Abstract
Background
Platelets support tumour progression. However, their prognostic significance and relation to circulating tumour cells (CTCs) in operable breast cancer (BrCa) are still scarcely known and, thus, merit further investigation.
Methods
Preoperative platelet counts (PCs) were compared with clinical data, CTCs, 65 serum cytokines and 770 immune-related transcripts obtained using the NanoString technology.
Results
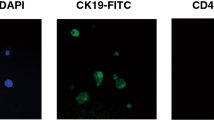
High normal PC (hPC; defined by the 75th centile cut-off) correlated with an increased number of lymph node metastases and mesenchymal CTCs in the 70 operable BrCa patients. Patients with hPC and CTC presence revealed the shortest overall survival compared to those with no CTC/any PC or even CTC/normal PC. Adverse prognostic impact of hPC was observed only in the luminal subtype, when 247 BrCa patients were analysed. hPC correlated with high content of intratumoural stroma, specifically its phenotype related to CD8+ T and resting mast cells, and an increased concentration of cytokines related to platelet activation or even production in bone marrow (i.e. APRIL, ENA78/CXCL5, HGF, IL16, IL17a, MDC/CCL22, MCP3, MMP1 and SCF).
Conclusions
Preoperative platelets evaluated alone and in combination with CTCs have prognostic potential in non-metastatic BrCa and define patients at the highest risk of disease progression, putatively benefiting from anti-platelet therapy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data that support the findings of this work are available from the corresponding author upon request. Immune-related transcriptome data are available at NCBI GEO under accession number GSE180186.
References
Leblanc R, Peyruchaud O. Metastasis: new functional implications of platelets and megakaryocytes. Blood. 2016;128:24–31.
Heeke S, Mograbi B, Alix-Panabières C, Hofman P. Never travel alone: the crosstalk of circulating tumor cells and the blood microenvironment. Cells. 2019;8:714.
Bendas G, Borsig L. Cancer cell adhesion and metastasis: selectins, integrins, and the inhibitory potential of heparins. Int J Cell Biol. 2012;2012:676731.
Coupland LA, Chong BH, Parish CR. Platelets and P-selectin control tumor cell metastasis in an organ-specific manner and independently of NK cells. Cancer Res. 2012;72:4662–71.
Mitrugno A, Pelz K, Sears R, McCarty O. Abstract B62: Role of the blood microenvironment in the upregulation of oncoproteins in circulating pancreatic cancer cells. Cancer Res. 2017;77:B62.
Lou X-L, Sun J, Gong S-Q, Yu X-F, Gong R, Deng H. Interaction between circulating cancer cells and platelets: clinical implication. Chin J Cancer Res. 2015;27:450.
Labelle M, Begum S, Hynes RO. Direct signaling between platelets and cancer cells induces an epithelial-mesenchymal-like transition and promotes metastasis. Cancer Cell. 2011;20:576–90.
Labelle M, Begum S, Hynes RO. Platelets guide the formation of early metastatic niches. Proc Natl Acad Sci USA. 2014;111:E3053–E3061.
Bednarz-Knoll N, Alix-Panabières C, Pantel K. Plasticity of disseminating cancer cells in patients with epithelial malignancies. Cancer Metastasis Rev. 2012;31:673–87.
Rao X-D, Zhang H, Xu Z-S, Cheng H, Shen W, Wang X-P. Poor prognostic role of the pretreatment platelet counts in colorectal cancer: a meta-analysis. Medicine. 2018;97:e10831.
Grilz E, Posch F, Königsbrügge O, Schwarzinger I, Lang IM, Marosi C, et al. Association of platelet-to-lymphocyte ratio and neutrophil-to-lymphocyte ratio with the risk of thromboembolism and mortality in patients with cancer. Thrombosis Haemost. 2018;118:1875–84.
Li L, Wang J, Meng S, Li Z, Huang Z, Sun J, et al. Peripheral blood leukocytes and platelets serve as prognostic factors in breast cancer. Cancer Biother Radiopharm. 2020;36:167–73.
Krenn-Pilko S, Langsenlehner U, Thurner EM, Stojakovic T, Pichler M, Gerger A, et al. The elevated preoperative platelet-to-lymphocyte ratio predicts poor prognosis in breast cancer patients. Br J Cancer. 2014;110:2524–30.
Zhang M, Huang X, Song Y, Gao P, Sun J, Wang Z. High platelet-to-lymphocyte ratio predicts poor prognosis and clinicopathological characteristics in patients with breast cancer: a meta-analysis. BioMed Res Int. 2017;2017:9503025.
Vernieri C, Mennitto A, Prisciandaro M, Huber V, Milano M, Rinaldi L, et al. The neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios predict efficacy of platinum-based chemotherapy in patients with metastatic triple negative breast cancer. Sci Rep. 2018;8:1–10.
Bruno A, Dovizio M, Tacconelli S, Contursi A, Ballerini P, Patrignani P. Antithrombotic agents and cancer. Cancers. 2018;10:253.
Jing L, Qu H, Wu D, Zhu C, Yang Y, Jin X, et al. Platelet-camouflaged nanococktail: Simultaneous inhibition of drug-resistant tumor growth and metastasis via a cancer cells and tumor vasculature dual-targeting strategy. Theranostics. 2018;8:2683.
Ponert JM, Schwarz S, Haschemi R, Müller J, Pötzsch B, Bendas G, et al. The mechanisms how heparin affects the tumor cell induced VEGF and chemokine release from platelets to attenuate the early metastatic niche formation. PLoS ONE. 2018;13:e0191303.
Papa AL, Jiang A, Korin N, Chen MB, Langan ET, Waterhouse A, et al. Platelet decoys inhibit thrombosis and prevent metastatic tumor formation in preclinical models. Sci Transl Med. 2019;11:eaau5898.
Vilsmaier T, Rack B, König A, Friese K, Janni W, Jeschke U, et al. Influence of circulating tumour cells on production of IL-1alpha, IL-1beta and IL-12 in sera of patients with primary diagnosis of breast cancer before treatment. Anticancer Res. 2016;36:5227–36.
Divella R, Daniele A, Abbate I, Bellizzi A, Savino E, Simone G, et al. The presence of clustered circulating tumor cells (CTCs) and circulating cytokines define an aggressive phenotype in metastatic colorectal cancer. Cancer Causes Control. 2014;25:1531–41.
Mego M, Cholujova D, Minarik G, Sedlackova T, Gronesova P, Karaba M, et al. CXCR4-SDF-1 interaction potentially mediates trafficking of circulating tumor cells in primary breast cancer. BMC Cancer. 2016;16:1–9.
Smolkova B, Mego M, Horvathova Kajabova V, Cierna Z, Danihel L, Sedlackova T, et al. Expression of SOCS1 and CXCL12 proteins in primary breast cancer are associated with presence of circulating tumor cells in peripheral blood. Transl Oncol. 2016;9:184–90.
Lippitz BE. Cytokine patterns in patients with cancer: a systematic review. Lancet Oncol. 2013;14:e218–e228.
Setrerrahmane S, Xu H. Tumor-related interleukins: old validated targets for new anti-cancer drug development. Mol Cancer. 2017;16:1–17.
Markiewicz A, Wełnicka-Jaśkiewicz M, Seroczyńska B, Skokowski J, Majewska H, Szade J, et al. Epithelial-mesenchymal transition markers in lymph node metastases and primary breast tumors-relation to dissemination and proliferation. Am J Transl Res. 2014;6:793.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12:1495–9.
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM. REporting recommendations for tumor MARKer prognostic studies (REMARK). Breast Cancer Res Treat. 2006;100:229–35.
Newman AM, Steen CB, Liu CL, Gentles AJ, Chaudhuri AA, Scherer F, et al. Determining cell type abundance and expression from bulk tissues with digital cytometry. Nat Biotechnol. 2019;37:773–82.
Popeda M, Stokowy T, Bednarz-Knoll N, Jurek A, Niemira M, Bielska A, et al. NF-kappa B signaling-related signatures are connected with the mesenchymal phenotype of circulating tumor cells in non-metastatic breast cancer. Cancers. 2019;11:1961.
R Core Team. R: A language and environment for statistical computing. 2013. https://www.R-project.org/.
Blair P, Flaumenhaft R. Platelet alpha-granules: basic biology and clinical correlates. Blood Rev. 2009;23:177–89.
Sandberg WJ, Otterdal K, Gullestad L, Halvorsen B, Ragnarsson A, Frøland SS, et al. The tumour necrosis factor superfamily ligand APRIL (TNFSF13) is released upon platelet activation and expressed in atherosclerosis. Thrombosis Haemost. 2009;102:704–10.
Ankus E, Price SJ, Ukoumunne OC, Hamilton W, Bailey SE. Cancer incidence in patients with a high normal platelet count: a cohort study using primary care data. Fam Pract. 2018;35:671–5.
Rachidi S, Wallace K, Day TA, Alberg AJ, Li Z. Lower circulating platelet counts and antiplatelet therapy independently predict better outcomes in patients with head and neck squamous cell carcinoma. J Hematol Oncol. 2014;7:1–7.
Balduini CL, Noris P. Platelet count and aging. Haematologica. 2014;99:953.
Khetawat G, Faraday N, Nealen ML, Vijayan KV, Bolton E, Noga SJ, et al. Human megakaryocytes and platelets contain the estrogen receptor beta and androgen receptor (AR): testosterone regulates AR expression. Blood. 2000;95:2289–96.
Jayachandran M, Miller VM. Human platelets contain estrogen receptor alpha, caveolin-1 and estrogen receptor associated proteins. Platelets. 2003;14:75–81.
Gear AR, Camerini D. Platelet chemokines and chemokine receptors: linking hemostasis, inflammation, and host defense. Microcirculation. 2003;10:335–50.
Uzan G, Prandini M-H, Rosa J-P, Berthier R. Hematopoietic differentiation of embryonic stem cells: an in vitro model to study gene regulation during megakaryocytopoiesis. Stem Cells. 1996;14:194–9.
Bonci D, Hahne M, Felli N, Peschle C, De Maria R. Potential role of APRIL as autocrine growth factor for megakaryocytopoiesis. Blood. 2004;104:3169–72.
Avraham H, Vannier E, Cowley S, Jiang SX, Chi S, Dinarello CA, et al. Effects of the stem cell factor, c-kit ligand, on human megakaryocytic cells. Blood. 1992;79:365–71.
Tan W, Liu B, Barsoum A, Huang W, Kolls JK, Schwarzenberger P. Requirement of TPO/c-mpl for IL-17A-induced granulopoiesis and megakaryopoiesis. J Leukoc Biol. 2013;94:1303–8.
Varricchi G, Galdiero MR, Loffredo S, Marone G, Iannone R, Marone G, et al. Are mast cells MASTers in cancer? Front Immunol. 2017;8:424.
Tu J-F, Pan H-Y, Ying X-H, Lou J, Ji J-S, Zou H. Mast cells comprise the major of interleukin 17-producing cells and predict a poor prognosis in hepatocellular carcinoma. Medicine. 2016;95:e3220.
Srenathan U, Steel K, Taams LS. IL-17+ CD8+ T cells: differentiation, phenotype and role in inflammatory disease. Immunol Lett. 2016;178:20–26.
Acknowledgements
We thank all patients who agreed to donate blood for this research. We would like to acknowledge Peter Grešner for providing statistics consultation within the services of the Centre of Biostatistics and Bioinformatics Analysis located at the Medical University of Gdańsk, Poland, working as part of “Excellence Initiative — Research University” (grant no. MNiSW 07/IDUB/2019/94).
Funding
This research was funded by the National Science Centre, grant number 2016/22/E/NZ4/00664 and the National Centre for Research and Development, grant number WPC/33/HESCAP/2018.
Author information
Authors and Affiliations
Contributions
Conceptualisation, NB-K and AJZ; methodology, NB-K, TK, JSz, DS and JL; formal analysis, NB-K and MP; investigation, NB-K, TK, JSz, MP, AM, DS and JL; resources, BK, KP, LK, JS and AJZ; data curation, NB-K and MP; writing — original draft preparation, NB-K and AJZ.; writing — review and editing, all authors; visualisation, NB-K and MP; supervision, NB-K and AJZ; project administration, AJZ; funding acquisition, AJZ.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Primary tumour samples and blood samples were collected from the patients according to a standard protocol approved by the Medical University of Gdansk ethics committee and upon signing an informed consent. This study was performed in accordance with the tenets of the Declaration of Helsinki.
Consent for publication
All informed consent was obtained. This report does not contain any individual person’s information.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Bednarz-Knoll, N., Popęda, M., Kryczka, T. et al. Higher platelet counts correlate to tumour progression and can be induced by intratumoural stroma in non-metastatic breast carcinomas. Br J Cancer 126, 464–471 (2022). https://doi.org/10.1038/s41416-021-01647-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-021-01647-9