Abstract
Gastrin is a gastrointestinal peptide that possesses potent trophic properties on both normal and neoplastic cells of gastrointestinal origin. Previous studies have indicated that chronic hypergastrinaemia increases the risk of colorectal cancer and cancer growth and that interruption of the effects of gastrin could be a potential target in the treatment of colorectal cancer. Here we demonstrate that gastrin leads to a dose-dependent increase in colon cancer cell proliferation and tumour growth in vitro and in vivo, and that this increment is progressively reversed by pretreatment with the cyclo-oxygenase-2 inhibitor NS-398. Gastrin was able to induce cyclo-oxygenase-2 protein expression, as well as the synthesis of prostaglandin E2, the major product of cyclo-oxygenase. Moreover, gastrin leads to approximately a two-fold induction of cyclo-oxygenase-2 promoter activity in transiently transfected cells. The results of these studies demonstrate that cyclo-oxygenase-2 appears to represent one of the downstream targets of gastrin and that selective cyclo-oxygenase-2 inhibition is capable of reversing the trophic properties of gastrin and presumably might prevent the growth of colorectal cancer induced by hypergastrinaemia.
Similar content being viewed by others
Main
The polypeptide hormone gastrin was identified nearly 100 years ago, and its role in the physiology of gastric acid secretion is well-established (Modlin et al, 1997). Another biological property attributed to gastrin is its trophic effect on gastrointestinal (GI) mucosa, including its role in the pathogenesis of GI carcinogenesis (Koh et al, 1999; Stepan et al, 1999; Koh and Chen, 2000). Previous epidemiological studies have indicated that chronic hypergastrinaemia constitutes a risk factor for the development of colorectal cancer (Hakanson et al, 1986; Sundler et al, 1986; Wolfe, 1992; Lamberts et al, 1999; Singh et al, 2000; Watson and Smith, 2001). Significant hypergastrinaemia occurs in association with a number of clinical conditions, including pernicious anaemia and Zollinger-Ellison syndrome and following the development of potent acid suppression in response to the administration of proton pump inhibitors (Klingensmith et al, 1999). The increased incidence of colorectal cancer in hypergastrinaemic patients appears to occur as a result of an increased rate of proliferation of normal colonic epithelium, thus increasing the chance of sporadic mutations. Hypergastrinaemia may also enhance the proliferation and progression of colorectal adenomas (Thorburn et al, 1998; Watson and Smith, 2001).
Epidemiological studies have demonstrated a 40–50% reduction in mortality from colorectal cancer in individuals taking nonsteroidal anti-inflammatory drugs (NSAIDs), which appears to reduce the risk of colorectal cancer (CRC) by inhibiting cyclo-oxygenase (COX), a key enzyme involved in the metabolic conversion of arachidonic acid to prostaglandins (Giovannucci et al, 1994; Giardiello et al, 1995). Numerous studies have shown that the expression of COX-2, one of the two isoforms of COX, is increased significantly in colonic neoplasms compared with normal colonic mucosa, and that COX-2 plays an integral role in colon cancer tumorigenesis and proliferation (Sheng et al, 1997; Barnes et al, 1998; Barnes and Lee, 1998; Sawaoka et al, 1998; Tsujii et al, 1998). However, the cellular and molecular mechanisms governing any possible relationship between gastrin and COX during GI tumour growth have not been elucidated. The purpose of this study was to examine whether COX-2 inhibition is able to reverse the trophic properities of gastrin in CRC.
Materials and methods
Cell culture
MC-26 cells, a transplantable mouse colon cancer cell line that possesses both COX-2 and functional gastrin receptors (Singh et al, 1986), were obtained from Dr KK Tanabe (Boston, MA, USA). MC-26 cells were maintained in Dulbecco's Modified Eagle Media (DMEM; Life Technologies, Inc, Gaithersburg, MD, USA) supplemented with 10% fetal calf serum and antibiotics (100 U ml−1 penicillin and 100 μg ml−1 streptomycin) at 37°C in a humidified atmosphere of 95% air per 5% CO2.
Proliferation studies
DNA synthesis was estimated by the measurement of [3H]thymidine incorporation into cellular DNA. Cells (100 000 ml−1) were seeded onto 12- or 24-well plates and allowed to attach overnight, after which they were incubated in serum-free medium for another 24 h. This incubation was followed by treatment with different concentrations of gastrin-17 (G-17; Peninsula Laboratories, San Carlos, CA, USA) in the presence or absence of the specific COX-2 inhibitor, NS-398 (Cayman Chemical, Ann Arbor, MI, USA). NS-398 and gastrin-17 were dissolved in DMSO and 30 mM NH4HCO3, respectively, as stock solutions. One μCi ml−1 of [3H]thymidine (New England Nuclear Products, Boston, MA, USA) was added and allowed to incorporate for 6 h at 37°C. Cells were washed with cold phosphate buffered saline (PBS) three times. Cold 10% trichloracetate (TCA) was added to cells and maintained at 4°C 30 min, after which cells were washed again with cold PBS three times and lysed in 0.1 N NaOH per 10% SDS. Radioactivity was counted in a liquid scintillation counter, and data were expressed as percentage of control±standard error (s.e.) of several experiments.
Mouse colorectal cancer model
Six- to ten-week old male BALB/C mice were obtained from Taconic (Germantown, NY, USA). MC-26 cells were harvested from subconflent cultures using trypsin-EDTA, followed by centrifugation at 300 G for 15 min at room temperature. Cells were then resuspended in serum-free DMEM or Hank's Balanced Salt Solution (Life Technologies, Inc, Gaithersburg, MD, USA), and the cell number was adjusted to a final concentration of 100 000 cells per ml. Using a 27-gauge needle and a 1 ml syringe, 100 μl of tumour cell suspension was injected subcutaneously into the flanks of mice. All animal studies were conducted using a protocol approved by the Animal Care and Use Committee at Boston University Medical Center and in accordance with UKCCCR Guidelines (Workman et al, 1998).
Animal study procedure
NS-398, dissolved in DMSO, was administered by oral gavage once daily. G-17 was dissolved in 0.9% NaCl and was administrated using an implanted Alzet® osmotic pump (Alza corporation, Palo Alto, CA, USA). For osmotic pump insertion, animals were anaesthetised using intraperitoneal pentobarbital (65 mg kg−1) injection. An incision ∼0.8 cm in length was made, and the osmotic pump was implanted subcutaneously. After tumour cell injection, mice were randomly divided into four groups (10 animals per group) on day 0, followed by treatment with different test reagents:
Group 1 (control group): Infusion of 0.9% NaCl by osmotic pump and DMSO (vehicle) 0.1 ml by gavage;
Group 2: Infusion of G-17 10 nmol kg−1 h−1 by osmotic pump and DMSO 0.1 ml by gavage;
Group 3: Infusion of G-17 10 nmol kg−1 h−1 by osmotic pump along with NS-398 1 mg kg−1 body weight by gavage; and
Group 4: Infusion of G-17 10 nmol kg−1 h−1 by osmotic pump along with NS-398 10 mg kg−1 body weight by gavage.
Subcutaneous tumour size was determined after day 7 by measuring the longest and shortest diameters of the tumour at 2–3 day intervals. Tumour volume (mm3) was calculated using the standard formula: tumour volume=(shortest diameter)2 × (longest diameter) × 0.5. After sacrificing the mice on day 18, tumours were excised and weighed and measured. Tumour tissue was flash frozen in liquid nitrogen and stored at –70°C, and a portion of the tissue was fixed with 10% formalin for histological examination.
Prostaglandin E2 assay
MC-26 cells (100 000 ml−1) were seeded onto six-well plates and allowed to attach overnight. Cells were then cultured in serum-free medium for another 24 h, followed by treatment with 20 nM of G-17. To evaluate the activity of COX, prostaglandin E2 (PGE2), the major metabolite of arachidonic acid metabolism, was measured by an enzyme immunoassay (EIA) kit (Cayman Chemical, Ann Arbor, MI, USA) in culture media maintained at 20°C using the protocol provided by manufacturer. Measurements were made in triplicate in three separate experiments.
Transfection and reporter gene assays
To examine transcriptional regulation of the COX-2 promoter by gastrin, MC-26 cells were transiently transfected with 742-kb COX-2 promotor (kindly provided by Dr H Herschman, UCLA) or control plasmid pGL3-Luc (Promega, Madsion, WI, USA) in the presence of G-17 using LipofectamineTM Reagent (Life Technologies, Inc, Gaithersburg, MD, USA). A β-galactosidase-expressing plasimd was included in each transfection to monitor the transfection efficiency. For luciferase assay, transfected cells were washed twice with phosphate buffered saline (PBS, pH 7.4) and lysed in 200 μl of lysis buffer following the manufacturer's instructions (BD PharMingen, San Diego, CA, USA). β-galactosidase activity in 50 μl of the cell lysate was determined after 5–20 min incubation at 37°C with 2 mM chlorophenol red β-galactopyranoside (Boehringer Mannheim, Indianapolis, IN, USA) in 20 mM MgCl2, 0.1 mM MnCl2, 45 mM 2-mercaptoethanol, and 100 mM NaHPO4, pH 8.0. The reaction was stopped by adding 500 μl of 0.5 M EDTA, pH 8.0, and the absorbency at 570 nm measured using a spectrophotometer. With each experiment, luciferase activity was determined in duplicate and normalized to β-galactosidase activity for each dish.
Western blot hybridization
Mouse COX-2 and cyclin D1 monoclonal antibodies were purchased from BD transduction laboratories (Lexington, KY, USA). To extract protein from cells, MC-26 cells cultured under different conditions were harvested and lysed in RIPA buffer (PBS, 1% NP-40, 0.5% sodium deoxycholate, 0.1% SDS, 100 ng ml−1 PMSF, 66 ng ml−1 aprotinin). To extract protein from tissues, 0.1 g of tumour tissue was placed in 2.0 ml of cold RIPA buffer and homogenized for 1 min with Polytron-Aggregate (Kinmatica, Luzern, Switzerland). After removal of cell debris by centrifugation, total protein of cells or tissues was determined by BCA protein assay (Pierce chemical, Rockford, IL, USA). Protein was mixed with gel loading buffer (50 mM Tris pH 6.8, 2% SDS, 10% glycerol, 2% 2-mercaptoethanol, 0.1% bromphenol blue) and heated for 10 min at 100°C. Samples containing 20–40 μg protein were loaded on a 10–12% SDS–PAGE gel and then electrophoretically transferred to a polyvinylidene difluoride membrane in transfer buffer (25 mM Tris, 190 mM glycine, 20% methanol). The blots were blocked with 7% dry milk for 1 h at room temperature and incubated with the primary antibody overnight. They were then washed three times for 15 min each in Tris-buffered saline, containing 0.05% Tween-20. The blots were further incubated with the anti-mouse IgG antibody (Sigma) for 1 h at room temperature. After washing three times, blots were incubated with luminous ECL reagent (Pierce chemical, Rockford, IL, USA) for 10 s to 2 min and exposed to Kodak X-ray film. Protein bands were quantified by laser densitometry.
Immunohistochemistry
Proliferating cell nuclear antigen (PCNA) monoclonal antibodies were purchased from BD transduction laboratories (Lexington, KY, USA). Paraffin-embedded specimens were deparaffinized and incubated with PCNA antibody for 2 h at 37°C. The specimens were then incubated with the secondary antibody, anti-mouse IgG, for 1 h at 37°C and stained by the avidin-biotin peroxidase complex (ABC) method using the ABC staining system (Santa Cruz Biotech, Santa Cruz, CA, USA). They were visualized by 3,3-diaminobenzidine (DAB) staining and counterstaining with haematoxylin. To confirm the specificity of the mouse PCNA antibody, tonsil specimens was used as a positive control. The PCNA index was evaluated by counting the number of PCNA-positive staining cells out of a total of 500 tumour cells: PCNA index= (number of PCNA-positive-staining cells per 500 cells counted) × 100%.
Statistical analysis
One-way ANOVA was performed to compare [3H]thymidine incorporation, tumour volume and weight, PCNA index, and densitometric values of Western blot bands among the different animal groups, followed by Tukey's procedure for paired comparison. The two-tailed t-test was used to compare PGE2 levels in the different conditions. Statistical significance was assigned if P<0.05.
Results
Cell proliferation
The addition of G-17 led to an increase in [3H]thymidine incorporation, with ∼40% increase detected using at a G-17 concentration of 20 nM. NS-398, a COX-2 selective inhibitor, decreased [3H]thymidine incorporation in a dose-dependent manner. When MC-26 cells were incubated in culture media containing both 20 nM G-17 and 10 μM NS-398, [3H]thymidine incorporation was 110.0% of control (Figure 1), indicating that the enhancement in cell proliferation induced by gastrin could be partially attenuated by COX-2 inhibition with NS-398.
[3H]thymidine incorporation of colon cancer cells (MC-26) treated with gastrin-17 (G-17) in the absence or presence of the COX-2 selective inhibitor NS-398. DNA synthesis was estimated by [3H]thymidine incorporation into cellular DNA, as described in the Materials and Methods section, under various conditions: gastrin-17 (A) and the combination of G-17 and NS-398 (B). *P<0.05.
Tumour growth
In animal studies, 6- to 10-week old BALB/C mice were inoculated with MC-26 cells subcutaneously on day 0. Figure 2 depicts the effects of G-17 and NS-398 on tumour volume and tumour weight at the end of the period of observation (day 18). Twenty per cent of G-17 treated mice died as a result of heavy tumour burden. Both tumour volume and weight in mice treated with G-17 (10 nmol kg−1 h−1) were significantly greater than those in the control group (tumour volume 1761.8±427.6 mm3 vs 1220.2±224.0 mm3, tumour weight 0.53±0.04 g vs 0.38±0.07 g, P<0.05). In contrast, no significant differences in tumour volume and weight from control was detected in mice treated with both NS-398 (1 mg kg−1) and G-17 (10 nmol kg−1 h−1). Moreover, tumour growth stimulated by G-17 was reversed by both low- (1 mg kg−1) and high-dose (10 mg kg−1) NS-398. The latter not only suppressed gastrin-induced tumour growth, but also unstimulated (control) tumour growth (tumour volume: 955.8±325.1 mm3 vs 1220.2±224.0 mm3, P<0.05; tumour weight: 0.15±0.09 g vs 0.38±0.07 g, P<0.01).
Effect of gastrin-17 (G-17) or/and the COX-2 selective inhibitor (NS-398) on colon cancer growth in vivo. MC-26 cells were injected subcutaneously in the flank of 6 to 10-week old male BALB/c mice. Subcutaneous tumour size was determined from day 7 by measuring the longest and shortest diameter of the tumour at 2–3 days intervals. (A) Tumour volume (mm3) was calculated by a standard formula: Volume=(the shortest diameter)2 × (the longest diameter) × 0.5. (B) Tumour weight was measured on day 18 after tumour was removed from sacrificed mice. *P<0.05. **P<0.01.
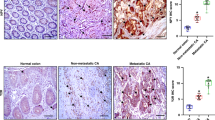
Consistent with tumour growth, cyclin D1 protein and PCNA index in tumour tissues were significantly greater in the tumour tissue of G-17 treated mice. Low-dose NS-398 (1 mg kg−1) partially attenuated gastrin-induced cyclin D1 and PCNA, while high-dose NS-398 (10 mg kg−1) significantly decreased both of them to values significantly less than unstimulated conditions (Figures 3 and 4).
Proliferating cell nuclear antigen (PCNA) in colon cancer treated with gastrin-17 in the absence or presence of NS-398. Cells were injected subcutaneously in the flank of 6 to 10-week old male BALB/c mice. Mice were sacrificed on day 18, and PCNA index was determined by immunohistochemistry, as described in the Materials and Methods section (A: Control, B: Gastrin-17 10 nmol kg−1 h−1, C: Gastrin-17 10 nmol kg−1 h−1 and NS-398 10 mg kg−1, D: Gastrin-17 10 nmol kg−1 h−1 and NS-398 1 mg kg−1, E: Quantification of PCNA index. *P<0.05, **P<0.01).
COX-2 promoter activity, COX-2 protein expression and prostaglandin E2 (PGE2) levels
To study whether G-17 is capable of inducing COX-2 transcription, cells were transiently transfected with a COX-2 promoter luciferase construct, and luciferase assays were performed, as described above. COX-2 promoter activity was induced approximately two-fold in transfected cells incubated in presence of G-17 (100 nM) at 24 h. In addition, COX-2 protein expression was significantly increased in MC-26 cells incubated in the presence 10, 20, 50 and 100 nM G-17 at 24 h. When cells were incubated with 20 nM G-17, levels of PGE2, the major product of cyclo-oxygenase, were significantly increased at 24 h (215.9±13.6 pg well−1 vs 170.8±27.9 pg well−1, P<0.05) and 48 h (350.8±39.7 pg well−1 vs 272.2±35.6 pg well−1, P<0.05) (Figure 5).
Discussion
Previous studies have reported that gastrin and NSAIDs possess opposing effects on cell proliferation. Gastrin has long been recognized as a mitogenic factor that stimulates the growth of pre-existing tumours of GI origin (Baldwin and Shulkes, 1998; Smith and Watson, 2000; Dockray et al, 2001). Interruption of the effects of gastrin as a potential target in the treatment of colorectal cancer, using several different approaches, such as the gastrin (CCK-B or CCK-2) receptor antagonists, proglumide and benotript, has been assessed (Watson et al, 1992a, b). The major drawback of these compounds is their lack of potency, with relatively high concentrations required to displace amidated G-17. L-365,260 has a greater affinity for the gastrin receptor than proglumide and has been shown to reverse gastrin-stimulated growth of GI tumour cell, both in vitro and in vivo (Piontek and Hengels, 1993; Watson et al, 1991). However, this antagonist does not appear to inhibit basal growth of the tumour and lacks the capacity to interact with alternate gastrin receptor subtypes. In contrast, the effectiveness of anti-gastrin antibodies in inhibiting tumour growth has been demonstrated in several animal models of colorectal cancer (Watson et al, 1995, 1996, 2000).
The benefit of nonselective COX inhibitors in preventing tumorigenesis and tumour growth has been demonstrated in numerous studies (Dubois and Smalley, 1996; Levy, 1997). However, the use of these agents is often associated with the development of serious adverse GI events. COX-2 selective inhibitors are thought to exert similar anti-inflammatory and antimitogenic effects, but with diminished toxicity (Wolfe et al, 1999). N-[2-(cyclohexyloxy)-4-nitrophenyl]-methanesulphonamide (NS-398) is a sulfonamide derivative that inhibits COX-2 specifically with an IC50 of 30 nM. It does not affect COX-1 enzyme activity at concentrations exceeding 100 μM, and it inhibits COX-1 dependent prostanoid production only minimally even at doses >200 mg kg−1 (Futaki et al, 1994; Gierse et al, 1995). The results of these studies suggest the possibility of a functional relationship between gastrin and COX-2 expression and demonstrate that COX-2 selective inhibition is capable of reversing the trophic properties of growth on colorectal adenocarcinoma. Because COX-2 selective inhibition has been shown to possess antineoplastic properties with few adverse GI events, the use of these agents may potentially represent a novel therapeutic approach to reduce the risk of colon cancer associated with hypergastrinaemia.
Despite these observations, the cellular and molecular mechanisms governing any potential relationship between COX-2 and gastrin require further clarification. In this study, when MC-26 colorectal cancer cells were incubated in the presence of gastrin, significant increases in COX-2 protein levels and COX-2 promoter activity was detected, compared with control conditions. Furthermore, using a sensitive enzyme immonoassay (EIA) for the measurement of PGE2, modest, but significant, increases in PGE2 levels in response to 20 nM gastrin were observed. While further studies are necessary to clarify any possible functional relationship, the present results do imply that a COX-2 mediated pathway may be stimulated by gastrin and may contribute to its trophic effects on colorectal cancer.
Cyclin D1 is a protein involved in cell cycle regulation in both normal and neoplastic cells (Hunter and Pines, 1994). In the G1 (resting) phase of the cell cycle, cyclin D1 along with its cyclin dependent kinase (CDK) partner, is responsible for transition to the S (DNA synthesis) phase (Sherr, 1996). Overexpression of cyclin D1 releases a cell from its normal control and causes transformation to a malignant phenotype. Previous studies have demonstrated that cyclin D1 is increased in adenomatous polyps and in both sporadic and familial forms of colorectal cancer (Motokura and Arnold, 1993; Bartkova et al, 1994; Arber et al, 1996, 1997). Consistent with these prior observations, in the present study, gastrin increased cyclin D1 levels in vivo and in vitro, an effect that was reversed with NS-398. In addition to cyclin D1, PCNA functions as an auxiliary protein to DNA polymerase gamma and as a co-factor in DNA synthesis. The synthesis and expression of PCNA are enhanced in proliferating cells including those that are tumour-derived. Determination of PCNA represents one of the most reliable methods for evaluating proliferation in cells and tissues (Prosperi, 1997). In the present study, the PCNA index was significantly increased in gastrin-treated tumours when compared with control. Moreover, similar to studies assessing cyclin D1, the addition of NS-398 (10 mg kg−1 body weight) reversed the gastrin-induced increase in PCNA expression.
In conclusion, the results of these studies demonstrate that COX-2 might represent one of the downstream targets of gastrin and that selective COX-2 inhibition is capable of reversing the trophic properties of gastrin and presumably prevent growth of CRC induced by hypergastrinaemia. In addition to its effects on cyclin D1 and PCNA, it is certainly possible that other intracellular pathways are involved in mediating the trophic properties of gastrin on neoplastic proliferation. Although the therapeutic implications are obvious, further studies will be necessary to elucidate the cellular and molecular mechanisms governing any potential functional relationship between COX-2 and gastrin.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Arber N, Doki Y, Han EK, Sgambato A, Zhou P, Kim NH, Delohery T, Klein MG, Holt PR, Weinstein IB (1997) Antisense to cyclin D1 inhibits the growth and tumorigenicity of human colon cancer cells. Cancer Res 57: 1569–1574
Arber N, Hibshoosh H, Moss SF, Sutter T, Zhang Y, Begg M, Wang S, Weinstein IB, Holt PR (1996) Increased expression of cyclin D1 is an early event in multistage colorectal carcinogenesis. Gastroenterology 110: 669–674
Baldwin GS, Shulkes A (1998) Gastrin, gastrin receptors and colorectal carcinoma. Gut 42: 581–584
Barnes CJ, Cameron IL, Hardman WE, Lee M (1998) Non-steroidol anti-inflammatory drug effect on crypt cell proliferation and apoptosis during initiation of rat colon carcinogenesis. Br J Cancer 77: 573–580
Barnes CJ, Lee M (1998) Chemoprevention of spontaneous intestinal adenomas in the adenomatous polyposis coli Min mouse model with aspirin. Gastroenterology 114: 873–877
Bartkova J, Lukas J, Strauss M, Bartek J (1994) The PRAD-1/cyclin D1 oncogene product accumulates aberrantly in a subset of colorectal carcinomas. Int J Cancer 58: 568–573
Dockray GJ, Varro A, Dimaline R, Wang T (2001) The gastrins: their production and biological activities. Annu Rev Physiol 63: 119–139
DuBois RN, Smalley WE (1996) Cyclooxygenase, NSAIDs, and colorectal cancer. J Gastroenterol 31: 898–906
Futaki N, Takahashi S, Yokoyama M, Arai I, Higuchi S, Otomo S (1994) NS-398, a new anti-inflammatory agent, selectively inhibits prostaglandin G/H synthase/cyclooxygenase (COX-2) activity in vitro. Prostaglandins 47: 55–59
Giardiello FM, Offerhaus GJ, DuBois RN (1995) The role of nonsteroidal anti-inflammatory drugs in colorectal cancer prevention. Eur J Cancer 31A: 1071–1076
Gierse JK, Hauser SD, Creely DP, Koboldt C, Rangwala SH, Isakson PC, Seibert K (1995) Expression and selective inhibition of the constitutive and inducible forms of human cyclo-oxygenase. Biochem J 305: 479–484
Giovannucci E, Rimm EB, Stampfer MJ, Colditz GA, Ascherio A, Willett WC (1994) Aspirin use and the risk for colorectal cancer and adenoma in male health professionals. Ann Intern Med 121: 241–246
Hakanson R, Blom H, Carlsson E, Larsson H, Ryberg B, Sundler F (1986) Hypergastrinaemia produces trophic effects in stomach but not in pancreas and intestines. Regul Pept 13: 225–233
Hunter T, Pines J (1994) Cyclins and cancer. II: Cyclin D and CDK inhibitors come of age. Cell 79: 573–582
Klingensmith ME, Neville LJ, Delpire E, Wolfe MM, Soybel DI (1999) Gastrin-mediated effects of omeprazole on rat colon mucosa. Surgery 126: 272–278
Koh TJ, Chen D (2000) Gastrin as a growth factor in the gastrointestinal tract. Regul Pept 93: 37–44
Koh TJ, Dockray GJ, Varro A, Cahill RJ, Dangler CA, Fox JG, Wang TC (1999) Overexpression of glycine-extended gastrin in transgenic mice results in increased colonic proliferation. J Clin Invest 103: 1119–1126
Lamberts R, Wartenberg T, Creutzfeldt W (1999) Role of circulating gastrin in colorectal adenomas and carcinomas. Digestion 60: 101–109
Levy GN (1997) Prostaglandin H synthases, nonsteroidal anti-inflammatory drugs, and colon cancer. Faseb J 11: 234–247
Modlin IM, Kidd M, Marks IN, Tang LH (1997) The pivotal role of John S. Edkins in the discovery of gastrin. World J Surg 21: 226–234
Motokura T, Arnold A (1993) Cyclin D and oncogenesis. Curr Opin Genet Dev 3: 5–10
Piontek MK, Hengels KJ (1993) Differential mode of action of high- and low-affinity CCK/gastrin receptor antagonists in growth inhibition of gastrin–responsive human gastric adenocarcinoma cells in vitro. Anticancer Res 13: 715–720
Prosperi E (1997) Multiple roles of the proliferating cell nuclear antigen: DNA replication, repair and cell cycle control. Prog Cell Cycle Res 3: 193–210
Sawaoka H, Kawano S, Tsuji S, Tsujii M, Gunawan ES, Takei Y, Nagano K, Hori M (1998) Cyclooxygenase-2 inhibitors suppress the growth of gastric cancer xenografts via induction of apoptosis in nude mice. Am J Physiol 274: G1061–G1067
Sheng H, Shao J, Kirkland SC, Isakson P, Coffey RJ, Morrow J, Beauchamp RD, DuBois RN (1997) Inhibition of human colon cancer cell growth by selective inhibition of cyclooxygenase-2. J Clin Invest 99: 2254–2259
Sherr CJ (1996) Cancer cell cycles. Science 274: 1672–1677
Singh P, Velasco M, Given R, Wargovich M, Varro A, Wang TC (2000) Mice overexpressing progastrin are predisposed for developing aberrant colonic crypt foci in response to AOM. Am J Physiol Gastrointest Liver Physiol 278: G390–G399
Singh P, Walker JP, Townsend Jr CM, Thompson JC (1986) Role of gastrin and gastrin receptors on the growth of a transplantable mouse colon carcinoma (MC-26) in BALB/c mice. Cancer Res 46: 1612–1616
Smith AM, Watson SA (2000) Review article: gastrin and colorectal cancer. Aliment Pharmacol Ther 14: 1231–1247
Stepan VM, Sawada M, Todisco A, Dickinson CJ (1999) Glycine-extended gastrin exerts growth-promoting effects on human colon cancer cells. Mol Med 5: 147–159
Sundler F, Hakanson R, Carlsson E, Larsson H, Mattsson H (1986) Hypergastrinemia after blockade of acid secretion in the rat: trophic effects. Digestion 35: 56–69
Thorburn CM, Friedman GD, Dickinson CJ, Vogelman JH, Orentreich N, Parsonnet J (1998) Gastrin and colorectal cancer: a prospective study. Gastroenterology 115: 275–280
Tsujii M, Kawano S, Tsuji S, Sawaoka H, Hori M, DuBois RN (1998) Cyclooxygenase regulates angiogenesis induced by colon cancer cells. Cell 93: 705–716
Watson S, Durrant L, Elston P, Morris D (1991) Inhibitory effects of the gastrin receptor antagonist (L-365,260) on gastrointestinal tumor cells. Cancer 68: 1255–1260
Watson SA, Clarke PA, Morris TM, Caplin ME (2000) Antiserum raised against an epitope of the cholecystokinin B/gastrin receptor inhibits hepatic invasion of a human colon tumor. Cancer Res 60: 5902–5907
Watson SA, Crosbee DM, Morris DL, Robertson JF, Makovec F, Rovati LC, Hardcastle JD (1992a) Therapeutic effect of the gastrin receptor antagonist, CR2093 on gastrointestinal tumour cell growth. Br J Cancer 65: 879–883
Watson SA, Michaeli D, Grimes S, Morris TM, Crosbee D, Wilkinson M, Robinson G, Robertson JF, Steele RJ, Hardcastle JD (1995) Anti-gastrin antibodies raised by gastrimmune inhibit growth of the human colorectal tumour AP5. Int J Cancer 61: 233–240
Watson SA, Michaeli D, Grimes S, Morris TM, Robinson G, Varro A, Justin TA, Hardcastle JD (1996) Gastrimmune raises antibodies that neutralize amidated and glycine- extended gastrin-17 and inhibit the growth of colon cancer. Cancer Res 56: 880–885
Watson SA, Morris DL, Durrant LG, Robertson JF, Hardcastle JD (1992b) Inhibition of gastrin-stimulated growth of gastrointestinal tumour cells by octreotide and the gastrin/cholecystokinin receptor antagonists, proglumide and lorglumide. Eur J Cancer 28A (8–9): 1462–1467
Watson SA, Smith AM (2001) Hypergastrinemia promotes adenoma progression in the APC(Min−/+) mouse model of familial adenomatous polyposis. Cancer Res 61: 625–631
Wolfe MM (1992) Hypergastrinemia and colonic neoplasia: coincidental or related?. Gastroenterology 103: 1361–1363
Wolfe MM, Lichtenstein DR, Singh G (1999) Gastrointestinal toxicity of nonsteroidal antiinflammatory drugs. N Engl J Med 340: 1888–1899
Workman P, Twentyman P, Balkwill F, Balmain A, Chaplin D, Double J, Embleton J, Newell D, Raymond R, Stables J, Stephens T, Wallace J (1998) United Kingdom Co-ordinating Committee on Cancer Research (UKCCCR) Guidelines for the welfare of animals in experimental neoplasia, 2nd edn. Br J Cancer 77: 1–10
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Yao, M., Song, D., Rana, B. et al. COX-2 selective inhibition reverses the trophic properties of gastrin in colorectal cancer. Br J Cancer 87, 574–579 (2002). https://doi.org/10.1038/sj.bjc.6600495
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6600495
Keywords
This article is cited by
-
Identification of novel Cyclooxygenase-2-dependent genes in Helicobacter pylori infection in vivo
Molecular Cancer (2009)
-
Cyclo-oxygenase-Independent Inhibition of Apoptosis and Stimulation of Proliferation by Leptin in Human Colon Cancer Cells
Digestive Diseases and Sciences (2007)
-
Effects of Cyclooxygenase-2 Inhibition on Serum and Tumor Gastrins and Expression of Apoptosis-Related Proteins in Colorectal Cancer
Digestive Diseases and Sciences (2006)
-
Gastrin stabilises β-catenin protein in mouse colorectal cancer cells
British Journal of Cancer (2005)
-
Gastrin promotes human colon cancer cell growth via CCK‐2 receptor‐mediated cyclooxygenase‐2 induction and prostaglandin E2 production
British Journal of Pharmacology (2005)