Abstract
Overexpression of the cyclin-dependent kinase inhibitor p27Kip1 has been demonstrated to induce cell cycle arrest and apoptosis in various cancer cell lines, but has also been associated with the opposite effect of enhanced survival of tumor cells and increased resistance towards chemotherapeutic treatment. To address the question of how p27Kip1 expression is related to apoptosis induction, we studied doxycycline-regulated p27Kip1 expression in K562 erythroleukemia cells. p27Kip1 expression effectively retards proliferation, but it is not sufficient to induce apoptosis in K562 cells. p27Kip1-expressing K562 cells, however, become resistant to apoptosis induction by the proteasome inhibitors PSI, MG132 and epoxomicin, in contrast to wild-type K562 cells that are efficiently killed. Cell cycle arrest in the S phase by aphidicolin, which is not associated with an accumulation of p27Kip1 protein, did not protect K562 cells against the cytotoxic effect of the proteasome inhibitor PSI. The expression levels of p27Kip1 thus constitute an important parameter, which decides on the overall sensitivity of cells against the cytotoxic effect of proteasome inhibitors.
Similar content being viewed by others
Introduction
The ubiquitin-dependent proteasome pathway is the major proteolytic system encountered in the cytoplasm and nucleus of virtually all nucleated eukaryotic cells (reviewed in Hershko and Ciechanover1). Apparently, the majority of all cellular proteins are subjected to this turnover mechanism.2 This pathway usually rapidly degrades damaged or misfolded proteins. The ubiquitin–proteasome system does, however, not only serve as an intracellular shredding device that accepts damaged protein substrates for recycling. It is equally important for the generation of peptides presented in the context of MHC class I molecules on the cell surface2 and, in addition, is intrinsically linked to various signal transduction pathways by the selective degradation of short-lived proteins exerting crucial regulatory functions within a cell. Transcriptional regulators such as IkBα, p53, E2F1, c-jun or β-catenin belong to this class of substrate proteins as well as proteins regulating cell cycle progression (cyclins, cyclin-dependent kinases, (cdk's), the cyclin-dependent kinase inhibitor (cki) p27Kip1).1
Recently, it has become evident that proteasomal function is essential for cell survival and that inhibition of proteasomal activity, in particular of the chymotryptic activity by low molecular weight inhibitors, is a powerful means to induce caspase activation and apoptosis in many cell types, even in the absence of functional p53.3,4,5,6,7,8
Biochemical features consistently observed in experiments involving apoptosis induction by proteasome inhibitors are the accumulation of high molecular weight polyubiquitinated substrate proteins as well as an increase in the relative amounts of the tumor suppressor protein p539,10 and of the cki's p21Waf1 11,12 and p27Kip1.13 p27Kip1 together with p21Waf1 and p57Kip2 belong to a family of proteins that inhibit the kinase activity of cyclin/cdk complexes by stochiometric binding. In cycling cells the cki p27Kip1 is usually degraded at the transition from the G1 into the S phase of the cell cycle.13 Cyclin/cdk complexes for instance, blocked by p27Kip1, are then free to phosphorylate the Rb protein, which releases the transcription factor E2F required for the synthesis of S phase proteins.
Various classes of proteasome inhibitors have been developed, which have the potential to reduce dramatically the viability of proliferating cells (review by Kisseler and Goldberg 14), a property that is currently exploited in the search for novel antineoplastic drugs.15,16,17,18
However, nonproliferating, quiescent cells, in short-term experiments at least, remain largely unaffected and are remarkably protected against certain apoptosis-inducing stimuli by proteasomal inhibitors.19,20
Human leukemic HL60 cells, when terminally differentiated upon treatment with phorbolester, adopt macrophage-like properties with an adherent and quiescent phenotype. These differentiated nonproliferating HL60 cells – in a very analogous fashion – show a reduced sensitivity to apoptosis induction by proteasome inhibitors.3 A similar difference in terms of sensitivity to the cytotoxic effect of proteasome inhibitors can be observed when contact-inhibited, quiescent and subconfluent cycling primary endothelial cells are compared with each other.21 One common feature of both, the quiescent HL60 and the quiescent endothelial cells, is the upregulation of the cki p27Kip1, which appears to be a general property of cells that switch to a nonproliferative phenotype.22,23,24
To determine whether the resistance of quiescent cells towards the potent cytotoxic effect of proteasome inhibitors is directly related with the expression levels of p27Kip1, we investigated in the present study the consequences of inducible ectopic expression of p27Kip1 in the Philadelphia positive chronic myeloid leukemia (CML)-derived K562 cell line. We can show that K562 cells, which lack functional p53 and are resistant to a variety of chemotherapeutic drugs, readily undergo proteasome-inhibitor-mediated apoptosis when they are proliferating, but are protected by the expression of p27Kip1. This finding has implications for tumor development in general and in particular for the modalities of tumor therapies employing chemotherapeutic drugs.
Results
Inducible expression of HA-tagged p27Kip1in K562 cells
To investigate the functional role of p27Kip1 accumulation, as is observed during apoptosis induction by proteasome inhibitors, we inducibly expressed HA-tagged p27Kip1 (p27HA) under the control of a tetracycline-regulated expression system (pHD22/6; Figure 1a). K562 cells were transfected by a transferrinfection protocol and stable transfected clones were isolated by puromycin selection. Several clones could be identified that expressed p27HA in a constitutive fashion (not shown). Two of the clones that displayed doxycycline-regulated p27HA expression (K562-75 and K562-99) were investigated further.
Schematic diagram of an inducible p27Kip1 cassette inserted in pBabe puro. See text for details (a). Dose-dependent induction of p27HA: lysates of cells incubated for 24 h in the presence of increasing concentrations of doxycycline were analyzed by Western blotting using antibodies directed against the HA-Tag (12CA5) or against p27Kip1(b). Kinetics of p27HA induction: cells were exposed to a single dose of doxycycline (1 μg/ml) and the changes in the relative amounts of p27HA protein were analyzed (c). Reversibility of p27HA induction: p27HA expression was induced for 18 h (1 μg/ml doxycycline), followed by three washes and further incubation in the absence of doxycycline. At the indicated time points cells were lysed, subjected to SDS–PAGE and analyzed for the presence of p27HA (d)
Upon addition of doxycycline, p27HA was expressed in both clones in a dose-dependent manner, reaching a plateau between 1 and 2 μg/ml doxycycline (Figure 1b). Higher concentrations of the inducer did not result in a further increase in the amounts of p27HA protein. Residual expression of p27HA was detected in the absence of doxycycline. p27HA expression occurred rapidly after addition of doxycycline and could be detected already 6 h after addition of the drug (Figure 1c). The maximum of p27HA expression after a single administration of doxycycline was reached within 24–48 h of incubation in the presence of the drug, with levels of p27HA starting to decline again after 48 h (Figure 1c). When cells were allowed to resume proliferation in doxycycline-free medium after an initial p27HA induction for 18 h, baseline levels of p27HA expression were reached again within 48 h (Figure 1d). Expression of p27HA did not lead to differentiation of the K562 cells as judged by the absence of morphological alterations upon p27HA expression in cytospin preparations or the expression of the erythroid differentiation marker hemoglobin (Table 1).
Nuclear localization of p27HA
Immunofluorescence staining of cytospin preparations of both p27HA-expressing K562 clones demonstrated a strong nuclear staining for p27HA upon induction by doxycycline (Figure 2), indicating that the bipartite nuclear localization signal present close to the N-terminus of p27Kip1 is not destroyed by the introduction of the HA-Tag and is still functional, as it targets the protein to the correct subcellular compartment.
Nuclear localization of the ectopic p27HA. K562-75 (a–d) and K562-99 cells (e–h) were stimulated (1 μg/ml doxycycline) for 24 h, transferred onto glass slides and stained with the HA-specific antibody 3F10 to localize p27HA protein (c, g). Nuclear counterstaining was performed with Hoechst 33342 (d, h). Controls grown in the absence of doxycycline are shown in (a, b; K562-75) and (e, f; K562-99)
p27HA blocks K562 cell proliferation, but is not sufficient to induce apoptosis
We next investigated the capacity of p27HA to act as a cki and block cell proliferation. Expression of p27HA shifted the relation between hyperphosphorylated (ppRb) and hypophosphorylated (pRb) towards the hypophosphorylated form with kinetics that paralleled p27HA expression (Figure 3a, compare with Figure 1c). Densitometric quantification of the different phosphorylated forms of pRb indicated that there is a more than two- fold increase of the hypophosphorylated form of pRb at 24 h after doxycycline administration for clone K562-75 and a 0.6-fold increase for clone K562-99 (Figure 3b). Incubation of parental K562 cells in medium alone or in medium containing doxycycline (1 μg/ml) for 72 h did not result in a similar redistribution between the different phosphorylated forms of pRb (Figure 3c), excluding the possibility that the observed changes in pRb phosphorylation are due to changes in culture conditions or induced by doxycycline (1 μg/ml) itself, independently from p27HA expression.
p27HA expression leads to hypophosphorylation of pRb. (a) Western blot analysis of the variably phosphorylated isoforms of Rb in K562-75 and K562-99 cells after induction of p27HA (1 μg/ml doxycycline). (b) Densitometric quantification of results shown in a. (c) Phosphorylation status of pRb of parental K562 control cells grown either in the absence or the presence of doxycycline (1 μg/ml)
K562-75 and K562-99 cells become arrested primarily in G0/G1, as determined by propidium iodide staining and FACS analysis of cells incubated with doxycycline for 24 or 48 h (Figure 4a). No such arrest could be observed in K562 cells grown either in medium alone or in the presence of doxycycline (1 μg/ml), indicating that this arrest is not due to unspecific effects of doxycycline or to changes in culture conditions during the incubation period (Table 2). Determination of the cumulative cell numbers upon induction of p27HA in addition demonstrated that incubation of cells in the presence of 1 μg/ml of doxycycline (single addition of the drug at t=0 h) for 6 days was sufficient to block cell proliferation by 79% (K562-75) and by 66% (K562-99) (Figure 4b). A doxycycline concentration of 2.0 μg/ml not only increased growth inhibition further to 84% (K562-75) and 76% (K562-99), but also reduced the proliferation of untransfected K562 control cells to some extent (Figure 4b). Hence, all further experiments were carried out in the presence or absence of 1 μg/ml of doxycycline.
p27HA expression induces cell cycle arrest and growth inhibition of K562-75 and K562-99 cells. (a) Cell cycle distribution profiles of K562-75 and K562-99 cells after growth for 0, 24, and 48 h in the presence of doxycycline (1 μg/ml). Shown are the results of a representative experiment out of at least three experiments with similar results. (b) Cumulative cell numbers of K562wt (empty bars), K562-75 (hatched bars) and K562-99 (black bars) cells were determined after 6 days of growth in the presence of 1 or 2 μg/ml of doxycycline, and are expressed as the percentage of control cells that did not receive doxycycline. Experiments were performed in duplicate and repeated at least twice with similar results
Having demonstrated that p27HA expression was sufficient to inhibit K562 proliferation, we next investigated whether expression of p27HA contributed to apoptosis induction in these cells. Within 72 h of doxycycline administration the number of apoptotic cells with a sub-G1 DNA content did not increase substantially (Figure 5), indicating that p27HA expression per se is not sufficient to induce the cell death program in K562 cells. Furthermore, PARP cleavage to the characteristic apoptotic 89 kDa fragment could not be detected in Western blotting experiments (Figure 5).
p27HA expression is not sufficient to induce apoptosis in K562 cells. (a) K562-75 received doxycycline (1 μg/ml) for the indicated time points, were stained with PI and then analyzed for the percentage of cells with a sub G1 DNA content. (b) Cell lysates were subjected to SDS–PAGE and analyzed by Western blotting for the cleavage of PARP. Arrowheads point at the position of uncleaved PARP (116 kDa) and at the signature 85 kDa fragment generated during apoptosis. Similar results as shown in (a, b) were also obtained for the clone K562-99 (not shown)
Inducible p27HA expression provides protection for K562 cells against proteasome inhibitors
CML cells are highly resistant against various chemotherapeutic drugs because of a chromosomal translocation, which results in the expression of the constitutively active kinase BCR-ABL. BCR-ABL is one of the most potent survival promoting gene products known so far, and is found in more than 95% of all patients suffering from chronic myeloid leukemia (CML).
Thus, incubation of K562 cells with 50 μM etoposide or campthotecin does not introduce a significant extent of apoptosis within 24 h (data not shown). In sharp contrast, three structurally different proteasome inhibitors, namely PSI and MG132 (both at 50 μM) as well as epoxomicin (2 μM), were able to induce up to 85% apoptosis within 15 h of incubation in K562 cells (Figure 6). In contrast, the calpain inhibitor calpeptin did not display any proapoptotic activity at 50 μM, nor did overexpression of calpastatin in K562 cells elicit any apoptotic response (unpublished results).
Expression of p27HA in K562 cells protects against the cytotoxic effects of proteasome inhibitors. K562 and K562-75 cells received for 15 h the proteasome inhibitors PSI, MG132 or epoxomicin, either in the absence of doxycycline (upper two rows of panels) or following a preincubation with doxycycline (1 μg/ml) for 24 and 48 h, respectively (bottom two rows of panels). The sub G1 DNA content of the cells as a measure of apoptosis induction was determined by PI staining and FACS analysis. Similar results were also obtained for the K562-99 clone (not shown)
Following induction of p27HA expression, a progressive protection of both K562 clones examined against the cytotoxic effect of all three proteasome inhibitors could be observed (Figure 6). Both inducible clones displayed a decrease in sensitivity already in the uninduced state, which can be explained by weak baseline expression of p27HA in the uninduced state. The protective effect then becomes very pronounced at 48 h of doxycycline pretreatment. The desensitizing effect of p27HA expression can also be demonstrated by analyzing the combined activity of effector caspases 3 and 7, which is markedly reduced in both clones when p27HA is induced (Figure 7a). Generation of the apoptosis-specific signature 85 kDa fragment of PARP is also diminished when apoptosis is induced in the presence of p27HA, indicating that caspase activation is restrained (Figure 7b).
(a) Determination of the combined activity of caspases 3 and 7 after induction of p27HA expression. p27HA was induced for 48 h by doxycycline (1 μg/ml), and caspase activities generated through the administration of proteasome inhibitors for 15 h were determined using the fluorigenic caspase substrate Z-DEVD-R110. Shown are the RFU±S.D. values for K562-75 (black bars) and K562-99 cells (hatched bars). Determinations were performed in triplicate. (b) PARP cleavage is reduced in the presence of p27HA. Cell extracts of K562wt, K562-75 and K562-99 cells incubated with the proteasome inhibitor MG132 for 15 h, either with or without a preincubation for 24 or 48 h with doxycycline (1 μg/ml), were subjected to SDS–PAGE and analyzed for the cleavage of PARP (C2-10). DMSO served as a vehicle control for MG132 (a, b)
One of the reasons for the failure of chemotherapy treatment of CML is the development of drug resistance in blast crisis cells, which has been associated with an amplification of the BCR-ABL gene25 or enhanced BCR-ABL expression.26 We therefore investigated whether induction of p27HA expression would alter the relative levels of BCR-ABL protein by Western blotting analysis. As can be seen in Figure 8a, the relative amounts of BCR-ABL kinase remain unchanged upon administration of doxycycline (Figure 8a).
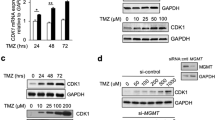
Protein levels for BCR-ABL (a), Bax and Bcl-2 (b) remain unaffected upon treatment of K562-75 cells with doxycycline. Equal loading of samples was controlled by reprobing the blots with anti-GAPDH. (c) Protein levels for BCR-ABL protein are reduced upon treatment with MG132 (50 μM, 15 h) in all cell lines in the presence or absence of doxycycline (1 μg/ml). Loading again was controlled by anti-GAPDH. (d) Reduced amounts of BCR-ABL protein are reflected by reduced extent of tyrosine phosphorylation in cells incubated with MG132. (1) Positive control: 20 μg of EGF-stimulated A431 control lysate. Equal loading of samples was controlled by reprobing the blots with β-actin
BCR-ABL harboring K562 cells express high amounts of the antiapoptotic protein Bcl-xL, but do not express detectable levels of the Bcl-2 protein.27 BCR-ABL stimulates expression of Bcl-xL through the constitutive activation of the transcription factor STAT5, which can bind to a STAT5 binding element in the Bcl-xL promoter. However, upregulation of Bcl-xL or Bcl-2, which could provide a potential explanation for the protective effect of ectopically expressed p27HA, could not be observed. Likewise, the relative levels of the proapoptotic bax protein do not change upon p27HA induction (Figure 8b) nor is there an increase in the expression of Bcl-2 in the presence of doxycycline (not shown). From these results we conclude that the protective effect of p27HA expression is independent from an upregulation of the antiapoptotic proteins Bcl-xL or Bcl-2 or the downmodulation of the proapoptotic bax protein. Even more, the relative amounts of BCR-ABL as well as c-ABL protein are reduced by the treatment with proteasome inhibitors (Figure 8c), a phenomenon that has been described earlier,28 excluding the possibility that increased amounts of BCR-ABL protein in p27HA-expressing cells are responsible for the protective effect. The reduced BCR-ABL levels are also reflected by an overall decrease in the extent of tyrosine phosphorylation (Figure 8d).
Cell cycle arrest at the G1/S transition is required to confer protection
We next examined whether the increased resistance of p27Kip1-expressing K562 cells against apoptosis induction by proteasome inhibitors can also be recapitulated in parental K562 cells that are arrested at a different position of the cell cycle.
For this purpose parental K562 cells were first pretreated for 24 h with aphidicolin to arrest the cells in the S phase of the cell cycle and then challenged with the proteasome inhibitor PSI for 15 h. S phase arrest by aphidicolin did not elicit an upregulation of endogenous p27Kip1 protein levels (Figure 9a), which was not expected, and was slightly toxic on its own (Figure 9b). When aphidicolin-arrested K562 cells were challenged with PSI, however, a protective effect of the aphidicolin treatment could not be observed (Figure 9b).
Aphidicolin blocks cell cycle progression in K562 cells, but does not confer protection against the proteasome inhibitors PSI. (a) Western blot analysis to detect endogenous p27Kip1 in S phase arrested cells. Only low amounts of p27Kip1 protein were present in aphidicolin (S phase) arrested cells as p27Kip1 is degraded at the G1/S transition. (b) Sub G1 DNA content of K562 cells following apoptosis induction by the proteasome inhibitor PSI (50 μM; 15 h) analyzed directly (upper panels) or after administration of aphidicolin (2 μg/ml) for 24 h (lower panels). (c) K562 cells induced by IPTG (2 mM, 24 h) to express p21Waf1 (arrowhead) showed increased amounts of endogenous p27Kip1 protein (arrowhead) and (d) became arrested in the G0/G1 compartment of the cell cycle. (e) p21Waf1- and p27Kip1-mediated cell cycle arrest at the restriction point (2 mM IPTG, 24 h) reduced the sub G1 DNA content of K562 cells following exposure to the proteasome inhibitor MG132 (50 μM) for 15 h
To further substantiate our observation that cell cycle arrest at the G1/S transition is required to confer protection against proteasome inhibitors, K562 cells that inducibly express p21Waf1 were employed.29 These cells upregulate endogenous p27Kip1 protein owing to a p21Waf1-mediated decrease in p27Kip1 phosphorylation and proteasomal degradation30 (Figure 9c). Upon induction of p21Waf1, increased amounts of p27Kip1 protein could be detected, cells again were arrested in G0/G1 (Figure 9d) and showed a reduced sensitivity towards MG132 (Figure 9e). Conversely, p27Kip1 induction by doxycycline did not elicit an increase in the relative amounts of p21Waf1 (unpublished results). From these results we conclude therefore that the protective effect of the p27Kip1-mediated G1/S arrest cannot be recapitulated by an arrest of the cells in the S phase and that the increased resistance of p27HA-expressing K562 cells towards proteasome inhibitor treatment specifically depends on the presence of the cdk inhibitor p27Kip1.
Discussion
Inhibition of K562 proliferation by p27Kip1
BCR-ABL kinase activity has been shown to be responsible for the suppression of endogenous p27Kip1,28,29 while pharmacological inhibition of the BCR-ABL kinase activity by the c-abl kinase inhibitor STI-571 rapidly upregulates p27Kip1 30 and induces apoptosis.9,10 A multiplicity of signaling pathways is activated by BCR-ABL kinase, and proteins such as RAS, PI3 K, JAK/STAT, Src kinases, focal adhesion kinase (FAK) and others have been identified as targets.31,32,33,34 Also, immediate early genes such as myc, fos and jun are induced by BCR-ABL,35,36 a process that can be correlated with an enhanced rate of transition from the G1 into the S phase of the cell cycle even in the absence of growth factors.
This is the first report demonstrating that re-expression of p27Kip1 potently reduced the proliferation rate of BCR-ABL-positive K562 leukemia cells and antagonized the deregulation of cell cycle checkpoints induced by BCR-ABL. p27Kip1 expression by itself was, nevertheless, not sufficient to induce apoptosis in these cells. Such a possibility has been suggested by experiments using adenoviral-mediated expression of p27Kip1 in tumor cells37,38,39 as well as by experiments using proteasome inhibitors to induce apoptotic cell death.3,18,40,41 The lack of apoptosis induction in K562 cells by expression of p27Kip1 therefore suggests that additional factors are necessary in K562 and other cells to decide if expression of the cki can effectively elicit the cell death program. Alternatively, a weak inherent proapoptotic property of p27Kip1 may be concealed by the multiple pro-survival functions of BCR-ABL, but is possibly revealed by overexpression in BCR-ABL negative cells. For various other genes, such as p53, bax, bad or bcl-xS, however, the proapoptotic function could be demonstrated when overexpressed in K562 cells42,43,44,45,46,47.
At the crossroad of the decision between proliferation, survival and death, proteins such as c-myc or c-jun could be positioned. These immediate early genes are not only involved in the regulation of cell cycle entry, as indicated earlier, but they also have well-described proapoptotic functions.48,49 Since they are substrates of the ubiquitin–proteasomal degradation pathway as well,50,51 they are rapidly accumulating together with p27Kip1 when the proteasome function is blocked by inhibitors, a process that might result in an internal signaling conflict that is answered by the cell through the induction of apoptosis. Such a scenario is supported by the observation that fibroblasts in which myc is activated under conditions where cell proliferation is blocked initiate apoptosis.52 An alternative explanation for proteasome-inhibitor-mediated apoptosis was recently suggested by Tani et al., who demonstrate that, concomitantly with the stabilization of myc protein, there is transcriptional upregulation of FasL mRNA leading to Fas receptor/caspase 8-mediated induction of apoptosis.53
p27Kip1 expression confers resistance to apoptosis induction
The presence of BCR-ABL in K562 cells is closely correlated with drug resistance and inhibition of apoptosis. Conversely, inactivation of the BCR-ABL kinase or suppression of BCR-ABL expression at least partially reverses the antiapoptotic effect of BCR-ABL.26,54,55 The most successful approach so far to antagonize BCR-ABL kinase activity was the development of the abl kinase inhibitor STI-571, which has shown striking clinical and cytogenetic benefits,56,57 but apparently can become ineffective due to mutations of BCR-ABL or to amplifications of the BCR-ABL gene.58,59,60,61 These findings emphasize the significance of BCR-ABL expression to promote cell survival and, consequently, BCR-ABL-positive CML cells have proven to be difficult to eradicate efficiently.
In this context, it appears remarkable that three different proteasome inhibitors, namely PSI, MG132 and epoxomicin, were able to induce apoptosis in BCR-ABL-positive K562 cells by an unknown mechanism involving the downmodulation of BCR-ABL kinase levels (Figure 8)28. This finding is confirming and extending earlier reports62,63 and is lending further support to the potential use of proteasome inhibitors either alone or in combination with other drugs as an effective treatment of leukemia, in particular of CML. Such an approach is also encouraged by results obtained with the proteasome inhibitor MLN341, which is currently under further investigation in clinical trials and which displays potent antitumor activity in vitro and in vivo.16,17,18,64
K562 cells, once they are induced to express p27Kip1, not only have a reduced proliferation rate but also become refractory towards the cytotoxic action of proteasome inhibitors, even in the presence of reduced BCR-ABL levels. The protective effect of increased p27Kip1levels is more pronounced in our robust doxycycline-dependent system where p27Kip1 is induced to relatively high levels, compared to the rather weak p21Waf1-mediated effect on p27Kip1 stabilization, and may be directly related to the different amounts of p27Kip1 present in the cells under the corresponding conditions.
A rather broad spectrum of effects has been ascribed to elevated levels of p27Kip1 protein, ranging from a proapoptotic function in various systems to survival-promoting properties in others. Overexpression of p27Kip1 by virtue of adenoviral expression systems was sufficient to induce apoptosis in various cancer cell lines,37,38,39 and the proapoptotic effect of elevated levels of p27Kip1 protein has therefore also served as an explanation for the cytotoxic effect of proteasome inhibitors3,18,40,41. These pro-apoptotic properties are also consistent with the notion that p27Kip1 exerts the task of a tumor suppressor gene. For instance, proteasome-dependent degradation of the cki p27Kip1 has been demonstrated to be enhanced in aggressive colorectal carcinomas,65 and such a reduction of the expression levels of p27Kip1 has been associated with reduced survival and poor prognosis also for breast cancer patients.66,67 An inverse correlation between levels of p27Kip1 and tumor grade has also been found to have prognostic significance for other tumors, such as colon, prostate, ovary, gastric carcinomas and nonsmall lung cancer,68 and mice deficient for p27Kip1 develop multiple tumors during adulthood69,70.
In contrast to these observations, it has also been shown that increasing p27Kip1 expression is associated with the opposite effect to enhance the survival of tumor cells and to increase the resistance towards chemotherapeutic treatments.71,72,73 Likewise, expression of p27Kip1 enhances the survival of serum-deprived p27−/− fibroblasts,74 while the reduction of p27Kip1 by an antisense strategy successfully sensitized tumor cells for the cytotoxic activity of flavopiridol.75 These observations are lending further support to the notion that under certain conditions p27Kip1 plays the role of a drug resistance factor.
When cells are switched to a nonproliferative phenotype and are rendered quiescent by serum removal, by treatment with TGF-β or by contact inhibition, they display increased amounts of p27Kip1.22,23,24 Increased p27Kip1 levels could thus provide an explanation for our earlier findings that differentiated HL60 cells as well as contact-inhibited and quiescent endothelial cells showed a reduced sensitivity against the cytotoxic action of proteasome inhibitors.3,21 It may be speculated that increased p27Kip1 levels could also be the reason why quiescent stem cells, positive for the BCR-ABL oncogene, display insensitivity to the tyrosine kinase inhibitor STI571 in vitro76 and provide an alternative explanation for the potential disease relapse in patients upon extended therapy with this drug.
One exception, however, to the rule that quiescent p27Kip1-expressing cells display chemoresistance are B cells from chronic lymphocytic leukemia patients (B-CLL), which are largely quiescent, express high levels of p27Kip1, but are sensitive to the cytotoxic action of proteasome inhibitors.72 These cells, however, possess a constitutively altered ubiquitin–proteasome system in contrast to normal lymphocytes, with a three-fold higher chymotryptic activity.72 This increased proteasomal activity may contribute to the constitutive activation of NF-kappa B, which has been shown to be essential for survival in these cells.73. Blocking transcriptional activation of NF-kappa B-controlled antiapoptotic genes by proteasome inhibitors consequently must have a dramatic impact on these cells.
Conclusion
The protective effect conferred by increased p27Kip1 expression has consequences for tumor development and tumor therapy, because p27Kip1 has to be considered as a double-edged sword: low p27Kip1 expression can be associated with accelerated tumor growth and poor prognosis.65,66,67. At the same time, p27Kip1-low tumors are more accessible for a tumor-targeted chemotherapy treatment. Conversely, high p27Kip1 expression implicates tumors with reduced growth rates and also with an enhanced resistance against the cytotoxic effects of proteasome inhibitors and other drugs rendering the tumor cells more difficult to eradicate.
As a consequence, we suggest that p27Kip1 expression levels should be regarded as a marker for the susceptibility of tumor cells to treatment with chemotherapeutic drugs. Concerning gene therapy strategies involving p27Kip1 delivery to tumor cells,77,78 it is also essential for the same reasons that precautions are taken to ensure that the protective effect of p27Kip1 expression against cytotoxic drugs does not inadvertently create tumor cell variants that are more resistant to conventional drug treatment regimens.
Materials and Methods
Chemicals and Antibodies
Antibodies used in Western blot assay were purchased from Santa Cruz Biotechnology (Bcl-2, Bax, Rb, p21Waf1), Transduction Laboratories (p27Kip1, Bcl-xL), Oncogene Research Products (c-abl, clone 24–21), Biomol (PARP, clone C-2-10) and Biogenesis (GAPDH). Antibodies recognizing the HA-Tag were either clone 12CA5 for Western blotting experiments or clone 3F10 (Roche Molecular Biochemicals) for immunofluorescence detection. Proteasome inhibitors PSI (N-carbobenzoxy-L-isoleucyl-L-γ-t-butyl-L-glutamyl-L-alanyl-L-leucinal) and MG132 (N-carbobenzoxy-L-leucyl-L-leucyl-L-leucinal) were obtained from the Peptide Institute (Osaka, Japan), and the proteasome inhibitor epoxomicin ((2R)-2-[acetyl-(N-methyl-L-isoleucyl)L-L-isoleucyl-L-threonyl-L-leucyl]-2-methyloxirane) from Calbiochem (Bad Soden, Germany). Inhibitors were dissolved in DMSO as 1000 × stock solutions and diluted into medium as indicated.
Cloning of p27Kip1 and vector construction
A pBabe puro retroviral vector (gift of H Land) was modified by insertion of an expression cassette containing a heptameric tetracycline responsive element (TRE) together with a reverse tetracycline-dependent transactivator (rtTA) element followed by a second TRE element with an inverted orientation relative to the 5′-LTR. The remaining EcoRI site between both elements allowed insertion of a C-terminally HA-tagged p27Kip1 (p27HA).
Full-length cDNA of human p27Kip1 was obtained by PCR amplification from an EST-clone (IMAG 998K191577; RZPD, Berlin), using primers p27-4 (AAGAATTCAAGATGT CAAACGTGCGAGTGTCTAAC) and p27-8 (TTGAATTCTCAGGAAGGTCCTCCCAGGCTGGCATAGTCAGGCACGTCATAAGGATAGCTTCCCCCCGTTTGACGTCTTCTGAGGCC). With both primers, EcoRI sites were introduced into the PCR product; primer p27-8 in addition introduced a C-terminal HA-Tag. The amplified PCR product was cut with EcoRI and ligated into pHD12 (see below). Correct orientation was confirmed by restriction analysis with HindIII/HincII and by sequencing using the primers rtTA-1 (AATTGACGAGTACGGTGGGTAG) and p27-14 (ATGTCTCTGCAGTGCTTCTC).
pHD12 had been constructed by 1) cloning a 470 bp BamHI/XhoI fragment containing the TRE from the pUDH 10-3 vector (gift of H Bujard) via blunt end ligation into the SalI site of pBabe puro; a clone had been selected carrying the plasmid with the TRE inserted in an inverted orientation relative to the 5′-LTR; and (2) by inserting a 1492 bp BamHI/XhoI fragment containing a TRE in front of an rtTA cassette isolated from the TOPO-2 RHD vector (gift of H Winkler) into the BamHI/XhoI sites. An internal EcoRI site within the 1492 bp BamHI/XhoI cDNA fragment previously subcloned into pBluescript vector had been deleted by cutting with EcoRI, blunt ending and religation.
Transfection of K562 cells and establishment of inducible clones
K562 cells cultured in RPMI containing 10% fetal calf serum and antibiotics were transfected by a transferrinfection protocol according to the instructions of the manufacturer (Bender Medsystems). Briefly, 2.5 × 106 cells were preincubated in 5 ml medium overnight with 100 μM desferrioxamine. On the next day, the cell number was adjusted to 5 × 105 cells/ml in fresh medium containing 100 μM desferrioxamine, and cells were transferred to a 24-well plate (1.25 × 105 cells/250 μl). To form the transfection complex 125 μl modified transferrin was mixed with 125 μl of pHD22/6 and incubated at room temperature (RT) for 30 min. After addition of chloroquin to the transfection mixture, the mixture was added to the cells for 4 h. Transfection medium was then replaced with fresh medium for 48 h, before cells were split into 96-well plates at a density of 10 cells/well and subjected to selection by puromycin (2 μg/ml). After expansion to 12-well plates, cells were incubated in the presence or absence of doxycycline for 24 h (2 μg/ml), lysed and inducible clones were selected by screening for p27HA expression in Western blotting experiments. K562 cells inducible for p21Waf1 (kindly provided by R Steinman, Pittsburgh) were cultured in the same medium as described above; induction of p21Waf1 was achieved by incubation in the presence of 2 mM IPTG.
Proliferation assay
Cells were seeded onto 24-well plates at a density of 5000 cells/ml and cell numbers were determined at the indicated time points in the absence or presence of doxycycline using a CASY cell counter (Schärfe Systems, Reutlingen, Germany). Experiments were performed in duplicate or triplicate and repeated at least twice.
FACS analysis
The extent of apoptosis induced by proteasome inhibitors was performed as described,79 with minor modifications. Cells (5 × 105) plated onto six-well tissue culture plates were treated with proteasome inhibitors for 15 h, either directly after plating or after preincubation with doxycycline (1 μg/ml) for 24 or 48 h. Live and apoptotic cells were harvested by centrifugation, resuspended in 1 ml propidium iodide (PI) staining buffer (PI 50 μg/ml, sodium citrate 0.1%, Triton X-100 0.1%) and analyzed after an overnight incubation at 4°C. For cell cycle analysis, cells were either prepared as described in Grohen et al.76 or fixed in 80% ethanol at −20°C overnight, washed with PBS, followed by RNase A treatment (100 μg/ml, 5 min) and PI staining (50 μg/ml in PBS). Both quantification of the apoptotic cell fraction as well as cell cycle analysis were performed on a FACS Scan flow cytometer using Cell Quest software (Becton Dickinson).
Hemoglobin content
The hemoglobin content of doxycycline treated and untreated cells was determined spectrophotometrically at 540 nm using a hemoglobin assay kit (Sigma, Deisenhofen). Three million cells were assayed according to the manufacturer's instructions. As positive control for the induction of erythroid differentiation, the same number of K562 cells incubated for 6 days with 2.5 μM Ara-C was analyzed.
Cytospin preparations and immunofluorescence staining
Cells were incubated for 24 h in the presence or absence of doxycycline (1 μg/ml). A total of 30 000 cells in a volume of 100 μl medium were centrifuged onto glass cover slips in a Shandon cytospin centrifuge, air-dried and postfixed in 2% paraformaldehyde/PBS/0.1% Triton X-100. After blocking the cell preparations with SuperBlock (Pierce) for 1 h at RT, HA-tagged p27Kip1 was detected by using an anti-HA-Tag antibody (clone3F10; Roche Diagnostics, Mannheim) and an Alexa 488 conjugated goat–anti-rat antibody (Molecular Probes, Leiden, Netherlands). Nuclei were stained by Hoechst 33342. Photographs were taken with a Zeiss Axiocam digital camera.
Protein assays
For Western blotting experiments, cells were lysed in 1% SDS, 10 mM Tris buffer pH 7.5 and immediately denatured at 95°C for 10 min. Insoluble debris was removed by centrifugation at 14 000 rpm in a microcentrifuge. PARP was extracted by solubilizing cells in M-PER (Pierce) supplemented with 200 mM NaCl. For detection of tyrosine phosphorylated proteins cell extracts were prepared in M-PER, supplemented with 200 mM NaCl, 2 mM vanadate, 1 mM EDTA and one tablet of protease inhibitor cocktail (Roche) per 10 ml buffer. Protein concentrations of all samples were determined by a BCA assay (Sigma). All samples were stored at −20°C until analyzed further.
After SDS–PAGE on homogeneous 7.5, 10 or 12% gels, proteins were transferred to nitrocellulose membranes, blocked with TBST/5% nonfat dry milk powder and probed with primary antibodies followed by incubation with horseradish peroxidase-conjugated secondary antibodies. Signals were generated using the SuperSignal West Pico reagent (Pierce). For densitometric quantification, scanned images were analyzed using MacBas Software (Fuji). Stripping of blot membranes was performed by incubating the membranes in Restore Buffer (Pierce) for 15–30 min at RT, washing in TBST and another blocking step using TBST/5% nonfat dry milk powder.
Determination of caspase activity
Cells were cultivated in the presence or absence of doxycycline (1 μg/ml) for 48 h. A total of 2.5 × 104 cells/well in a volume of 50 μl were then transferred to a 96-well plate and supplemented with an equal volume of medium containing either MG132 (25 μM final concentration) or DMSO (0.1%). After incubation for 15 h, the combined caspases 3 and 7 activity was determined using the ApoOne reagent, according to the manufacturers instructions (Promega), with a fluorescence plate reader (Lambda Fluoro 320; 485 nmEx/530 nmEm) after 3 h of incubation with the caspase substrate at RT.
Abbreviations
- cdk:
-
cyclin-dependent kinase
- cki:
-
cyclin-dependent kinase inhibitor
- DMSO:
-
dimethylsulfoxide
- CML:
-
chronic myeloid leukemia
- PSI:
-
N-carbobenzoxy-L-isoleucyl-L-γ-t-butyl-L-glutamyl-L-alanyl-L-leucinal)
- MG132:
-
(N-carbobenzoxy-L-leucyl-L-leucyl-L-leucinal)
- epoxomicin:
-
(2R)-2-[acetyl-(N-methyl-L-isoleucyl)-L-isoleucyl-L-threonyl-L-leucyl]-2-methyloxirane
References
Hershko A and Ciechanover A . (1998) The ubiquitin system. Annu. Rev. Biochem. 67: 425–479
Rock KL, Gramm C, Rothstein L, Clark K, Stein R, Dick L, Hwang D and Goldberg AL (1994) Inhibitors of the proteasome block the degradation of most cell proteins and the generation of peptides presented on MHC class I molecules. Cell 78: 761–771
Drexler HCA (1997) Activation of the cell death program by inhibition of proteasome function. Proc. Natl. Acad. Sci. USA 94: 855–860
Imajoh-Ohmi S, Kawaguchi T, Sugiyama S, Tanaka K, Omura S and Kikuchi H (1995) Lactacystin, a specific inhibitor of the proteasome, induces apoptosis in human monoblast U937 cells. Biochem. Biophys. Res. Commun. 217: 1070–1077
Fujita T, Ishido S, Muramatsu S, Itoh M and Hotta H (1996) Suppression of actinomycin D-induced apoptosis by the Ns3 protein of hepatitis C virus. Biochem. Biophys. Res. Commun. 229: 825–831
Shinohara K, Tomioka M, Nakano H, Tone S, Ito H and Kawashima S (1996) Apoptosis induction resulting from proteasome inhibition. Biochem. J. 317: 385–388
Tanimoto Y, Onishi Y, Hashimoto S and Kizaki H (1997) Peptidyl aldehyde inhibitors of proteasome induce apoptosis rapidly in mouse lymphoma Rvc cells. J. Biochem. 121: 542–549
An B, Goldfarb RH, Siman R and Dou QP (1998) Novel dipeptidyl proteasome inhibitors overcome Bcl-2 protective function and selectively accumulate the cyclin-dependent kinase inhibitor p27 and induce apoptosis in transformed, but not normal, human fibroblasts. Cell Death Differ. 5: 1062–1075
Dietrich C, Bartsch T, Schanz F, Oesch F and Wieser RJ (1996) p53-dependent cell cycle arrest induced by N-acetyl-L-leucinyl-L-leucinyl-L-norleucinal in platelet-derived growth factor-stimulated human fibroblasts. Proc. Natl. Acad. Sci. USA 93: 10 815–10 819
Lopes UG, Erhardt P, Yao RJ and Cooper GM (1997) p53-dependent induction of apoptosis by proteasome inhibitors. J. Biol. Chem. 272: 12 893–12 896
Blagosklonny MV, Wu GS, Omura S and Eldeiry WS (1996) Proteasome-dependent regulation of p21(Waf1/Cip1) expression. Biochem. Biophys. Res. Comm. 227: 564–569
Cayrol C and Ducommun B (1998) Interaction with cyclin-dependent kinases and PCNA modulates proteasome-dependent degradation of p21. Oncogene 17: 2437–2444
Pagano M, Tam SW, Theodoras AM, Beerromero P, Delsal G, Chau V, Yew PR, Draetta GF and Rolfe M (1995) Role of the ubiquitin–proteasome pathway in regulating abundance of the cyclin-dependent kinase inhibitor p27. Science 269: 682–685
Kisselev AF and Goldberg AL (2001) Proteasome inhibitors: from research tools to drug candidates. Chem. Biol. 8: 739–758
Adams J, Palombella VJ, Sausville EA, Johnson J, Destree A, Lazarus DD, Maas J, Pien CS, Prakash S and Elliott PJ (1999) Proteasome inhibitors: a novel class of potent and effective antitumor agents. Cancer Res. 59: 2615–2622
Sunwoo JB, Chen Z, Dong G, Yeh N, Crowl Bancroft C, Sausville E, Adams J, Elliott P and Van Waes C (2001) Novel proteasome inhibitor PS-341 inhibits activation of Nuclear Factor-kappa B, cell survival, tumor growth, and angiogenesis in squamous cell carcinoma. Clin. Cancer Res. 7: 1419–1428
Hideshima T, Richardson P, Chauhan D, Palombella VJ, Elliott PJ, Adams J and Anderson KC (2001) The proteasome inhibitor PS-341 inhibits growth, induces apoptosis, and overcomes drug resistance in human multiple myeloma cells. Cancer Res. 61: 3071–3076
Sun J, Nam S, Lee CS, Li B, Coppola D, Hamilton AD, Dou QP and Sebti SM (2001) CEP1612, a dipeptidyl proteasome inhibitor, induces p21WAF1 and p27KIP1 expression and apoptosis and inhibits the growth of the human lung adenocarcinoma A-549 in nude mice. Cancer Res. 61: 1280–1284
Sadoul R, Fernandez P-A, Quiquerez A-L, Martinou I, Maki M, Schröter M, Becherer JD, Irmler M, Tschopp J and Martinou J-C (1996) Involvement of the proteasome in the programmed cell death of NGF-deprived sympathetic neurons. EMBO J. 15: 3845–3852
Grimm LM, Goldberg AL, Poirier GG, Schwartz LM and Osborne BA (1996) Proteasomes play an essential role in thymocyte apoptosis. EMBO J. 15: 3835–3844
Drexler HCA, Risau W and Konerding MA (2000) Inhibition of proteasome function induces programmes cell death in proliferating endothelial cells. FASEB J. 14: 65–77
Polyak K, Kato JY, Solomon MJ, Sherr CJ, Massague J, Roberts JM and Koff A (1994) p27Kip1, a cyclin-Cdk inhibitor, links transforming growth factor-beta and contact inhibition to cell cycle arrest. Genes Dev. 8: 9–22
Hirano M, Hirano K, Nishimura J and Kanaide H (2001) Transcriptional up-regulation of p27(Kip1) during contact-induced growth arrest in vascular endothelial cells. Exp. Cell Res. 271: 356–367
Suzuki E, Nagata D, Yoshizumi M, Kakoki M, Goto A, Omata M and Hirata Y (2000) Reentry into the cell cycle of contact-inhibited vascular endothelial cells by a phosphatase inhibitor. Possible involvement of extracellular signal-regulated kinase and phosphatidylinositol 3-kinase. J. Biol. Chem. 275: 3637–3644
Hofmann F, Martelli F, Livingston DM and Wang ZY (1996) The retinoblastoma gene product protects E2f-1 from degradation by the ubiquitin-proteasome pathway. Genes Dev. 10: 2949–2959
McGahon A, Bissonnette R, Schmitt M, Cotter KM, Green DR and Cotter TG (1994) BCR-ABL maintains resistance of chronic myelogenous leukemia cells to apoptotic cell death. Blood 83: 1179–1187
Benito A, Silva M, Grillot D, Nunez G and Fernandez-Luna JL (1996) Apoptosis induced by erythroid differentiation of human leukemia cell lines is inhibited by Bcl-xL. Blood 87: 3837–3843
Jonuleit T, van der Kuip H, Miething C, Michels H, Hallek M, Duyster J and Aulitzky WE (2000) Bcr-Abl kinase down-regulates cyclin-dependent kinase inhibitor p27 in human and murine cell lines. Blood 96: 1933–1939
Gesbert F, Sellers WR, Signoretti S, Loda M and Griffin JD (2000) BCR/ABL regulates expression of the cyclin-dependent kinase inhibitor p27Kip1 through the phosphatidylinositol 3-Kinase/AKT pathway. J. Biol. Chem. 275: 39 223–39 230
Dan S, Naito M and Tsuruo T (1998) Selective induction of apoptosis in Philadelphia chromosome-positive chronic myelogenous leukemia cells by an inhibitor of BCR-ABL tyrosine kinase, CGP 57148. Cell Death Differ. 5: 710–715
Pendergast AM, Quilliam LA, Cripe LD, Bassing CH, Dai Z, Li N, Batzer A, Rabun KM, Der CJ, Schlessinger J et al. (1993) BCR-ABL-induced oncogenesis is mediated by direct interaction with the SH2 domain of the GRB-2 adaptor protein. Cell 75: 175–185
Shuai K, Halpern J, ten Hoeve J, Rao X and Sawyers CL (1996) Constitutive activation of STAT5 by the BCR-ABL oncogene in chronic myelogenous leukemia. Oncogene 13: 247–254
Skorski T, Kanakaraj P, Nieborowska-Skorska M, Ratajczak MZ, Wen SC, Zon G, Gewirtz AM, Perussia B and Calabretta B (1995) Phosphatidylinositol-3 kinase activity is regulated by BCR/ABL and is required for the growth of Philadelphia chromosome-positive cells. Blood 86: 726–736
Gotoh A, Miyazawa K, Ohyashiki K, Tauchi T, Boswell HS, Broxmeyer HE and, Toyama K (1995) Tyrosine phosphorylation and activation of focal adhesion kinase (p125FAK) by BCR-ABL oncoprotein. Exp. Hematol. 23: 1153–1159
Sawyers CL, Callahan W and Witte ON (1992) Dominant negative MYC blocks transformation by ABL oncogenes. Cell 70: 901–910
Mandanas RA, Boswell HS, Lu L and Leibowitz D (1992) BCR/ABL confers growth factor independence upon a murine myeloid cell line. Leukemia 6: 796–800
Katayose Y, Kim M, Rakkar ANS, Li ZW, Cowan KH and Seth P (1997) Promoting apoptosis – a novel activity associated with the cyclin-dependent kinase inhibitor p27. Cancer Res. 57: 5441–5445
Wang X, Gorospe M, Huang Y and Holbrook NJ (1997) p27Kip1 overexpression causes apoptotic death of mammalian cells. Oncogene 15: 2991–2997
Schreiber M, Muller WJ, Singh G and Graham FL (1999) Comparison of the effectiveness of adenovirus vectors expressing cyclin kinase inhibitors p16INK4A, p18INK4C, p19INK4D, p21(WAF1/CIP1) and p27KIP1 in inducing cell cycle arrest, apoptosis and inhibition of tumorigenicity. Oncogene 18: 1663–1676
Kudo Y, Takata T, Ogawa I, Kaneda T, Sato S, Takekoshi T, Zhao M, Miyauchi M and Nikai H (2000) p27Kip1 accumulation by inhibition of proteasome function induces apoptosis in oral squamous cell carcinoma cells. Clin. Cancer Res. 6: 916–923
An B, Goldfarb RH, Siman R and Dou QP (1998) Novel dipeptidyl proteasome inhibitors overcome Bcl-2 protective function and selectively accumulate the cyclin-dependent kinase inhibitor p27 and induce apoptosis in transformed, but not normal, human fibroblasts. Cell Death Differ. 5: 1062–1075
Kobayashi T, Ruan SB, Clodi K, Kliche KO, Shiku H, Andreeff M and Zhang W (1998) Overexpression of bax gene sensitizes K562 erythroleukemia cells to apoptosis induced by selective chemotherapeutic agents. Oncogene 16: 1587–1591
Cummings M, Siitonen T, Higginbottom K, Newland AC and Allen PD (2002) p53-mediated downregulation of Chk1 abrogates the DNA damage-induced G2 M checkpoint in K562 cells, resulting in increased apoptosis. Br. J. Haematol. 116: 421–428
Di Bacco AM and Cotter TG (2002) p53 expression in K562 cells is associated with caspase-mediated cleavage of c-ABL and BCR-ABL protein kinases. Br. J. Haematol. 117: 588–597
Kobayashi T, Sawa H, Morikawa J, Ueno S, Katayama N, Zhang W and Shiku H (2002) Bax-induction alone is sufficient to activate apoptosis cascade in wild-type Bax-bearing K562 cells, and the initiation of apoptosis requires simultaneous caspase activation. Int. J. Oncol. 20: 723–728
Ray S, Bullock G, Nunez G, Tang C, Ibrado AM, Huang Y and Bhalla K (1996) Enforced expression of Bcl-XS induces differentiation and sensitizes chronic myelogenous leukemia-blast crisis K562 cells to 1-beta-D-arabinofuranosylcytosine-mediated differentiation and apoptosis. Cell Growth Differ. 7: 1617–1623
Schimmer AD, Hedley DW, Pham NA, Chow S and Minden MD (2001) BAD induces apoptosis in cells over-expressing Bcl-2 or Bcl-xL without loss of mitochondrial membrane potential. Leuk. Lymphoma 42: 429–443
Amati B, Littlewood TD, Evan GI and Land H (1993) The c-Myc protein induces cell cycle progression and apoptosis through dimerization with Max. EMBO J. 12: 5083–5087
Leppa S and Bohmann D (1999) Diverse functions of JNK signaling and c-Jun in stress response and apoptosis. Oncogene 18: 6158–6162
Treier M, Staszewski LM and Bohmann D (1994) Ubiquitin-dependent c-Jun degradation in vivo is mediated by the delta domain. Cell 78: 787–798
Salghetti SE, Muratani M, Wijnen H, Futcher B and Tansey WP (2000) Functional overlap of sequences that activate transcription and signal ubiquitin-mediated proteolysis. Proc. Natl. Acad. Sci. USA 97: 3118–3123
Evan GI, Wyllie AH, Gilbert CS, Littlewood TD, Land H, Brooks M, Waters CM, Penn LZ, and, Hancock DC (1992) Induction of apoptosis in fibroblasts by c-Myc protein. Cell 69: 119–128
Tani E, Kitagawa H, Ikemoto H and Matsumoto T (2001) Proteasome inhibitors induce Fas-mediated apoptosis by c-Myc accumulation and subsequent induction of FasL message in human glioma cells. FEBS Lett. 504: 53–58
Bedi A, Zehnbauer BA, Barber JP, Sharkis SJ and Jones RJ (1994) Inhibition of apoptosis by BCR-ABL in chronic myeloid leukemia. Blood 83: 2038–2044
Skorski T, Nieborowska-Skorska M, Wlodarski P, Perrotti D, Hoser G, Kawiak J, Majewski M, Christensen L, Iozzo RV and Calabretta B (1997) Treatment of Philadelphia leukemia in severe combined immunodeficient mice by combination of cyclophosphamide and BCR/ABL antisense oligodeoxynucleotides. J. Natl. Cancer Inst. 89: 124–133
Druker BJ, Sawyers CL, Kantarjian H, Resta DJ, Reese SF, Ford JM, Capdeville R and Talpaz M (2001) Activity of a specific inhibitor of the BCR-ABL tyrosine kinase in the blast crisis of chronic myeloid leukemia and acute lymphoblastic leukemia with the Philadelphia chromosome. N. Engl. J. Med. 344: 1038–1042
Druker BJ, Talpaz M, Resta DJ, Peng B, Buchdunger E, Ford JM, Lydon NB, Kantarjian H, Capdeville R, Ohno-Jones S et al. (2001) Efficacy and safety of a specific inhibitor of the BCR-ABL tyrosine kinase in chronic myeloid leukemia. N. Engl. J. Med. 344: 1031–1037
Gorre ME, Mohammed M, Ellwood K, Hsu N, Paquette R, Rao PN and Sawyers CL (2001) Clinical resistance to STI-571 cancer therapy caused by BCR-ABL gene mutation or amplification. Science 293: 876–880
le Coutre P, Tassi E, Varella-Garcia M, Barni R, Mologni L, Cabrita G, Marchesi E, Supino R and Gambacorti-Passerini C (2000) Induction of resistance to the Abelson inhibitor STI571 in human leukemic cells through gene amplification. Blood 95: 1758–1766
Mahon FX, Deininger MW, Schultheis B, Chabrol J, Reiffers J, Goldman JM and Melo JV (2000) Selection and characterization of BCR-ABL positive cell lines with differential sensitivity to the tyrosine kinase inhibitor STI571: diverse mechanisms of resistance. Blood 96: 1070–1079
Weisberg E and Griffin JD (2000) Mechanism of resistance to the ABL tyrosine kinase inhibitor STI571 in BCR/ABL-transformed hematopoietic cell lines. Blood 95: 3498–3505
Naujokat C, Sezer O, Zinke H, Leclere A, Hauptmann S and Possinger K (2000) Proteasome inhibitors induced caspase-dependent apoptosis and accumulation of p21WAF1/Cip1 in human immature leukemic cells. Eur. J. Haematol. 65: 221–236
Soligo D, Servida F, Delia D, Fontanella E, Lamorte G, Caneva L, Fumiatti R and Lambertenghi Deliliers G (2001) The apoptogenic response of human myeloid leukaemia cell lines and of normal and malignant haematopoietic progenitor cells to the proteasome inhibitor PSI. Br. J. Haematol. 113: 126–135
Adams J, Palombella VJ, Sausville EA, Johnson J, Destree A, Lazarus DD, Maas J, Pien CS, Prakash S and Elliott PJ (1999) Proteasome inhibitors: A novel class of potent and effective antitumor agents. Cancer Res. 59: 2615–2622
Loda M, Cukor B, Tam SW, Lavin P, Fiorentino M, Draetta GF, Jessup JM and Pagano M (1997) Increased proteasome-dependent degradation of the cyclin-dependent kinase inhibitor p27 in aggressive colorectal carcinomas. Nat. Med. 3: 231–234
Porter PL, Malone KE, Heagerty PJ, Alexander GM, Gatti LA, Firpo EJ, Daling JR and Roberts JM (1997) Expression of cell-cycle regulators p27Kip1 and cyclin E, alone and in combination, correlate with survival in young breast cancer patients. Nat. Med. 3: 222–225
Catzavelos C, Bhatacharya N, Ung YC, Wilson JA, Roncari L, Sandhu C, Shaw P, Yeger H, Moravaprotzner I, Kapusta L et al. (1997) Decreased levels of the cell-cycle inhibitor p27(Kip1) protein – prognostic implications in primary breast cancer. Nat. Med. 3: 227–230
Catzavelos C, Tsao MS, DeBoer G, Bhattacharya N, Shepherd FA and Slingerland JM (1999) Reduced expression of the cell cycle inhibitor p27(Kip1) in non-small cell lung carcinoma: a prognostic factor independent of ras. Cancer Res. 59: 684–688
Fero ML, Rivkin M, Tasch M, Porter P, Carow CE, Firpo E, Polyak K, Tsai LH, Broudy V, Perlmutter RM et al. (1996) A syndrome of multiorgan hyperplasia with features of gigantism, tumorigenesis, and female sterility in p27(Kip1)-deficient mice. Cell 85: 733–744
Nakayama K, Ishida N, Shirane M, Inomata A, Inoue T, Shishido N, Horii I and Loh DY (1996) Mice lacking p27(Kip1) display increased body size, multiple organ hyperplasia, retinal dysplasia, and pituitary tumors. Cell 85: 707–720
St. Croix B, Florenes VA, Rak JW, Flanagan M, Bhattacharya N, Slingerland JM and Kerbel RS (1996) Impact of the cyclin-dependent kinase inhibitor p27Kip1 on resistance of tumor cells to anticancer agents. Nat. Med. 2: 1204–1210
Eymin B, Haugg M, Droin N, Sordet O, Dimanche-Boitrel MT and Solary E (1999) p27(Kip1) induces drug resistance by preventing apoptosis upstream of cytochrome c release and procaspase-3 activation in leukemic cells. Oncogene 18: 1411–1418
Dimanche-Boitrel MT, Micheau O, France D, Hammann A, Duchamp O, Genne P and Solary E (2000) p27(Kip1) overexpression inhibits the growth and doxorubicin sensitivity of HT29 human colon cancer cells in vivo. Anticancer Res. 20: 849–852
Hiromura K, Pippin JW, Fero ML, Roberts JM and Shankland SJ (1999) Modulation of apoptosis by the cyclin-dependent kinase inhibitor p27(Kip1). J. Clin. Invest. 103: 597–604
Achenbach TV, Muller R and Slater EP (2000) Synergistic antitumor effect of chemotherapy and antisense-mediated ablation of the cell cycle inhibitor p27(Kip-1). Clin. Cancer Res. 6: 3006–3014
Graham SM, Jorgensen HG, Allan E, Pearson C, Alcorn MJ, Richmond L and Holyoake TL (2002) Primitive, quiescent, Philadelphia-positive stem cells from patients with chronic myeloid leukemia are insensitive to STI571 in vitro. Blood 99: 319–325
Park KH, Seol JY, Kim TY, Yoo CG, Kim YW, Han SK, Shim YS and Lee CT (2001) An adenovirus expressing mutant p27 showed more potent antitumor effects than adenovirus-p27 wild type. Cancer Res. 61: 6163–6169
Naruse I, Hoshino H, Dobashi K, Minato K, Saito R and Mori M (2000) Over-expression of p27Kip1 induces growth arrest and apoptosis mediated by changes of pRb expression in lung cancer cell lines. Int. J. Cancer 88: 377–383
Nicoletti I, Migliorati G, Pagliacci MC, Grignani F and Riccardi C (1991) A rapid and simple method for measuring thymocyte apoptosis by propidium iodide staining and flow cytometry. J. Immunol. Methods 139: 271–279
Acknowledgements
We are indebted to R Steinman for providing p21Waf1 inducible K562 cells. We also thank H Land, H Bujard and B Winkler for providing plasmids, and we gratefully acknowledge the technical assistance of S Heinz. We are also grateful to U Deutsch for advice during the vector construction period, and to F Kiefer and M Clauss for critically reading the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Edited by G. Cohen
Rights and permissions
About this article
Cite this article
Drexler, H., Pebler, S. Inducible p27Kip1 expression inhibits proliferation of K562 cells and protects against apoptosis induction by proteasome inhibitors. Cell Death Differ 10, 290–301 (2003). https://doi.org/10.1038/sj.cdd.4401159
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cdd.4401159
Keywords
This article is cited by
-
Cell-cycle arrest in mature adipocytes impairs BAT development but not WAT browning, and reduces adaptive thermogenesis in mice
Scientific Reports (2017)
-
The novel protective role of P27 in MLN4924-treated gastric cancer cells
Cell Death & Disease (2015)
-
Gene delivery of cyclin-dependent kinase inhibitors p21 Waf1 and p27 Kip1 suppresses proliferation of MCF-7 breast cancer cells in vitro
Breast Cancer (2014)
-
Resveratrol protects leukemic cells against cytotoxicity induced by proteasome inhibitors via induction of FOXO1 and p27Kip1
BMC Cancer (2011)
-
Histone deacetylase inhibitors and hydroxyurea modulate the cell cycle and cooperatively induce apoptosis
Oncogene (2008)