopenia and impaired cellular immunity. In early childhood she suffered from chronic obstipation. In addition to the diagnostic features of CHH, she had mild aortic stenosis and clubfeet.
Patient B was a daughter of healthy unrelated parents (maternal and paternal ages at birth were 28 and 32 years, resepectively) and had two unaffected siblings. At the age of 12 years her growth was severely retarded (−15.5 SD below normal mean, below 10th percentile on CHH-specific growth curves). Hair was thin, sparse and light in color. She had combined immunodeficiency; immunological studies in early childhood revealed markedly depressed responses of the blood lymphocytes to phytohemagglutinin, concavalin A, and poke-weed mitogen, and at the age of 10 years she developed hypogammaglobulinemia. She has had several prolonged infections including recurrent respiratory infections, chronic otitis media, and chronic sinusitis. She had hypoplastic macrocytic anemia which had been treated with repeated red cell transfusions. At the age of 11 years she developed autoimmune hemolytic anemia. She also had an unspecified cardiomyopathy in infancy, and marked hepatosplenomegaly. In addition, prolonged hypokalemia, vitamin K deficiency, transient neutropenia, diarrhea due to Trichuris trichiura, and vitamin D deficiency with hypocalcemic tetany have been detected.
Patient C had severe growth failure (25th percentile on CHH-specific growth curves), a history of hypoplastic anemia in early childhood, and defective cellular immunity but no severe infections. Patient D had moderate growth failure (75th percentile on CHH-specific growth curves), thin hair but no immunodeficiency or anemia.
Analysis of DNA
Genomic DNA was extracted either from blood or lymphoblastoid cell lines according to standard procedures. Altogether 24 chromosome 9-specific microsatellite markers and 21 markers from all other autosomes and the X chromosome were studied in patients A and B. In patients C and D, 12 chromosome 9 markers were studied. The widest gap between the markers on chromosome 9 was 28 cM [9]. The detection of polymorphisms was carried out as described previously [4].
Fluorescent in situ Hybridization Studies
In order to investigate the possibility of a short deletion in the CHH gene region in patients C and D, a fluorescent in situ hybridization (FISH) experiment was set up. Chromosome preparations were made from blood lymphocyte cultures and lymphoblastoid cell lines [10] using standard procedures. For the FISH experiments the slides were pretreated with pepsin (0.01 mg/ml), washed 4 times in destilled water, and dehydrated in an ethanol series to remove excess cytoplasm. Slides were denatured in 70% formamide/2 × SSC (vol 1:1) at 70 ° C for 3 min and dehydrated in a cold ethanol series.
P1 clone 2902 (Genome Systems, St. Louis, Mo., USA) identified by the marker D9S163 was used as a probe in the FISH experiments. Plasmid DNA was extracted by the alkaline lysis procedure with minor modifications [11, 12]. It was nick-labelled with biotin 14-dATP as recommended by the kit supplier (Gibco BRL, Bethesda, Md., USA). The labelled probe was precipitated with human Cot-1 DNA and herring sperm DNA. Hybridization was performed in a total volume of 1 ml of a solution containing 50 µg of biotinylated probe, 1 mg of human Cot-1 DNA, 1 mg of herring sperm DNA, 50% formamide, and 10% dextran sulfate, in 2 x SSC. The hybridization was performed according to Cremer et al. [13] with some modifications. The mixture was denatured at 75 ° C for 5 min and 30 µl added to each slide. The slides were covered with coverslips and incubated overnight at 37 ° C in a moist chamber. After incubation, the slides were washed 3 times at 44 ° C in 50% formamide/2 × SSC, 2 times in 2 × SSC, and once in 0.01 × SSC, each wash for 5 min. Hybridization signals were detected with avidin-conjugated fluorescein isothiocyanate (FITC) as described in Pinkel et al. [14]. The cells were counterstained with 4,6-diamidino-2-phenylindole (DAPI) and propidium iodide. The cells were mounted with Vectashield™ antifading and analyzed using a Zeiss Laborlux fluorescence photomicroscope with Zeiss filters 02 (FITC) and 09 (DAPI).
Segregation Analysis
The methods of ascertainment have been described previously [3]. The segregation analysis was performed using the ‘singles’, ‘a priori’, and ‘a posteriori’ methods, each assuming complete ascertainment, and by the ‘sib’ method which assumes single incomplete ascertainment.
Results
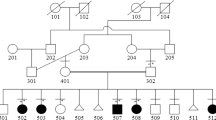
Patients A and B and their parents were studied for altogether 24 markers spanning the entire chromosome 9 (fig. 1). Patient A was homozygous for all marker loci studied. Twelve markers were completely informative and showed no paternal contribution, and, therefore, isodisomic inheritance of a maternal homologue of chromosome 9 is suggested. Patient B was homozygous for the majority of the markers. Of these, 11 were informative suggesting exclusively maternal inheritance of chromosome 9. No conclusively paternal allele was detected. However, the patient was heterozygous for markers D9S153, D9S167 and D9S197 on proximal 9q, and for ASS, D9S164 and D9S158 on distal 9q. Of these, markers D9S197 and D9S164 showed conclusively that the patient had inherited both maternal alleles. This patient is thus suggested to be partially isodisomic and partially heterodisomic for the maternal homologues. To evaluate the likelihood of false paternity, both families were typed for selected markers from all other autosomes and the X chromosome (table 1). In patients A and B markers from nine and eleven chromosomes, respectively, showed definite allele contribution from both parents. The rest of the combinations were not fully informative in respect to parental origin of the alleles, but no ‘extra’ alleles at any of the marker loci were observed. Therefore, nonpaternity was highly unlikely (p ≈ 1.3 × 10−10). The karyotype of patient A was determined from G-banded chromosomes and found to be normal. No chromosomal heteromorphisms allowing the derivation of the chromosomes 9 were present [data not shown]. As the proliferation of lymphocytes was seriously depressed in patient B (a characteristic feature of CHH), her chromosomes could not be analyzed.
Haplotype analysis of 22 chromosome 9 markers. The physical locations of 8 markers are shown on the left. The interval harboring the CHH gene is shown as a vartical bar [5, 6]. Superscript ‘a’ indicates a marker showing linkage to the CHH gene, superscript ‘b’ a marker demonstrating isodisomy, and superscript ‘c’ a marker demonstrating heterodisomy.
The clinical features of patients A and B are shown in table 2. In patient A, growth was severely retarded (fig. 2), hair was very hypoplastic, and there was marked ligamentous laxity, whereas the other features were only moderate or mild in severity. Additional atypical features in patient A were mild clubfeet and aortic stenosis. Patient B was also very severely affected (table 2). She had late onset B cell immunodeficiency, i.e. combined immunodeficiency which occasionally has been observed in patients with CHH [28, 29]. Atypical features in patient B included late onset hemolytic anemia, and, in early childhood, unspecified cardiomyopathy that subsided, and marked hepatomegalia.
Growth of CHH patients A and B with UPD as compared to the 10th and 90th percentile CHH-specific curves for 108 Finnish patients [2] and to ± 2 SD curves for normal Finnish girls.
Patients C and D were studied for chromosome 9 markers from D9S263 to D9S55 and for D9S168, D9S197, D9S195, and D9S158 [data not shown]. Patient C was homozygous for the markers from D9S43 to D9S55, whereas patient D was homozygous for the markers from D9S263 to D9S55. However, UPD was excluded in both cases as contributions from both parents were verified by allele segregation at D9S52 and D9S195 in patient C and at D9S168 and D9S197 in patient D.
Since the patients C and D were homozygous for a number of marker loci linked to the CHH gene and the possibility of UPD was excluded, a FISH experiment was performed to investigate whether these patients might carry a short deletion in this region. P1 clone 2902 identified by the closely linked marker D9S163 showing homozygosity in both patients was used as a probe. The results in patient C are shown in figure 3. Hybridization signals were found on 9p13 in both homologues in most metaphases. In patient D a similar result was obtained [data not shown].
Segregation analysis was done in a series of 101 Finnish CHH families including 125 affected members; 4 families had 3 affected children, 16 families had 2 affected children, and 81 families had only 1 affected child. There were altogether 164 unaffected siblings. The ‘singles’ and ‘a posteriori’ methods both gave a ratio of 0.212 (SE 0.036). By the ‘a priori’ method the expected number of patients was 130.2 (SE 5.1), whereas 125 patients were observed. The ‘sib’ method produced a ratio of 0.128 (SE 0.024) for the affected siblings.
Discussion
UPD is a state where both homologues of a chromosome pair are inherited from a single parent [7]. It may appear as isodisomy, i.e. an individual has inherited two copies of a single homologue, as heterodisomy, i.e. an individual has inherited both homologues of a chromosome pair, or as a combination of both if one or more recombinations have taken place during meiosis I. Possible mechanisms for the production of UPD include gamete complementation involving fertilization between one nullisomic and one disomic gamete for a particular chromosome, duplication of a chromosome in a monosomic zygote, early correction of a trisomic zygote through nondisjunction in somatic tissues, and postfertilization errors such as nondisjunction or duplication [30]. UPD may result in appearance of abnormal phenotypes. It is occasionally associated with developmental anomalies due to imprinting, i.e. differential functioning of genetic loci depending on their parental origin [31, 32]. So far, an imprinting effect has been confirmed for human chromosomes 7, 11, 14, and 15 [reviewed in 32]. Furthermore, UPD may cause occurrence of autosomal recessive diseases if two copies of a mutated gene are inherited from a single parent. This has been suggested in cases including 2 patients with cystic fibrosis (chromosome 7) [30, 33], and 1 patient with rod monochromacy (chromosome 14) [34], spinal muscular atrophy (chromosome 5) [35], Bloom syndrome (chromosome 15) [36], and chloride diarrhea (chromosome 7) [37].
In addition to CHH, lower than expected segregation ratios have been reported in autosomal recessive disorders including spinal muscular atrophy, osteogenesis imperfecta, and ataxia telangiectasia [reviewed in 38]. In addition to explanations due to parental behavior (false paternity, not reporting of previous affected children and parental decision against having further children) and observer errors, biological mechanisms may occur [1, 38]. These include genetic heterogeneity, low penetrance, early lethality of some homozygotes, gamete selection, UPD and hemizygosity owing to de novo deletion. All these mechanisms may increase the number of families with only 1 affected child and, thus, reduce the segregation ratio. Of the explanations listed above, both allelic and locus heterogeneity have been observed in human and murine osteogenesis imperfecta in which autosomal dominant and recessive forms have been reported and in which the autosomal dominant forms are often caused by new mutations [39, 40]. In spinal muscular atrophy, both a patient with UPD for chromosome 5 and patients with de novo deletions in the region spanning the disease locus in 5q13 have been reported [35, 41, 42].
Here we have described 2 CHH patients with UPD for chromosome 9. Patient A was homozygous for a maternal allele at all chromosome 9 loci studied, suggesting isodisomy for the entire chromosome, whereas patient B was partially isodisomic and heterodisomic for the maternal homologues, suggesting that at least three recombinations had occurred during maternal meiosis I. The heterodisomic areas were separated by approximately 51 cM, and the markers (D9S55 on 9p12 and D9S173 on 9q22.3–q31) flanked the area of the suggested double recombination by approximately 45 cM on a sex-averaged map [9]. The complete isodisomy in patient A was consistent with a mechanism including fertilization between a monosomic egg cell and a nullisomic sperm cell followed by a duplication, but gamete complementation (involving one nullisomic and one disomic gamete), trisomy ‘rescue’ or post-fertilization errors could not be excluded. In patient B the mechanism must have included fertilization of a disomic egg cell with either a nullisomic or monosomic sperm cell. As the CHH mutation is relatively common in Finland (carrier frequency 1/76 [3]), the mothers most likely are carriers and have transmitted two copies of the defective gene to their offspring although formal proof must wait until the gene and mutation(s) are identified. It might be noted that the mother of the maternal grandmother of patient B was born in a geographic region with high CHH gene frequency, whereas the roots of the father were in a region not showing an enrichment of the CHH gene. The maternal genealogy of patient A remained unknown.
Both patients with UPD were seriously affected in several clinical respects (table 2, fig. 2). In addition, both patients presented with some atypical but discordant manifestations. Severely retailed growth might result from a homozygous mutation or genomic imprinting of a hypothetical maternal growth-related gene on chromosome 9, as has been suggested for chromosome 7 [30, 33, 43–46]. However, CHH patients cannot provide a definite proof of an additional growth-related gene(s) on chromosome 9 as the condition itself presents with retarded growth [1, 8]. Furthermore, UPD was excluded in 9 Finnish CHH patients with similarly severe growth failure [data not shown]. A previously published report on an individual with maternal UPD for chromosome 9 does not allow more definite conclusions in this regard [47]. The patient carried two copies of a maternal homologue containing a pericentric inversion of the heterochromatic region (invp11q12), and a DNA analysis of polymorphic markers suggested a recombination having occurred in maternal meiosis I. In addition to UPD, the patient had trisomy 9 mosaicism which was found in a fraction of lymphocytes but not in skin or muscle cell cultures. The clinical features included mild retardation of growth (163 cm, below −2 SD of normal standards) and psychomotor development, but the relative contributions of UPD and trisomy mosaicism remained unclear [47].
Recently in spinal muscular atrophy, heterozygous de novo deletions of the critical region have been observed [41, 42]. The possibility of short de novo deletions in the CHH region was studied by FISH experiments in patients C and D who showed homozygosity for a number of markers close to the CHH gene but excluded UPD (fig. 3). In both patients a signal was detected on both chromatids of both homologues on proximal 9p, most probably on band 9p13, by a probe containing D9S163, a marker residing approximately 0.3 cM from the CHH gene [6]. This observation decreases the likelihood of a deletion. However, although the possibility of a short deletion (or segmental UPD) could not be excluded formally, it is most likely that the observed homozygosity simply reflects disomy for the conserved ancestral haplotype [6].
A statistically significant deficiency of affected members has been reported in the Amish CHH families [1], but corresponding analyses of 83 [3] or 101 (this study) Finnish families have failed to give evidence of a similar deficiency. However, despite the fact that the observed segregation ratio in the Finnish series is in accordance with the expected ratio of a recessive disease, UPD might provide at least a partial explanation for the low segregation ratio found in the Amish. The large Amish sibships (on average 6.3 children/family [1]) with only a single affected individual, of whatever cause, could distort the segregation ratio more easily than the smaller Finnish sibships (in the 101 CHH families available to us on average 2.9 children/family). However, none of the 12 patients in Amish uniplex families (or 12 sporadic patients from other populations than Finnish or Amish) studied by us so far has proved to be a UPD case [5, 48, unpubl. observations]. Therefore, we are unable to assess the likelihood that UPD (or de novo deletions) might be detected if further Amish families were carefully studied; this clearly should be done. If UPD is not detected, other causes should be sought.
Finally, we wish to recall the challenges to genetic counselling and prenatal diagnosis that UPD gives rise to. Contrary to all the rules of recessive inheritance, in UPD families only one of the parents needs to be a carrier. Although UPD is a rare event, it should be taken into account in the genetic counselling and prenatal diagnostics of CHH families.
References
McKusick VA, Eldridge R, Hostetier JA, Ruangwit U, Egeland JA: Dwarfism in the Amish. II. Cartilage-hair hypoplasia. Bull Johns Hopkins Hosp 1965;116:232–272.
Mäkitie O, Kaitila I: Cartilage-hair hypoplasia — Clinical manifestations in 108 Finnish patients. Eur J Pediatr 1993; 152:211–217.
Mäkitie O: Cartilage-hair hypoplasia in Finland — Epidemiological and genetic aspects of 107 patients. J Med Genet 1992;29:652–655.
Sulisalo T, Sistonen P, Hästbacka J, Wadelius C, Mäkitie O, de la Chapelle A, Kaitila I: Cartilage-hair hypoplasia gene assigned to chromosome 9 by linkage analysis. Nature Genet 1993; 3:338–341.
Sulisalo T, Francomano CA, Sistonen P, Maher JF, McKusick VA, de la Chapelle A, Kaitila I: High-resolution genetic mapping of the cartilage-hair hypoplasia (CHH) gene in Amish and Finnish families. Genomics 1994;20:347–353.
Sulisalo T, Klockars J, Mäkitie O, Francomano CA, de la Chapelle A, Kaitila I, Sistonen P: High-resolution linkage-disequilibrium mapping of the cartilage-hair hypoplasia gene. Am J Hum Genet 1994;55:937–945.
Engel E: A new genetic concept: Uniparental disomy and its potential effect, isodisomy. Am J Med Genet 1980;6:137–143.
Mäkitie O, Perheentupa J, Kaitila I: Growth in cartilage-hair hypoplasia. Pediatr Res 1992;31: 176–180.
Povey S, Armour J, Farndon P, Haines JL, Knowles M, Olopade F, Pilz A, White JA: Report on the third international workshop on chromosome 9. Ann Hum Genet 1994;58:177–250.
Anderson MA, Gusella JF: Use of cyclosporin A in establishing Epstein-Barr virus-transformed human lymphoblastoid cell lines. In Vitro 1984;20:856–858.
Birnboim HC, Doly J: A rapid alkaline extraction procedure for screening recombinant Plasmid DNA. Nucleic Acids Res 1979,7:1513–1523.
Pierce JC, Sternberg N: Using the bacteriophage P1 system to clone high molecular weight (HMW) genomic DNA. Methods Enzymol 1992;216:549–574.
Cremer T, Lichter P, Borden J, Ward DC, Manuelidis L: Detection of chromosome aberrations in metaphase and interphase tumor cells by in situ hybridization using chromosome-specific library probes. Hum Genet 1988; 80:235–246.
Pinkel D, Straume T, Gray JW: Cytogenetic analysis using quantitative, high-sensitivity, fluorescence hybridization. Proc Natl Acad Sci USA 1986;83:2934–2938.
Wilkie PJ, Krizman DB, Weber JL: Linkage map of human chromosome 9 microsatellite polymorphisms. Genomics 1992;12:607–609.
Weissenbach J, Gyapay G, Dib C, Vignal A, Morissette J, Millasseau P, Vaysseix G, Lathrop M: A second-generation linkage map of the human genome. Nature 1992;359:794–801.
Gyapay G, Morissette J, Vignal A, Dib C, Fizames C, Millasseau P, Marc S, Bernardi G, Lathrop M, Weissenbach J: The 1993–1994 Généthon human genetic linkage map. Nature Genet 1994;7:246–339.
Weber JL, May PE: Dinucleotide repeat polymorphism at the D9S43 locus. Nucleic Acids Res 1991;18:2203.
Graw SL, Kwiatkowski DJ: Three dinucleotide repeat polymorphisms on chromosome 9 (D9S200, D9S201, D9S199). Hum Mol Genet 1993;2:614.
Sharma V, Brown D, Smith C, Magenis RE, Litt M: Dinucleotide repeat polymorphism at the D9S55 locus. Nucleic Acids Res 1991;19: 4023.
Kwiatkowski DJ, Henske EP, Weimer K, Ozelius L, Gusella JF, Haines J: Construction of a GT polymorphism map of human 9q. Genomics 1992;12:229–240.
Ozelius L, Schuback DE, Stefansson K, Slaugenhaupt S, Gusella JF, Breakefield XO: Dinucleotide repeat polymorphism for the hexabrachion gene (HXB) on chromosome 9q32–34. Hum Mol Genet 1992;1:141.
Yuille MA, Hampson RM, Harris RM, Affara NA, Yates JR, Ferguson-Smith MA: CA repeat polymorphism at the ASS locus. Nucleic Acids Res 1990; 18:7472.
Morral N, Nunes V, Casals T, Estivill X: CA/GT microsatellite alleles within the cystic fibrosis transmembrane conductance regulator (CFTR) gene are not generated by unequal crossingover. Genomics 1991;10:692–698.
Weber JL, Kwitek AE, May PE: Dinucleotide repeat polymorphism at the D16S260, D16S261, D16S265, D16S266, and D16S267 loci. Nucleic Acids Res 1990; 18:4034.
Warren AC, McInnis MG, Blaschak J, Kaliatsidaki M, Petersen MB, Chakravarti A, Antonorakis SE: Dinucleotide repeat (GT)n markers on chromosome 21. Genomics 1992; 14:818–819.
Luty JA, Willard HF, Litt M: Three new microsatellite VNTRs on the X chromosome. Cytogenet Cell Genet 1989;51:1036.
Steele RW, Britton HA, Anderson CT, Kniker WT: Severe combined immunodeficiency with cartilage-hair hypoplasia: In vitro response to thymosin and attempted reconstitution. Pediatr Res 1976;10:1003–1005.
Rubie H, Graber D, Fischer A, Tauber MT, Maroteaux P, Robert A, Le Deist F, Rochiccilio P, Griscelli C, Régnier C: Hypoplasie du cartilage et des cheveux avec deficit immunitaire combiné. Ann Pédiatr (Paris) 1989;36: 390–392.
Spence JE, Perciaccante RG, Greig GM, Willard HF, Ledbetter DH, Hejtmancik JF, Pollack MS, O’Brien WE, Beaudet AL: Uniparental disomy as a mechanism for human genetic disease. Am J Hum Genet 1988;42:217–226.
Nicholls RD, Knoll JHM, Butler MG, Karam S, Lalande M: Genetic imprinting suggested by maternal heterodisomy in non-deletion Prader-Willi syndrome. Nature 1989;342:281–285.
Ledbetter DH, Engel E: Uniparental disomy in humans: Development of an imprinting map and its implications for prenatal diagnosis. Hum Mol Genet 1995;4:1757–1764.
Voss R, Ben-Simon E, Avital A, Godfrey S, Zlotogora J, Dagan J, Tikochinski Y, Hillel J: Isodisomy of chromosome 7 in a patient with cystic fibrosis: Could uniparental disomy be common in humans? Am J Hum Genet 1989; 45:373–380.
Pentao L, Lewis RA, Ledbetter DH, Patel PI, Lupski JR: Maternal uniparental isodisomy of chromosome 14: Association with recessive rod monochromacy. Am J Hum Genet 1992;50: 690–699.
Brzustowicz LM, Allitto BA, Matseoane D, Theve R, Michaud L, Chatkupt S, Sugarman E, Penchszadeh GK, Suslak L, Koenigsberger MR, Gilliam TC, Handelin BL: Paternal isodisomy for chromosome 5 in a child with spinal muscular atrophy. Am J Hum Genet 1994;54: 482–488.
Woodage T, Prasad M, Dixon JW, Selby RE, Romain DR, Columbano-Green LM, Graham D, Rogan PK, Seip JR, Smith A, Trent RJ: Bloom syndrome and maternal uniparental disomy for chromosome 15. Am J Hum Genet 1994;55:74–80.
Höglund P, Holmberg C, de la Chapelle A, Kere J: Paternal isodisomy for chromosome 7 is compatible with normal growth and development in a patient with congenital chloride diarrhea. Am J Hum Genet 1994;55:747–752.
Bundey S, Young ID: Low segregation ratios in autosomal recessive disorders. J Med Genet 1993;30:449–451.
Byers P: Osteogenesis imperfecta; in Royce PM, Steinman B (eds): Connective Tissue and Its Heritable Disorders. New York, Wiley-Liss, 1993, pp 317–350.
Guenet JL, Stanescu R, Maroteux P, Stanescu V: Fragilitas ossium: A new autosomal recessive mutation in the mouse. J Hered 1981;72: 440–441.
Melki J, Lefebvre S, Burglen L, Burlet P, Clermont O, Millasseau P, Reboullet S, Bénichou B, Zeviani M, Le Paslier D, Cohen D, Weissenbach J, Minnich A: De novo and inherited deletions of the 5q13 region in spinal muscular atrophies. Science 1994;264:1474–1477.
Rodrigues NN, Owen N, Talbot K, Ignatius J, Dubowitz V, Davies K: Deletions in the survival motor neuron gene on 5q13 in autosomal recessive spinal muscular atrophy. Hum Mol Genet 1995;4:631–634.
Spotila LD, Sereda L, Prockop DJ: Partial isodisomy for maternal chromosome 7 and short stature in an individual with a mutation at the COL1A2 locus. Am J Hum Genet 1992;51: 1396–1405.
Eggerding FA, Schonberg SA, Chehab FF, Norton ME, Cox VA, Epstein CJ: Uniparental isodisomy for paternal 7p and maternal 7q in a child with growth retardation. Am J Hum Genet 1994;55:253–265.
Kotzot D, Schmitt S, Bernasconi F, Robinson WP, Lurie IW, Ilyina H, Ménes K, Hamel BCJ, Otten BJ, Hergersberg M, Werder E, Schoenle E, Schinzel A: Uniparental disomy 7 in Silver-Russell syndrome and primordial growth retardation. Hum Mol Genet 1995;4:583–587.
Preece M, Price SM, Clough L, Davies VC, Stanier P, Trembath RC, Moore GE: Maternal uniparental disomy of chromosome 7 and Silver-Russell syndrome (abstract). Eur J Hum Genet 1996;4 (suppl 1):12.
Willatt LR, Davison BCC, Goudie D, Alexander J, Dyson HM, Jenks PE, Ferguson-Smith ME: A male with trisomy 9 mosaicism and maternal uniparental disomy for chromosome 9 in the euploid cell line. J Med Genet 1992;29: 742–744.
Sulisalo T, van der Burgt I, Rimoin DL, Bonaventure J, Sillence D, Campbell JB, Chitayat D, Scott CI, de la Chapelle A, Sistonen P, Kaitila I: Genetic homogeneity of cartilage-hair hypoplasia. Hum Genet 1995;95:157–160.
Acknowledgements
This study was supported by the Sigrid Jusélius Foundation, Finland, the March of Dimes Birth Defects Foundation (MOD FY94-0272), USA, and the Academy of Finland. Part of the study was done at the Folkhälsan Institute of Genetics.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sulisalo, T., Mäkitie, O., Sistonen, P. et al. Uniparental Disomy in Cartilage-Hair Hypoplasia. Eur J Hum Genet 5, 35–42 (1997). https://doi.org/10.1007/BF03405875
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF03405875