Abstract
Besides a variety of other proteases, polymorphonuclear leukocyte elastase (PMN-E) is also suggested to play a role in the processes of tumour cell invasion and metastasis. Yet, there is only limited data available on the relation between the tumour level of PMN-E and prognosis in patients with primary breast cancer, and no published information exists on its relation with the efficacy of response to systemic therapy in patients with advanced breast cancer. In the present study, we have measured with enzyme-linked immunosorbent assay the levels of total PMN-E in cytosolic extracts of 463 primary breast tumours, and have correlated their levels with the rate and duration of response on first-line tamoxifen therapy (387 patients) or chemotherapy (76 patients) in patients with locally advanced and/or distant metastatic breast cancer. Furthermore, the probabilities of progression-free survival and postrelapse survival were studied in relation to the tumour levels of PMN-E. Our results show that in logistic regression analysis for response to tamoxifen treatment in patients with advanced disease, high PMN-E tumour levels were associated with a poor rate of response compared with those with low PMN-E levels (odds ratio: OR, 0.40; 95% CI, 0.22–0.73; P=0.003). After correction for the contribution of the traditional predictive factors in multivariate analysis, the tumour PMN-E status was an independent predictor of response (P=0.01). Furthermore, a high tumour PMN-E level was related with a poor progression-free survival (P<0.001) and postrelapse survival (P=0.002) in a time-dependent analysis. In contrast, the tumour level of PMN-E was not significantly related with the efficacy of response to first-line chemotherapy in patients with advanced breast cancer. Our present results suggest that PMN-E is an independent predictive marker for the efficacy of tamoxifen treatment in patients with advanced breast cancer.
Similar content being viewed by others
Main
A complex cascade of proteinases, their receptors and inhibitors, are required for invasion of tumour cells through the extracellular matrix, for subsequent metastasis and angiogenesis (reviewed by Mignatti et al, 1986; Andreasen et al, 1997; Nelson et al, 2000). Tumour growth and angiogenesis are associated with a strong inflammatory response via the attraction of macrophages and polymorphonuclear (PMN) leukocytes by tumour cell-secreted chemoattractants (Jackson et al, 1997; Lee et al, 1997). In contrast to their attributed role in exterminating the tumour, recruited inflammatory cells have been reported to be associated with tumour progression as well (Scholl et al, 1994; Yamashita et al, 1994, 1996; Shamamian et al, 2000, 2001). The responsible protease is thought to be PMN-elastase (PMN-E), a serine protease that can degrade various components of the extracellular matrix directly (Janoff and Schere, 1968; Mainardi et al, 1980; McDonald and Kelley, 1980; Barrett, 1981), or indirectly through either the activation of other proteases (Machovich and Owen, 1990; Shamamian et al, 2001) or the inactivation of their inhibitors (Levin and Santell, 1987; Gramse et al, 1984; Wu et al, 1995). Furthermore, it has been shown that PMN-E is not only produced by neutrophils but by human breast cancer cells as well (Kao and Stern, 1986; Yamashita et al, 1994), and moreover can promote the adhesion of tumour cells to vascular endothelial cells facilitating its role in tumour metastasis (Nozawa et al, 2000).
In many types of cancer, various tumour-associated proteases and their inhibitors have been shown to be independent prognostic factors for relapse-free and overall survival. The most extensively studied protease systems involve those of the urokinase-type plasminogen activator (uPA) (reviewed by Andreasen et al, 1997; Schmitt et al, 1997a; Look and Foekens, 1999) and a variety of matrix metalloproteinases (MMPs) (reviewed by Duffy et al, 2000; Nelson et al, 2000). Similarly, high tumour levels of PMN-E have been reported to be associated with a poor prognosis in patients with primary breast cancer (Yamashita et al, 1994, 1995a, 1995b; Foekens et al, 2002) and nonsmall cell lung cancer (Yamashita et al, 1996). In addition to their prognostic relevance in primary disease, several proteases have been shown to be positive or negative predictive factors for the efficacy of adjuvant systemic endocrine therapy or chemotherapy in patients with breast cancer. These proteases comprise uPA (Harbeck et al, 2001, 2002a, 2002b; Jänicke et al, 2001), MMP-2 (Talvensaari-Mattila et al, 2001), and several cathepsins (Fernö et al, 1994; Billgren et al, 2000; Harbeck et al, 2001).
For breast cancer patients who received systemic therapy for advanced disease, only three studies are available relating the levels of serine proteases, that is, uPA (Foekens et al, 1995), human kallikrein 3 (PSA) (Foekens et al, 1999), or human kallikrein 10 (Luo et al, 2002) to a poor efficacy of first-line tamoxifen treatment. With respect to the predictive value of serine proteases for response to chemotherapy in advanced breast cancer, no published studies are yet available. Taking the prognostic value and the potential predictive value of serine proteases into account, we hypothesised that tumour-associated PMN-E might be predictive for the type of response to systemic treatment in patients with advanced breast cancer. In order to examine this hypothesis, we measured PMN-E in cytosols of primary breast tumours and correlated those with the type of response to first-line treatment with tamoxifen or chemotherapy in patents with advanced disease. In addition, we have studied the relation between the tumour level of PMN-E and the length of progression-free and postrelapse overall survival.
Materials and methods
Patients and tissues
PMN-E levels were determined in cytosol preparations (as described below) from 463 primary invasive breast tumours collected between 1978 and 1989. Selection of samples was based on the availability of stored cytosol extracts (in liquid nitrogen), which remained after routine oestrogen receptor (ER) and progesterone receptor (PgR) analyses. Inoperable T4 tumours were not included. Our study design was approved by the Medical Ethical Committee of the Erasmus Medical Center, Rotterdam, The Netherlands (♯MEC-02.953). Patient tissues that were sampled after neoadjuvant treatment, or obtained from a biopsy specimen, were excluded. Radiotherapy was given to 366 patients (79%): on the breast/thoracic wall in 259 patients and/or on the axilla in 222 patients, and/or parasternal and/or supraclavicular lymph nodes in 243 patients. T1 tumours (⩽2 cm) were present in 112 patients (24%), T2 tumours (>2–5 cm) in 261 patients (56%), T3 tumours (>5 cm) in 53 patients (11%), and operable T4 tumours in 37 patients (8%). At time of primary tumour removal, 122 patients (26%) had no involved lymph nodes, 117 patients (25%) had 1–3 nodes involved, 208 patients (45%) had >3 nodes involved, and of 16 patients (3%) information on nodal status was missing. Pathological examination was carried out as described previously (Foekens et al, 1989b) and the histological differentiation grade was coded as poor in 279 patients (60%), moderate in 77 patients (17%), well in five patients (1%), and unknown for 102 patients (22%).
Of the 463 patients, 387 received tamoxifen as first-line treatment, and 76 received polychemotherapy as first-line treatment (cyclophosphamide, methotrexate, 5-fluorouracil (CMF), 59 patients; 5-fluorouracil and cyclophosphamide with adriamycin (FAC); or with epirubicin (FEC) in 17 patients). The following inclusion criteria were used for patients who received tamoxifen: patients with advanced disease who were treated with first-line tamoxifen therapy (40 mg day−1) and were not exposed to hormonal treatment at an earlier stage (hormono naive). The median age of these patients at start of treatment for advanced disease was 62 years (range 28–91 years). For the 76 patients who received first-line treatment with CMF, FAC, or FEC for advanced disease, patients were included if previously not exposed to any systemic treatment for advanced disease. The median age of these patients at start of chemotherapy was 53 years (range 31–75 years). The characteristics of the patients who received the different types of systemic treatment with respect to menopausal status at the start of systemic treatment for advanced disease, the first dominant site of disease, the number of patients with metastatic disease (M1 patients) at primary surgery, disease-free interval (DFI) between primary tumour removal and first recurrence, hormone receptor status, and the type and frequency of adjuvant therapy are listed in Table 1. The median follow-up of patients still alive after start of systemic therapy for advanced disease was 54 months (range 9–137 months) in the tamoxifen-treated patients (38 patients still alive), and 39 months (range 7–80 months) in those who received chemotherapy (four patients still alive). On first-line tamoxifen therapy, tumour progression occurred in 385 patients (99%), of whom 256 were subsequently treated with one or more additional hormonal agents (mostly high-dose progestins). To date, after the development of hormonal resistance, 216 patients have received systemic chemotherapy (CMF, 131 patients; FAC or FEC, 72 patients; or other agents, 13 patients). On first-line chemotherapy, tumour progression occurred in 75 patients (99%) during follow-up. Of these patients, 42 were eventually treated with endocrine therapy (tamoxifen in 28 patients, progestins in 14 patients).
All patients were assessed by standard International Union Against Cancer criteria for complete and partial remission (objective response). Patients with no change for >6 months (stable disease) have a postrelapse survival similar to patients with partial remission (Ravdin et al, 1992; Foekens et al, 1994a). Therefore, for overall response, objective response and stable disease were combined.
Assays of PMN-E, ER, PgR, and total protein
Tumour tissues were stored in liquid nitrogen and pulverised in the frozen state with a microdismembrator as recommended by the European Organization for Research and Treatment of Cancer (EORTC) for processing of breast tumour tissue for cytosolic ER and PgR determinations (EORTC Breast Cancer Cooperative Group, 1980). The resulting tissue powder was suspended in EORTC receptor buffer (10 mM dipotassium chloride EDTA, 3 mM sodium azide, 10 mM monothioglycerol, and 10% vv−1 glycerol, pH 7.4). The suspension was centrifuged for 30 min at 100 000 × g to obtain the supernatant fraction (cytosol). ER and PgR levels were determined by ligand binding assay or with enzyme immunoassay as described previously (Foekens et al, 1989a). Cytosol protein was quantified with the Coomassie brilliant blue method (Bio-Rad Laboratories, CA, USA) with human serum albumin as a standard. Taking into account that most of the PMN-E in body fluids or tissue cytosols is complexed with its main antagonist, the α1-proteinase inhibitor, we used a commercial two-site enzyme-linked immunosorbent assay for quantification of total PMN-E levels after adding a surplus of α1-proteinase inhibitor (100 μg ml−1) to each cytosol (Milenia-PMN Elastase, Milenia Biotec, Bad Nauheim, Germany).
Statistics
The strength of the associations of PMN-E with continuous variables was tested with Spearman rank correlation (rs). The strength of the association of PMN-E (used as a continuous variable) with other variables (used as grouping variable) was tested with the nonparametric Wilcoxon rank-sum test or Kruskal–Wallis test, followed by a Wilcoxon-type test for trend across ordered groups where appropriate. The length of progression-free survival was defined as the time from the start of treatment for advanced disease until the start of next treatment because of progressive disease or until the time of intercurrent death. Survival probabilities were calculated by the actuarial method of Kaplan and Meier (1958). The log-rank test was used to test for differences between survival curves. Both univariate and multivariate analyses were performed using the Cox proportional hazards model. The proportionality assumption was investigated using a test based on the Schoenfeld residuals (Grambsch and Therneau, 1994). The residuals were retrieved and a smooth function of time was fitted and then tested whether there was a relation. The likelihood ratio test in the Cox regression models was used to test for differences and interactions. The relation of predictive factors with response to therapy was examined with logistic regression analysis. In our search for the best categorisation of PMN-E, we have used isotonic regression analysis (Barlow et al, 1972; Foekens et al, 1994b) using the rate of overall response to tamoxifen treatment as end point. All computations were done with the STATA statistical package, release 7.0 (STATA Corp., College Station, TX, USA). All P-values are two-sided.
Results
PMN-E levels and patient and tumour characteristics
The levels of PMN-E in all the 463 primary breast tumours analysed ranged from 0.4 to 1667 ng mg−1 protein (median, 6.3 ng mg−1 protein). They were not related with age (rs=−0.04, P=0.41), but were slightly higher in tumours of premenopausal patients (median, 6.7 ng mg−1 protein) compared with those of postmenopausal patients (median, 5.9 ng mg−1 protein) at time of primary surgery (P=0.08). PMN-E levels were negatively related with ER (rs=−0.20, P<0.001) and PgR (rs=−0.19, P<0.001), but were not significantly related with tumour size (P=0.74) or grade (P=0.11), or with the lymph-node status of the patient (P=0.48).
The median level of PMN-E in the tumour cytosols of the 387 patients, who were treated with first-line tamoxifen therapy, was 6.0 ng mg−1 protein (range 0.4–1667 ng mg−1 protein). This is significantly (P=0.03) lower than the median level of 7.1 ng mg−1 protein (range 0.7–426 ng mg−1 protein) that was measured in tumours of the 76 patients who were treated with first-line chemotherapy. The data are consistent with the higher proportion of ER-negative tumours in the latter series of patients and the observed negative relation between the levels of PMN-E and ER.
Univariate analysis for response to treatment in advanced disease
Of the 387 patients who received tamoxifen as first-line treatment for advanced disease, 197 (51%) responded (11 complete remission, 48 partial remission, and 138 stable disease). The median duration of response in these responders was 15 months. Using logistic regression analysis, it was shown that older age and postmenopausal status were associated with a higher rate of response to tamoxifen treatment than younger age and premenopausal status (Table 2). In patients with a disease-free interval less than 1 year (35% response; odds ratio, OR set at 1), the fraction of responding patients was smaller than in patients with a disease-free interval ⩾1 year (57% response, OR=2.47). Adjuvant chemotherapy and first site of relapse were not related to the type of response on tamoxifen treatment. Patients with ER-positive or PgR-positive tumours had a more favourable response rate (OR=3.73 and OR=1.73, respectively) than patients with ER-negative or PgR-negative tumours (OR=1). As expected, the traditional prognostic factors nodal status, and size and grade of the primary tumour were not significantly related with the type of response to tamoxifen in advanced disease, that is, they were no predictive factors. When analysing the relation of continuous tumour PMN-E levels with response, it appeared that there was a trend towards a lower response rate with increasing levels of PMN-E (P=0.07). Using isotonic regression analysis, 20.0 ng mg−1 protein was chosen as cutoff point to classify advanced breast cancer patients as PMN-E-high and PMN-E-low. Compared with the 331 patients with low PMN-E levels (54% response (16% complete and partial remission, 38% stable disease), OR=1), the 56 patients with high PMN-E levels showed a worse rate of response (32% response (11% complete and partial remission, 21% stable disease), OR=0.40; P=0.003).
The median postrelapse survival time after the start of tamoxifen treatment was longer in the 331 patients with low tumour PMN-E levels compared with the 56 patients with high PMN-E levels (25 and 15 months, respectively). However, the median duration of response in the 179 responding patients with low tumour PMN-E levels was not different from that in the 18 responding patients with high PMN-E levels (median 15 and 17 months, respectively). In Cox univariate regression analysis using continuous PMN-E levels, PMN-E was not significantly associated with progression-free survival (P=0.51) or postrelapse survival (P=0.06) when all failures during the total follow-up period were taken into account (385 and 349 events in the analyses of progression-free and postrelapse survival, respectively). However, both in the analysis for postrelapse and progression-free survival, the proportional hazards assumption was violated (P=0.01 and P=0.04, respectively). This was indicative for a time-dependent relation between the level of PMN-E and the survival analyses. Since the median progression-free survival time was 6.7 months and that of postrelapse survival was 23.5 months, we further explored the short-term predictive value of PMN-E for the periods before 6 months in the analysis of progression-free survival (182 events of a total of 385) and before 20 months in the analysis of postrelapse survival (167 events of a total of 349). In these analyses, increasing levels of PMN-E were significantly related with a poor progression-free (P=0.01) and postrelapse survival (P=0.001). Furthermore, the proportional hazards assumption was no longer violated with respective P-values of 0.93 in the analysis of progression-free survival and of 0.64 in the analysis of postrelapse survival.
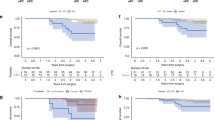
The results of the Kaplan–Meier analysis for progression-free and postrelapse survival in all 387 patients, who received first-line tamoxifen treatment for advanced disease as a function of dichotomised PMN-E status, are shown in Figure 1A and B, respectively. Restricting the analyses to the first 6 months for progression-free survival and to 20 months for postrelapse survival resulted in hazard ratios (HRs) of 2.02 (P<0.001, Figure 1A) and 1.79 (P=0.002, Figure 1B), respectively. In the analyses including all failures over the total follow-up period, the strengths of the relation of PMN-E with postrelapse survival (P=0.06) and progression-free survival (P=0.12) were less and not statistically significant.
Of the 76 patients who received chemotherapy as first-line treatment for advanced disease, 33 (43%) responded (seven complete remission, 14 partial remission, 12 stable disease). In these patients, PMN-E levels, neither when analysed as a continuous nor as a dichotomised variable, were significantly related with the rate of response, duration of response, or the length of progression-free or postrelapse survival.
Multivariate analysis for response to tamoxifen treatment in advanced disease
The independent relation of PMN-E levels with the rate of response to tamoxifen treatment in advanced breast cancer was studied using multivariate logistic regression analysis ( Table 2). High levels of PMN-E were associated with a poor rate of response (OR=0.45, P=0.01). In addition to PMN-E status, premenopausal status, a short DFI, and ER negativity were associated with a poor response rate in the multivariate analysis. In separate multivariate analyses in which PMN-E was added as a dichotomised variable and ER as a continuous variable to the model, the contributions of ER (OR, 1.30; 95% CI, 1.15–1.48; P<0.001) and PMN-E (OR, 0.47; 95% CI, 0.25–0.89; P=0.02) were statistically significant as well. However, when PMN-E was added as a continuous instead of a dichotomised variable to the multivariate model shown in Table 2, its contribution was not statistically significant (P=0.31). Furthermore, there was no statistically significant interaction between categorically added PMN-E and ER with respect to the rate of response to tamoxifen treatment.
Response to tamoxifen treatment in ER subgroups of tumours
We explored the association of PMN-E with the response rate in the clinically important subgroups of ER-positive and ER-negative patients. The predictive value of a high PMN-E level for a lower response rate appeared to be confined to the subgroup of 338 ER-positive patients. Of the 40 patients with a high tumour PMN level, only 14 (35%) responded compared with 171 (57%) of 298 patients with a low PMN-E level (OR, 0.40; 95% CI, 0.20–0.80; P=0.009). In 49 ER-negative patients, the fraction of responding patients was 24% (eight out of 33) and 25% (four out of 16) for those with low or high tumour PMN-E levels, respectively (OR, 1.04; 95% CI, 0.26–4.16; P=0.95).
Discussion
During the past 20 years, the presence of steroid receptors in the primary breast tumour has been the major guide to the physician to treat the patients with endocrine therapy. However, the steroid receptor status of the primary tumour does not fully predict which patient will benefit or fail from endocrine therapy, and many more potential cell biological predictive factors have been studied (reviewed by Klijn et al, 1999, 2002). The expression levels of several serine proteases, such as uPA, human kallikreins 3 and 10 have been reported to be associated with a poor relapse-free and/or overall survival in patients with primary breast cancer. Since the serine protease PMN-E is the only neutral protease that is able to degrade insoluble elastin (Janoff and Schere, 1968; Baugh and Travis, 1976), which is a structural component of breast tissues (Hornebeck et al, 1977), we considered it of interest to study the clinical relevance of PMN-E in breast cancer. Analogous to other serine proteases, the tumour level of PMN-E was also shown to be able to discriminate between primary breast cancer patients with high and low risk of recurrence (Yamashita et al, 1994, 1995b), irrespective of whether adjuvant tamoxifen treatment was given (Yamashita et al, 1995a). Yet, from the latter study, no conclusions can be drawn with respect to a possible relation between PMN-E and efficacy of tamoxifen therapy. Recently we showed that primary breast cancer patients with high tumour levels of uPA and its inhibitor PAI-1, being classified as high risk for recurrence, experienced an enhanced benefit from adjuvant chemotherapy (Harbeck et al, 2002a, 2002b). For patients with advanced breast cancer, a very limited number of studies (all from our laboratory) addressing the relation of serine proteases with the efficacy of systemic treatment are available. In this respect, we showed that high tumour levels of uPA (Foekens et al, 1995), kallikrein 3 (Foekens et al, 1999), or kallikrein 10 (Luo et al, 2002) were significantly associated with a poor rate of response to tamoxifen therapy. In the present study, we investigated the predictive value of PMN-E for the efficacy of tamoxifen and chemotherapy in patients with advanced breast cancer. The direct measurable effect of the therapy on the size of relapse or the development of new relapses was considered the main end point of the study. This study is different from those performed in the adjuvant setting in which all intentionally cured primary breast cancer patients are evaluated with the development of a relapse as end point. In the case of nonrandomised patients, the occurrence of a relapse does not necessarily reflect an association of the marker studied with the efficacy of adjuvant treatment. Furthermore, response as in objective response and progressive disease cannot be studied because by definition there is no measurable tumour in the adjuvant setting. In the present study analysing the predictive value of PMN-E in the advanced setting, we corrected for traditional prognostic and predictive factors, including disease-free interval, in the multivariable logistic regression analysis for response to tamoxifen treatment. Thus, the possibility that the observed predictive value of PMN-E partly reflects its prognostic value is minimal excluded.
So far, the reason for the observed negative relations between the levels of PMN-E and ER and PgR, which we also showed in a larger series of 1143 primary breast cancer patients in which we studied the prognostic value of PMN-E (Foekens et al, 2003), is not clear. It may be explained by an inhibition in elastase activity by oestradiol and progesterone that has been observed in breast cancer cells grown in vitro (Kao and Stern, 1986). On the other hand, the amount of immunoreactive PMN-E secreted by breast cancer cells into culture media was not affected by oestradiol, which suggested that PMN-E synthesis is oestrogen independent (Yamashita et al, 1994). The only other laboratory that studied PMN-E expression in human breast cancer tissues reported a nonsignificant trend towards a negative correlation between PMN-E levels and those of ER and PgR in a small series of 62 tumours (Yamashita et al, 1994). In their subsequent study involving 184 tumours of node-negative patients (Yamashita et al, 1995a), no significant relation between PMN-E and ER or PgR was found. However, the statistical method used was different from that of our study in which we used Spearman rank correlation that is better suited for evaluating correlations between continuous variables. A further difference is that we have analysed PMN-E levels in cytosolic tissue extracts, whereas Yamashita et al (1995a) used Triton X-100 extracts.
In the present study, high tumour levels of PMN-E were associated with a poor efficacy of tamoxifen treatment in patients with advanced disease, independent of the traditional predictive factors menopausal status, disease-free interval, and hormone receptor status. From the exploratory subgroup analyses, it appeared that the association of PMN-E with the type of response to tamoxifen treatment was exclusively present in patients with ER-positive tumours. The association of PMN-E with the lengths of progression-free and postrelapse survival was only of statistical significance during short-term follow-up. These analyses were indicated since by taking all the failures during the total follow-up period into account, the proportional hazards assumption, on which the Cox regression analysis is based, was violated. Such a time-dependent relation between cell biological factors and (relapse-free) survival in primary breast cancer has recently been observed for PMN-E (Foekens et al, 2003), as well as for clinical and other biological factors like uPA (Yoshimoto et al, 1993; Schmitt et al, 1997b; Hilsenbeck et al, 1998). In the present study, no relation between the tumour PMN-E level and the efficacy of first-line chemotherapy in patients with advanced breast cancer was seen, suggesting that possible interfering effects of PMN-E are overruled by the chemotherapy regimens applied.
The underlying mechanisms explaining why the primary tumour level of PMN-E is associated with the efficacy of tamoxifen therapy in advanced disease is unclear. In addition to its described role in tumour cell invasion and metastasis, the serine protease PMN-E may, similar as has been suggested for uPA for human ovarian carcinoma cells (Fischer et al, 1998) and breast cancer cells (Foekens et al, 1995), provoke cell proliferation via enzymatic activation of several growth factor (receptor) pathways. In this respect, the ability of elastase to cleave or activate several growth factors or receptors, such as EGF and EGF receptor (Di Camillo et al, 2002), IL-2 and IL-6 receptor (Bank et al, 1999), stromal cell-derived factor-1 (Valenzuela-Fernandez et al, 2002), supports such a local elastase-directed growth interfering mechanism.
In summary, our study suggests that a high tumour level of PMN-E is associated with a poor rate of response to tamoxifen therapy, and a short progression-free and postrelapse survival. Thus, patients with low tumour levels of PMN-E may respond better to tamoxifen therapy. In contrast, since the levels of PMN-E do not affect the effectiveness of chemotherapy, patients with high tumour levels of PMN-E might benefit from chemotherapy rather that from endocrine therapy. The present pilot study is the first to report the relation between the tumour level of PMN-E and the efficacy of systemic therapy in patients with advanced breast cancer. However, confirmatory studies are needed before any conclusions can be drawn regarding suggestions to be made for the most promising systemic treatment based on the tumour level of PMN-E.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Andreasen PA, Kjøller L, Christensen L, Duffy MJ (1997) The urokinase-type plasminogen activator system in cancer metastasis: a review. Int J Cancer 72: 1–22
Bank U, Reinhold D, Schneemilch C, Kunz D, Synowitz HJ, Ansorge S (1999) Selective proteolytic cleavage of IL-2 receptor and IL-6 receptor ligand binding chains by neutrophil-derived serine proteases at foci of inflammation. J Interferon Cytokine Res 19: 1277–1287
Barlow RE, Bartholomew DJ, Bremner JM, Brunck HD (1972) Statistical Inference Under Order Restrictions. New York: John Wiley & Sons, Inc.
Barrett AJ (1981) Leukocyte elastase. Methods Enzymol 80: 581–588
Baugh RJ, Travis J (1976) Human leukocyte elastase: rapid isolation and characterization. Biochemistry 15: 836–841
Billgren AM, Rutqvist LE, Johansson H, Hägerström T, Skoog L (2000) The role of cathepsin D and PAI-1 in primary invasive breast cancer as prognosticators and predictors of treatment benefit with adjuvant tamoxifen. Eur J Cancer 36: 1374–1380
Di Camillo SJ, Carreras I, Panchenko MV, Stone PJ, Nugant MA, Foster JA, Panchenko MP (2002) Elastase-released epidermal growth factor recruits epidermal growth factor receptor and extracellular signal-regulated kinases to down-regulate tropoelastin mRNA in lung fibroblasts. J Biol Chem 277: 18938–18946
Duffy MJ, Maguire TM, Hill A, McDermott E, O'Higgins N (2000) Metalloproteinases: a role in breast carcinogenesis, invasion and metastasis. Breast Cancer Res 2: 252–257
EORTC Breast Cancer Cooperative Group (1980) Revision of the standards for the assessment of hormone receptors in human breast cancer; report of the second E.O.R.T.C. Workshop, held on 16–17 March, 1979, in The Netherlands Cancer Institute. Eur J Cancer 16: 1513–1515
Fernö M, Baldetorp B, Borg Å, Brouillet J-P, Olsson H, Rochefort H, Sellberg G, Sigurdsson H, Killander for the South Sweden Breast Cancer Group (1994) Cathepsin D, both a prognostic factor and a predictive factor for the effect of adjuvant tamoxifen in breast cancer. Eur J Cancer 14: 2042–2048
Fischer K, Lutz V, Wilhelm O, Schmitt M, Graeff H, Heiss P, Nishiguchi T, Harbeck N, Kessler H, Luther T, Magdolen V, Reuning U (1998) Urokinase induces proliferation of human ovarian cancer cells: characterization of structural elements required for growth factor function. FEBS Lett 438: 101–105
Foekens JA, Diamandis EP, Yu H, Look ME, Meijer-van Gelder ME, van Putten WLJ, Klijn JGM (1999) Expression of prostate-specific antigen (PSA) correlates with poor response to tamoxifen therapy in recurrent breast cancer. Br J Cancer 79: 888–894
Foekens JA, Look MP, Peters HA, van Putten WLJ, Portengen H, Klijn JGM (1995) Urokinase-type plasminogen activator and its inhibitor PAI-1: predictors of poor response to tamoxifen therapy in recurrent breast cancer. J Natl Cancer Inst 87: 751–756
Foekens JA, Portengen H, van Putten WLJ, Peters HA, Krijnen HLJM, Alexieva-Figusch J, Klijn JGM (1989a) Prognostic value of estrogen and progesterone receptors measured by enzyme immunoassays in human breast tumour cytosols. Cancer Res 49: 5823–5828
Foekens JA, Portengen H, van Putten WLJ, Thirion B, Bontenbal M, Alexieva-Figusch J, Klijn JGM (1994a) Relation of PS2 with response to tamoxifen therapy in patients with recurrent breast cancer. Br J Cancer 70: 1217–1223
Foekens JA, Portengen H, van Putten WLJ, Trapman AMAC, Reubi JC, Alexieva-Figusch J, Klijn JGM (1989b) Prognostic value of receptors for insulin-like growth factor-1, somatostatin, and epidermal growth factor in human breast cancer. Cancer Res 49: 7002–7009
Foekens JA, Ries C, Look MP, Gippner-Steppert C, Klijn JGM, Jochum M (2003) The prognostic value of polymorphonuclear leukocyte elastase in patients with primary breast cancer. Cancer Res 63: 337–341
Foekens JA, Schmitt M, van Putten WLJ, Peters HA, Kramer MD, Jänicke F, Klijn JGM (1994b) Plasminogen activator inhibitor-1 and prognosis in primary breast cancer. J Clin Oncol 12: 1648–1658
Grambsch PM, Therneau TM (1994) Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 81: 515–526
Gramse M, Egbring R, Havemann K (1984) α2-plasmin inhibitor inactivation by granulocyte elastase. Hoppe-Seyler's Z Physiol Chem 356: 19–26
Harbeck N, Alt U, Berger U, Krüger A, Thomssen C, Jänicke F, Höfler H, Kates RE, Schmitt M (2001) Prognostic impact of proteolytic factors (urokinase-type plasminogen activator, plasminogen activator inhibitor 1, and cathepsins B, D, and L) in primary breast cancer reflects effects of adjuvant systemic therapy. Clin Cancer Res 7: 2757–2764
Harbeck N, Kates RE, Look MP, Meijer-van Gelder ME, Klijn JGM, Krüger A, Kiechle M, Jänicke F, Schmitt M, Foekens JA (2002a) Enhanced benefit from adjuvant chemotherapy in breast cancer patients classified high-risk according to uPA and PAI-1 (n=3424). Cancer Res 62: 4617–4622
Harbeck N, Kates RE, Schmitt M (2002b) Clinical relevance of invasion factors urokinase-type plasminogen activator and plasminogen activator inhibitor type 1 for individualised therapy decisions in primary breast cancer is greatest when used in combination. J Clin Oncol 20: 1000–1007
Hilsenbeck SG, Ravdin PM, de Moor CA, Chamness GC, Osborne CK, Clark GM (1998) Time-dependence of hazard ratios for prognostic factors in primary breast cancer. Breast Cancer Res Treatm 52: 227–237
Hornebeck W, Derouette JC, Brechemier D, Adnett JJ, Robert L (1977) Elastogenesis and elastinolytic activity in human breast cancer. Biomedicine 26: 48–52
Jackson JR, Seed MP, Kircher CH, Willoughby DA, Winkler JD (1997) The codependence of angiogenesis and chronic inflammation. FASEB J 11: 457–465
Jänicke F, Prechtl A, Thomssen C, Harbeck N, Meisner C, Untch M, Sweep CGJ, Selbman H–K, Graeff H, Schmitt M (2001) Randomized adjuvant chemotherapy trial in high-risk, lymph node-negative breast cancer patients identified by urokinase-type plasminogen activator and plasminogen activator inhibitor type 1. J Natl Cancer Inst 93: 913–920
Janoff A, Schere J (1968) Elastolytic activity in granules of human polymorphonuclear leukocytes. J Exp Med 128: 1137–1156
Kao RT, Stern R (1986) Elastases in human breast carcinoma cells. Cancer Res 46: 1355–1358
Kaplan EL, Meier P (1958) Non-parametric estimation of incomplete observations. J Am Stat Assoc 53: 457–481
Klijn JGM, Berns EMJJ, Foekens JA (1999) Prognostic and predictive factors in breast cancer. In Contemporary Endocrinology: Endocrinology of Breast Cancer. Manni A (ed) pp 205–220. Totowa, NJ, USA: Humana Press Inc
Klijn JGM, Berns EMJJ, Foekens JA (2002) Prognostic and predictive factors and targets for therapy in breast cancer. In Breast Cancer: Prognosis, Treatment and Prevention. Pasqualini JR (ed) pp 93–124. New York, USA: Marcel Dekker Inc
Lee AH, Happerfield LC, Borrow LG, Mills PR (1997) Angiogenesis and inflammation in ductal carcinoma in situ of the breast. J Pathol 181: 200–206
Levin EG, Santell L (1987) Association of a plasminogen activator inhibitor (PAI-1) with the growth substratum and membrane of human endothelial cells. J Cell Biol 105: 2543–2549
Look MP, Foekens JA (1999) Clinical relevance of the urokinase plasminogen activator system in breast cancer. APMIS 107: 150–159
Luo L-Y, Diamandis EP, Look MP, Soosaipillai AP, Foekens JA (2002) Higher expression of human kallikrein 10 in breast cancer tissue predicts tamoxifen resistance. Br J Cancer 86: 1790–1796
Machovich R, Owen WG (1990) The elastase-mediated pathway of fibrinolysis. Blood Coagul Fibrinol 1: 79–90
Mainardi CL, Dixit SN, Kang AH (1980) Degradation of type IV (basement membrane) collagen by a proteinase isolated from human polymorphonuclear leukocyte granules. J Biol Chem 255: 5435–5441
McDonald JA, Kelley DG (1980) Degradation of fibronectin by human leukocyte elastase: release of biologically active fragments. J Biol Chem 255: 8848–8858
Mignatti P, Robbins E, Rifkin DB (1986) Tumor invasion through the human amniotic membrane: requirement for a proteinase cascade. Cell 47: 487–498
Nelson AR, Fingleton B, Rothenberg ML, Matrisian LM (2000) Matrix metalloproteinases: biological activity and clinical implications. J Clin Oncol 18: 1135–1149
Nozawa F, Hirota M, Okabe A, Shibata M, Iwumura T, Haga Y, Ogawa M (2000) Elastase activity enhances the adhesion of neutrophil and cancer cells to vascular endothelial cells. J Surg Res 94: 153–158
Ravdin PM, Green S, Dorr TM, McGuire WL, Fabian C, Pugh RP, Carter RD, Rivkin SE, Borst JR, Belt J, Metch B, Osborne CK (1992) Prognostic relevance of progesterone receptor levels in estrogen receptor-positive patients with metastatic breast cancer treated with tamoxifen: results of a prospective Southwest Oncology Group Study. J Clin Oncol 10: 1284–1291
Schmitt M, Harbeck N, Thomssen C, Wilhelm O, Magdolen V, Reuning U, Ulm K, Höfler H, Jänicke F, Graeff H (1997a) Clinical impact of the plasminogen activation system in tumor invasion and metastasis: prognostic relevance and target for therapy. Thromb Haemost 78: 285–296
Schmitt M, Thomssen C, Ulm K, Seiderer A, Harbeck N, Höfler H, Jänicke F, Graeff H (1997b) Time-varying prognostic impact of tumour biological factors urokinase (uPA), PAI-1 and steroid hormone receptor status in primary breast cancer. Br J Cancer 76: 306–311
Scholl SM, Pallud C, Beuvon P, Hacène K, Stanley ER, Rohrschneider L, Tang R, Pouillart P, Lidereau R (1994) Anti-colony-stimulating factor-1 antibody staining in primary breast adenocarcinoma correlates with marked inflammatory cell infiltrates and prognosis. J Natl Cancer Inst 86: 120–126
Shamamian P, Pocock BJ, Schwartz JD, Monea S, Chuang N, Whiting D, Marcus SG, Golloway AC, Mignatti P (2000) Neurophil-derived serine proteases enhance membrane type-1 matrix metalloproteinase-dependent tumor cell invasion. Surgery 127: 142–147
Shamamian P, Schwartz JD, Pocock BJ, Monea S, Whiting D, Marcus SG, Mignatti (2001) Activation of progelatinase A (MMP-2) by neutrophil elastase, cathepsin G, and proteinase-3: a role for inflammatory cells in tumor invasion and angiogenesis. J Cell Physiol 189: 197–206
Talvensaari-Matilla A, Pääkkö P, Blanco-Sequieros G, Turpeenniemi-Hujanen T (2001) Matrix metalloproteinase-2 (MMP-2) is associated with the risk for a relapse in postmenopausal patients with node-positive breast carcinoma treated with antiestrogen adjuvant therapy. Breast Cancer Res Treatm 65: 55–61
Valenzuela-Fernandez A, Planchenault T, Baleux F, Starpoli I, Le-Barillec K, Ludec D, Delaunay F, Virelizier JL, Chingard M, Pidard D, Arenzana-Seisdedos F (2002) leukocyte elastase negatively regulates stromal cell-derived factor-1 (SDF-1)/CXCR4 binding and functions by amino-terminal processing of SDF-1 and CXCR4. J Biol Chem 277: 15677–15689
Wu K, Urano T, Ihara H, Takada Y, Fujie M, Shikimori M, Hashimoto K, Takada A (1995) The cleavage and inactivation of plasminogen activator inhibitor type 1 by neutrophil elastase: the evaluation of its physiologic relevance in fibrinolysis. Blood 86: 1056–1061
Yamashita J-I, Ogawa M, Ikei S, Omachi H, Yamashita S-I, Saishoji T, Nomura K, Sato H (1994) Production of immunoreactive polymorphonuclear leukocyte elastase in human breast cancer cells: possible role of polymorphonuclear leukocyte in the progression of human breast cancer. Br J Cancer 69: 72–76
Yamashita J-I, Ogawa M, Sato K (1995a) Prognostic significance of three novel biological factors in a clinical trial of adjuvant therapy for node-negative breast cancer. Surgery 117: 601–608
Yamashita J-I, Ogawa M, Shirakusa T (1995b) Free-form neutrophil elastase is an independent marker predicting recurrence in primary breast cancer. J Leuk Biol 57: 375–378
Yamashita J-I, Toshiro K, Yoneda S, Kawahara K, Shirakusa T (1996) Local increase in polymorphonuclear leukocyte elastase is associated with tumor invasiveness in non-small cell lung cancer. Chest 109: 1328–1334
Yoshimoto M, Sakamoto G, Ohashi Y (1993) Time dependency of the influence of prognostic factors on relapse in breast cancer. Cancer 72: 2993–3001
Acknowledgements
We gratefully express our thanks to Ms ME Meijer-van Gelder (Erasmus MC, Rotterdam) for the collection of clinical follow-up data, and the surgeons, pathologists, and internists of the St Clara Hospital, Ikazia Hospital, and St Franciscus Gasthuis at Rotterdam, and the Ruwaard van Putten Hospital at Spijkenisse, for the supply of tumour tissues and/or assisting us in the collection of the clinical follow-up data. The valuable technical assistance of Mr T Pitsch (LMU Munich) measuring PMN-E is highly acknowledged. This study is supported by Grant SFB 469 (B1), Ludwig-Maximilians-University, Munich, Germany, and by Grant DDHK 2000-2256 of the Dutch Cancer Society, Amsterdam, The Netherlands.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Foekens, J., Ries, C., Look, M. et al. Elevated expression of polymorphonuclear leukocyte elastase in breast cancer tissue is associated with tamoxifen failure in patients with advanced disease. Br J Cancer 88, 1084–1090 (2003). https://doi.org/10.1038/sj.bjc.6600813
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6600813
Keywords
This article is cited by
-
Acute inflammation induced by the biopsy of mouse mammary tumors promotes the development of metastasis
Breast Cancer Research and Treatment (2013)