Abstract
Typing somatostatin receptor expression in neuroendocrine tumors is of relevance to target somatostatin analogue-based diagnostic approach and treatment. The expanding use of immunohistochemistry to detect somatostatin receptors is to date not paralleled by an accurate methodological setting and standardized interpretation of the results. A multicentric study was designed to compare somatostatin receptor immunohistochemical expression with in vivo scintigraphic data and verify its usefulness in the clinical management of neuroendocrine tumors. After methodological setting by testing different somatostatin receptor antibodies, 107 cases of neuroendocrine tumors with available somatostatin receptor scintigraphy data and pathological material were retrospectively analyzed for somatostatin receptor types 2A, 3 and 5 immunohistochemical expression, and compared with scintigraphic images and, whenever available, with the clinical response to somatostatin analogue treatment. Restricting ‘positive cases’ to the presence of a membrane pattern of staining, an overall somatostatin receptor type 2A immunohistochemistry/somatostatin receptor scintigraphy agreement of 77% (χ2 test P<0.0001) was reached. Lower concordance ratios were detected in preoperative and metastatic tumor samples, possibly as a consequence of somatostatin receptor expression heterogeneity. Pure somatostatin receptor type 2A cytoplasmic staining showed poor correlation with somatostatin receptor scintigraphy (54% concordance rate). The immunohistochemical detection of somatostatin receptor types 3 and 5, which showed almost exclusively a cytoplasmic pattern, did not improve the concordance with scintigraphic data. In a pilot series, somatostatin receptor type 2A immunohistochemistry correlated with clinical response in 75% of cases. In conclusion, we propose a scoring system for somatostatin receptor type 2A immunohistochemistry in neuroendocrine tumors correlated with in vivo data, based on the evidence that only membrane (rather that cytoplasmic) staining should be considered for a reliable, standardized and clinically relevant report.
Similar content being viewed by others
Main
Neuroendocrine tumors belong to a spectrum of lesions with variable degree of differentiation and have various locations and various disease stages: carcinoids (benign and malignant or typical and atypical) lie in the well differentiated extreme of the spectrum, while small and large cell neuroendocrine carcinomas represent the poorly differentiated variants.1, 2
There are several therapeutic options for neuroendocrine tumors. Apart from surgery, chemotherapy and biotherapy are generally the first line treatments. The latter includes in both functioning and non-functioning neuroendocrine tumors somatostatin analogue administration, both in medical treatment and as radio-labeled agents, and interferon.3, 4, 5
Somatostatin is an acidic polypeptide that is widely distributed throughout the central nervous system and different peripheral tissues and organs. Several biological functions related to somatostatin have been described, and include potent inhibition of basal and stimulated secretion from a wide variety of endocrine and exocrine cells, neuromodulatory actions in the central nervous system6, 7, 8, 9 as well as regulatory properties on cell proliferation and differentiation.10 The physiological actions of somatostatin are initiated by its interaction with a family of specific membrane-bound receptors, the somatostatin receptors family, which encompass to date five different subtypes, named somatostatin receptors types 1–5, displaying a remarkable degree of structural conservation across species (40–60% structural homologies), but mediating different biological actions of somatostatin, via the activation of different intracellular signaling pathways.11, 12
The rationale for somatostatin analogue (eg octreotide) treatment is the presence of somatostatin receptors on the surface of tumor cells. These bind octreotide with different degrees of affinity, being somatostatin receptors types 2, 3 and 5 those mostly involved in octreotide binding.
In the clinical practice, the presence of functional somatostatin receptors is documented by somatostatin receptor scintigraphy by 111In-pentetreotide: if positive, a binding of the radioligand with one or more of the somatostatin receptors is demonstrated. Unfortunately, this technique does not identify the receptor type and—most importantly—does not determine the cell population containing the binding sites (tumor cells vs other intratumoral cell types). Various methods to detect somatostatin receptors in tumor specimens were reported, including autoradiography, RT-PCR, in situ hybridization, immunoblotting and immunohistochemistry. Several studies have documented that generally these methods correlate each other in somatostatin receptors positive cases, with only minor discrepancies.13, 14, 15, 16, 17, 18, 19, 20, 21, 22
The currently available somatostatin analogues bind preferentially somatostatin receptors type 2 (which is the most widely expressed subtype in neuroendocrine tumors) and to a lower extent types 3 and 5, and somatostatin receptors profiling in individual patients may be of relevance to better tailor the somatostatin analogue-based treatment. This would hopefully allow to increase the response rate of each patient and reduce costs of biotherapy, which are generally high.
Immunohistochemistry is a cheap, reproducible, and easily accessible procedure that can be performed in most pathology laboratories on fresh and also archival tissue samples. Commercially available antibodies specific for the different receptor subtypes are currently available, but they need to be validated in the clinical practice. No data exist in fact on the quantification and interpretation of somatostatin receptor immunohistochemical findings, although scoring systems have been developed and applied for many years in the analysis of several other receptors (eg estrogen receptor, c-erb-b2, etc).
Aim of the present study is therefore to define the somatostatin receptors immunohistochemical profile in a large series of neuroendocrine tumors of which surgical and/or biopsy material were available, and compare the results with the in vivo data on 111In-pentetreotide scintigraphy and response to somatostatin analogue treatment.
Materials and methods
Case Selection
A series of 107 neuroendocrine tumors (from years 1998 to 2006) treated in three different highly specialized Italian centers of the Universities of Turin, Naples and Varese was selected according to the following criteria: (i) revised histopathological diagnosis; (ii) tissue material available for pathological review and immunohistochemistry; (iii) 111In-pentetreotide scintigraphy data available.
For most cases, medical treatment administered, response to treatment (as progressive disease, partial remission or stable disease) and follow-up data were also accessible.
Somatostatin receptor scintigraphy was performed preoperatively in all but seven patients, who had post-surgical somatostatin receptor scintigraphy in the presence of residual disease. 111Indium-DTPA0-octreotide (135 MBq) was administered immediately after checking the specific radiochemical purity by chromatography, which was always higher than 95%. The scintigraphic procedure included 4- and 24-h planar anterior and posterior images (matrix size 128 × 128) of the chest, upper and lower abdomen and anterior views of the head and proximal lower legs. At least 500 Kilocounts were recorded over the chest and abdomen and 50–200 Kilocounts were obtained for the head and neck and lower leg views. SPECF of the abdomen was performed 24 h after injection. Sixty-four 40-s views (matrix size: 64 × 64) were acquired through a 360° arc. Planar and SPECF images were acquired using a large field of view γ camera equipped with a medium-energy, general-purpose collimator. Somatostatin receptor scintigraphy images were scored in four groups according to Kwekkeboom et al.23
The tissue material corresponded to 41 preoperative samples (fine-needle aspiration or core biopsies) and 66 surgical samples. All surgical samples were fixed in buffered formalin; preoperative samples were both fixed in formalin or in alcohol. All cases have been reviewed and diagnosed according to years 2000 and 2004 WHO classifications of Endocrine Tumors.1, 2 They included 70 cases of well-differentiated neuroendocrine tumors (benign carcinoids) or carcinomas (malignant/atypical carcinoids) (63 cases from lung, pancreas and gastrointestinal tract, and 7 cases of liver or lymph node metastases in the absence of evident primary disease), 18 cases of poorly differentiated neuroendocrine carcinomas (mainly from lung), 9 cases of medullary thyroid carcinomas and 7 additional cases of neuroendocrine tumors from skin, paraganglia, thymus and pituitary, as well as 3 cases of adenocarcinomas with neuroendocrine differentiation of the breast and prostate. In 31 cases, tissue material was obtained from metastatic deposits, and in 3 of these cases primary and metastatic lesions from the same patient could be compared. The study was approved by the Local Ethic Committee.
Immunohistochemistry
Serial 5-μm thick paraffin sections were collected onto charged slides and processed by immunohistochemistry in a single Institution (Orbassano, Turin, Italy). In a pilot series of 20 neuroendocrine tumors, as well as in control sections of normal pancreatic tissue, alternative polyclonal somatostatin receptor type 2A antibodies (BioTrend, Cologne, Germany, code SS-800; Santa Cruz Biotechnology, Santa Cruz, CA, USA, code sc-25676; LifeSpan Biosciences, Seattle WA, USA, code LS-A998) were tested. Although all three somatostatin receptor type 2A antibodies were comparable in the majority of normal and neoplastic specimens in terms of staining intensity, in our laboratory protocols BioTrend antibody appeared to be more sensitive as compared to the others, in terms of both presence of positive internal reference controls (ie blood vessels) and demonstration of a membranous staining pattern in normal and neoplastic cell populations. It was therefore selected to be applied to the complete series of cases and for comparison with in vivo data. Pre-absorption experiments, performed in control sections by pre-incubation of the primary antibody with a 10- to 50-fold excess of blocking peptide (BioTrend, code SS-801), could confirm the specificity of such antibody. Negative control experiments by somatostatin receptor type 2A pre-absorption were therefore performed in each immunohistochemical run. In addition, polyclonal antibodies to somatostatin receptor types 3 and 5 from three different sources (BioTrend, codes SS-830 and SS-838, LifeSpan, codes LS-A2622 and LS-A2639, and Abcam, Cambridge, UK, codes ab28680 and ab28618, for subtypes 3 and 5, respectively) were also tested in the pilot series of 20 cases of neuroendocrine tumors. According to the preliminary immunohistochemical findings, Abcam antibodies demonstrated the most intense and reliable results and were therefore employed on the whole case series. Moreover, pre-absorption experiments for BioTrend somatostatin receptor types 3 and 5 antibodies, using the same conditions as for somatostatin receptor type 2A (blocking peptides from BioTrend, codes SS-831 and SS-839-A, respectively) failed to confirm the specificity of these latter primary antibodies, even applying different batches.
For somatostatin receptor immunohistochemistry the following conditions were applied: antigen retrieval was performed in pH 6.0 citrate buffer in a microwave oven (three cycles 5 min each at 750 W) and the primary antibodies were incubated for 4 h at 37°C. Primary antibodies dilutions were 1/3000, 1/1000 and 1/500 for somatostatin receptor types 2A, 3 and 5. Immunoreactions were revealed by a biotin-free dextran-chain detection system (Envision, DakoCytomation, Glostrup, Denmark), and developed using diaminobenzidine as the chromogen. The specificity was also validated in parallel negative control sections by omitting the primary antibodies for each immunohistochemical run.
All somatostatin receptor immunohistochemical findings were analyzed independently by two observers (MV and IR) in one center (Orbassano, Turin, Italy).
In 14 selected cases, somatostatin receptor type 2A immunohistochemistry was repeated in a different laboratory (Varese) following the same working conditions, and the results checked to test inter-laboratory agreement.
Somatostatin Receptor Immunohistochemistry Scoring System
For somatostatin receptor type 2A a semiquantitative scoring system was designed, taking into consideration both the subcellular localization and the extent of the staining, as follows: score 0: absence of immunoreactivity; score 1: pure cytoplasmic immunoreactivity, either focal or diffuse; score 2: membranous reactivity in less than 50% of tumor cells, irrespective of the presence of cytoplasmic staining; score 3: circumferential membranous reactivity in more than 50% of tumor cells, irrespective of the presence of cytoplasmic staining.
For somatostatin receptor types 3 and 5, a cytoplasmic pattern of staining only was observed, and cases were scored as positive in the presence of at least 10% of positive tumor cells.
Response to Treatment
Tumor responses was classified according to the RECIST criteria.24 Complete response was defined as the absence of radiologically documented lesions. A partial response was defined as at least a 30% decrease in the sum of the longitudinal diameter of target lesions. Progressive disease was defined as at least a 20% increase in the sum of the longitudinal diameter of target lesions or the appearance of one or more new lesions. Stable disease was defined as neither a sufficient shrinkage to qualify for partial response, nor sufficient increase to qualify for progression disease.
Statistical Analysis
Immunohistochemical results were compared to somatostatin receptor scintigraphy status and available clinico-pathological parameters by χ2 test using 1 degree of freedom (d.f.=1), and a level of statistical significance of P=0.05. For statistical comparison, somatostatin receptor type 2A immunohistochemical scores 0 and 1 were considered negative, as opposed to scores 2 and 3 (see also below).
Results
Somatostatin Receptors Distribution in Neuroendocrine Tumors
Immunohistochemistry
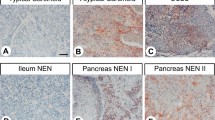
Somatostatin receptor types 2A, 3 and 5 antibodies showed the specific signal in internal reference controls (ie blood vessels, pancreatic islets) or in control sections of both formalin- and alcohol-fixed tissue samples. In the case of somatostatin receptor type 2A, pre-absorption experiments abolished the immunoreactivity (both membranous and cytoplasmic patterns) and confirmed the specificity of the reaction (Figure 1). Grouping somatostatin receptor type 2A immunohistochemical scores 2 and 3 together as positive (see also below), somatostatin receptor type 2A was detected in 79% of well-differentiated neuroendocrine tumors/carcinomas and in 44% of poorly differentiated neuroendocrine carcinomas (Table 1). In somatostatin receptor type 2A score 1 cases, the cytoplasmic reactivity was generally weak to moderate; comparing scores 2 and 3, apart from the percentage of positive tumor cells which determined the inclusion in one or the other group, a slightly weaker and often incomplete membrane staining was observed in score 2 cases, whereas a strong and circumferential membranous pattern was characteristic of score 3 cases (Figures 2 and 3). Inter-observer cross validation between the two independent investigators (MV and IR) was up to 98%; for discrepant cases agreement was reached by reviewing the slides at a multihead microscope. Inter-laboratory cross validation (between the slides stained in Orbassano and in Varese) showed 100% scoring agreement in all 14 cases tested.
Representative illustration of somatostatin receptor type 2A immunohistochemical scores in surgical (left-sided pictures; (a) lymph node metastasis of medullary thyroid carcinoma; (c) atypical carcinoid of the lung, (e) well-differentiated neuroendocrine carcinoma of the pancreas, not functioning) and preoperative cytological (right-sided pictures; (b) liver metastasis of well-differentiated neuroendocrine carcinoma of the pancreas; (d) lymph node metastasis of well-differentiated neuroendocrine carcinoma, primary unknown; (f) liver metastasis of well-differentiated neuroendocrine carcinoma of the small ileum) samples. The lesions represented included: (a, b) Score 1 (a and b) included pure cytoplasmic reactivity, either moderate/strong (a) or weak (b). Score 2 (c and d) was considered in the presence of a membranous pattern of staining in less than 50% of tumors cells, either in scattered cells with complete membrane outlining (c) or with partial membrane staining in most tumor cells (d). Score 3 was clearly recognizable by a membranous, usually intense, staining in more than 50% of tumors cells (e and f).
Somatostatin receptor types 3 and 5 showed a cytoplasmic pattern only, with very occasional membrane reinforcement. They were positive in 44 and 71% of well-differentiated neuroendocrine tumors/carcinomas and in 17 and 28% of poorly differentiated neuroendocrine carcinomas, respectively for types 3 and 5 (Table 1).
Somatostatin receptor scintigraphy
In vivo somatostatin receptor analysis by 111In-pentetreotide detected positive binding (including scores 2–4 according to Kwekkeboom et al23 in 78/107 cases (73%), with a decreasing percentage of positive cases comparing well-differentiated lesions (79%), poorly differentiated neuroendocrine carcinomas (44%) and the group miscellaneous neuroendocrine tumors (21%).
Correlation of Immunohistochemistry with In Vivo Data
When checking the correlation of somatostatin receptor type 2A antibody reactivity with in vivo data among the different immunohistochemical groups, scores 2 and 3 showed a high concordance with somatostatin receptor scintigraphy, being correlated to scintigraphic positivity in 87 and 94% of cases, respectively, and were grouped together for further statistical comparison. By contrast, immunohistochemical scores 0 and 1 showed a poor correlation with somatostatin receptor scintigraphy results, and therefore were grouped together as negative for further statistical analysis (Figure 3).
An overall somatostatin receptor type 2A immunohistochemistry/somatostatin receptor scintigraphy agreement of 77% (82/107 cases, χ2 P<0.0001) was reached (Table 2). Among the 82 concordant cases, 61 were both methods positive (Figure 4a–c) and 21 were both methods negative. Consistent concordance rates were observed in the group of well-differentiated (79%, χ2 P=0.05) and poorly differentiated (94%, χ2 P<0.0001) neoplasms. Conversely, considering individual tumor locations, a low concordance rate was observed in the case of medullary thyroid carcinomas and occult primary neuroendocrine carcinomas (67 and 54% immunohistochemistry/somatostatin receptor scintigraphy agreement, respectively). The latter group showed mainly an immunohistochemistry negative/somatostatin receptor scintigraphy positive profile (Figure 4d–f).
Fine-needle aspiration biopsy of a liver metastasis from a well-differentiated pancreatic neuroendocrine carcinoma (a) strongly expressing somatostatin receptor type 2A by immunohistochemistry (b, immunohistochemical score 3) and clearly visible by 111In-pentetreotide scintigraphy (c). By contrast, a case of fine-needle aspiration biopsy of a para-caval lymph node metastasis from a well-differentiated neuroendocrine carcinoma of primary unknown origin (d) showing discrepant results between negative immunohistochemistry (e, immunohistochemical score 1) and positive scintigraphy (f).
A rather poor correlation was observed in the group of preoperative biopsy samples (73% immunohistochemistry/somatostatin receptor scintigraphy agreement, χ2 P=0.09) and in patients from whom metastatic tumor samples were available (65% immunohistochemistry/somatostatin receptor scintigraphy agreement, χ2 P=0.3).
When correlating scintigraphic data with all three somatostatin receptor antibodies, the overall agreement in the presence of at least one positive somatostatin receptor type did not change (82/107 cases, 77%), whereas an increase of immunohistochemistry positive/scintigraphy negative cases was observed (with a loss of ‘specificity’ if considering 111In-pentetreotide scintigraphy the reference method; Table 3). In 28 patients, all bearing well-differentiated neuroendocrine carcinomas from pancreas and gastrointestinal tract or unknown origin, homogeneous somatostatin analogue treatment was administered until progression, consisting in intramuscular injection of the long-acting release octreotide (octreotide L-A-R) at a dose of 20 mg every 28 days. Immunohistochemical somatostatin receptor type 2A status correlated to response to treatment in 75% of cases (21/28); among these 21 concordant cases, 16 patients had a disease stabilization and 2 cases had a partial response to treatment in the presence of somatostatin receptor type 2A immunoreactivity, whereas the 3 remaining cases, negative to somatostatin receptor type 2A immunohistochemistry, had disease progression. By contrast, all seven discordant cases had disease progression in spite of somatostatin receptor type 2 protein immunohistochemical expression.
Discussion
The wide expression of somatostatin receptors in neuroendocrine tumors has been largely investigated and led nowadays to the development of clinically relevant diagnostic and therapeutic strategies.25 However, which methodology could better determine the somatostatin receptor status of a given tumor and could predict its possible visualization by somatostatin receptor scintigraphy and response to somatostatin-analogue therapy is far from being settled in the clinical practice. At present for the clinicians, somatostatin receptor scintigraphy remains the golden standard method to detect somatostatin receptors. In fact, octreotide scintigraphy provides information on the whole tumor mass including metastases and its signal intensity is used for radiotherapeutic decisions.23 Among alternative methods, immunohistochemistry seems to be a reliable tool to detect the somatostatin receptor profile in neuroendocrine tumors, due to the following advantages: detection of the receptor protein (instead of RNA, for example in PCR-based methods), possibility of detecting the cellular type expressing the receptor (neoplastic cells vs blood vessels or reactive lymphocytes, etc), availability of subtype specific antibodies, applicability in archival material, low cost/benefit ratio which renders this method applicable in most laboratories.13, 15, 16, 17, 19, 21 On the contrary, major disadvantages are related to the lack of standardization of the method (from both technical and interpretation viewpoints) which is a great limitation in diagnostic applications, the failure of demonstrating ‘functional’ receptors (as opposed to autoradiography), and undetermined sensitivity of the technique, since limited evidence has been reported on the correlation between immunohistochemistry and other in vivo techniques. In a recent paper, Korner et al15 tested different somatostatin receptor type 2A antibodies in different human tumors, and correlated the immunohistochemical pattern with previous autoradiographic data on 37 cases, demonstrating a good correlation between the two methods applying the same antibody selected in our study. Previous reports testing somatostatin receptor immunohistochemistry in lung18 and gastrointestinal16 neuroendocrine tumors and in pheochromocytomas17 in correlation to somatostatin receptor scintigraphy are limited by the relative low number of cases compared and by a general lack of standardization of the immunohistochemical interpretation (ie membranous vs cytoplasmic pattern). Therefore, we designed the present study on a large multicentric series of neuroendocrine tumors to validate the reproducibility of the immunohistochemical method and to compare the results with somatostatin receptor scintigraphy imaging.
As a first aim, a practical immunohistochemical scoring system for the most common somatostatin receptor subtype—namely type 2A—based on the percentage of positive tumor cells and the pattern of staining was proposed and assessed. The correlation with 111In-pentetreotide scintigraphy data indicate that the higher concordance rates were achieved only when a membranous pattern of staining was observed (corresponding to scores 2 and 3), whereas pure cytoplasmic staining (score 1) presented a rather poor and random concordance rate and was therefore considered as negative for further analysis. Although ‘functional’ mechanisms for somatostatin receptor type 2A cytoplasmic positivity (ie receptor internalization) have been discussed in the literature,26 it might be speculated that in the diagnostic practice careful search for membranous pattern (associated or not with a faint cytoplasmic pattern) should be pursued to define a positive staining. The same consideration should be deserved for somatostatin receptor types 3 and 5 antibodies, which showed almost exclusively a cytoplasmic pattern of staining, and which did not improve significantly the capability of somatostatin receptor type 2A alone to correlate with octreotide scintigraphy.
Immunohistochemical somatostatin receptor type 2A scores 2 and 3 were higher, as expected, in well-differentiated neuroendocrine tumor/carcinoma group as compared to poorly differentiated carcinomas (Table 1), without significant differences considering the organs of origin, except for the cases of metastatic samples of unknown primary origin which showed a lower rate of somatostatin receptor type 2A expression. When comparing the complete somatostatin receptor type 2A immunohistochemical data with somatostatin receptor scintigraphy, an overall high agreement (77%, χ2 test P<0.0001) was observed, irrespective of the degree of differentiation. However, when going through the major causes of discrepancy, some considerations might be drawn. First of all, in most instances the source of discrepancy was related to a negative somatostatin receptor type 2A immunohistochemical result in the presence of positive somatostatin receptor scintigraphy. In this respect it is difficult, if not useless, to determine which method is more sensitive or specific. It is well known, in fact, that false somatostatin receptor scintigraphy positivity may be related to necrotic areas or inflammation which may be frequent within an otherwise somatostatin receptor negative tumor,18 and therefore immunohistochemistry represents, rather than an alternative, a useful adjunct to somatostatin receptor scintigraphy. Moreover, the possible role of other somatostatin receptor subtypes (namely types 3 and 5), which possess high affinity for the currently available somatostatin analogues, was investigated, although their analysis did not improve the overall concordance between scintigraphy and immunohistochemistry, and their application in the clinical practice still needs the availability of satisfactory commercial reagents, in our opinion.
By contrast, it should be speculated that immunohistochemistry may present a lower sensitivity than 111In-pentetreotide scintigraphy and the tissue material investigated may not represent the somatostatin receptor type 2A expression pattern of the whole tumor. The frequent heterogeneity of somatostatin receptor distribution in tumor tissues may cause discrepant (either positive or negative) immunohistochemical results as compared to somatostatin receptor scintigraphy, and this is more evident in our study when analyzing separately preoperative (ie small tissue fragments) and metastatic samples, which showed lower concordance rates (73 and 65%, χ2 P=0.09 and P=0.3, respectively). Technical artifacts related to tissue fixation and preservation are instead unlikely to explain discrepancies between the two methods considered, since comparable results were observed in both formalin and alcohol-fixed tissue specimens, and irrespective of the length of tissue storage.
It is important to note that the correlation with somatostatin receptor scintigraphy represents only one side of the matter, and the predictive value of somatostatin receptor immunohistochemistry in determining the clinical response to somatostatin analogues treatment would have comparable if not greater clinical impact. Such a correlation was limited in our study because of heterogeneous medical treatments of the patients and different intrinsic biological behavior of the diseases (ie from well- to poorly differentiated forms). However, in a group of 28 cases with comparable disease and therapeutic schedules, positive somatostatin receptor type 2A immunohistochemistry correlated with somatostatin analogues response in up to 75% of cases. Large clinical trials should be designed to validate the role of somatostatin receptor immunohistochemical profile in the prediction of clinical response.
In conclusion, our data indicate that (i) immunohistochemistry represents a reliable and useful method to characterize somatostatin receptor expression in neuroendocrine tumors, with special reference to type 2A, provided that accurate methodological conditions and standardized interpretation of the immunohistochemical results (membranous vs cytoplasmic pattern) are obtained; (ii) a standardized scoring system for immunohistochemistry is proposed, with good clinical correlates; which support its role as a useful adjunct to somatostatin receptor scintigraphy in the clinical management of these patients, providing additional information on the tissue distribution of the receptors, heterogeneity among primary and metastatic lesions, and picking up false-positive scintigraphic images; (iii) somatostatin receptor type 2A immunohistochemistry may predict clinical response to somatostatin analogue therapy, although further validation on large series is needed.
References
DeLellis RA, LLoyd R, Heitz PU (eds). World Health Organization Classification of Tumors, Pathology and Genetics—Tumors of Endocrine Organs. IARC Press: Lyon, 2004.
Solcia E, Kloppel G, Sobin LH . World Health Organization International histological classification of tumors. Histological typing of endocrine tumors. Springer: Berlin, 2000.
Oberg K, Astrup L, Eriksson B, et al. Guidelines for the management of gastroenteropancreatic neuroendocrine tumors (including bronchopulmonary and thymic neoplasms). Part II-specific NE tumour types. Acta Oncol 2004;43:626–636.
Oberg K, Astrup L, Eriksson B, et al. Guidelines for the management of gastroenteropancreatic neuroendocrine tumours (including bronchopulmonary and thymic neoplasms). Part I-general overview. Acta Oncol 2004;43:617–625.
Waldherr C, Pless M, Maecke HR, et al. Tumor response and clinical benefit in neuroendocrine tumors after 7.4 GBq (90)Y-DOTATOC. J Nucl Med 2002;43:610–616.
Bloom SR, Mortimer CH, Thorner MO, et al. Inhibition of gastrin and gastric-acid secretion by growth-hormone release-inhibiting hormone. Lancet 1974;2:1106–1109.
Epelbaum J . Somatostatin in the central nervous system: physiology and pathological modifications. Prog Neurobiol 1986;27:63–100.
Haroutunian V, Mantin R, Campbell GA, et al. Cysteamine-induced depletion of central somatostatin-like immunoactivity: effects on behavior, learning, memory and brain neurochemistry. Brain Res 1987;403:234–242.
Raynor K, Lucki I, Reisine T . Somatostatin receptors in the nucleus accumbens selectively mediate the stimulatory effect of somatostatin on locomotor activity in rats. J Pharmacol Exp Ther 1993;265:67–73.
Lamberts SW, Krenning EP, Reubi JC . The role of somatostatin and its analogs in the diagnosis and treatment of tumors. Endocr Rev 1991;12:450–482.
Patel YC, Greenwood MT, Panetta R, et al. The somatostatin receptor family. Life Sci 1995;57:1249–1265.
Reisine T, Bell GI . Molecular biology of somatostatin receptors. Endocr Rev 1995;16:427–442.
Hofland LJ, Liu Q, Van Koetsveld PM, et al. Immunohistochemical detection of somatostatin receptor subtypes sst1 and sst2A in human somatostatin receptor positive tumors. J Clin Endocrinol Metab 1999;84:775–780.
Janson ET, Gobl A, Kalkner KM, et al. A comparison between the efficacy of somatostatin receptor scintigraphy and that of in situ hybridization for somatostatin receptor subtype 2 messenger RNA to predict therapeutic outcome in carcinoid patients. Cancer Res 1996;56:2561–2565.
Korner M, Eltschinger V, Waser B, et al. Value of immunohistochemistry for somatostatin receptor subtype sst2A in cancer tissues: lessons from the comparison of anti-sst2A antibodies with somatostatin receptor autoradiography. Am J Surg Pathol 2005;29:1642–1651.
Kulaksiz H, Eissele R, Rossler D, et al. Identification of somatostatin receptor subtypes 1, 2A, 3, and 5 in neuroendocrine tumours with subtype specific antibodies. Gut 2002;50:52–60.
Mundschenk J, Unger N, Schulz S, et al. Somatostatin receptor subtypes in human pheochromocytoma: subcellular expression pattern and functional relevance for octreotide scintigraphy. J Clin Endocrinol Metab 2003;88:5150–5157.
Papotti M, Croce S, Bello M, et al. Expression of somatostatin receptor types 2, 3 and 5 in biopsies and surgical specimens of human lung tumours. Correlation with preoperative octreotide scintigraphy. Virchows Arch 2001;439:787–797.
Papotti M, Bongiovanni M, Volante M, et al. Expression of somatostatin receptor types 1-5 in 81 cases of gastrointestinal and pancreatic endocrine tumors. A correlative immunohistochemical and reverse-transcriptase polymerase chain reaction analysis. Virchows Arch 2002;440:461–475.
Reubi JC, Schaer JC, Waser B, et al. Expression and localization of somatostatin receptor SSTR1, SSTR2, and SSTR3 messenger RNAs in primary human tumors using in situ hybridization. Cancer Res 1994;54:3455–3459.
Reubi JC, Kappeler A, Waser B, et al. Immunohistochemical localization of somatostatin receptors sst2A in human tumors. Am J Pathol 1998;153:233–245.
Vikic-Topic S, Raisch KP, Kvols LK, et al. Expression of somatostatin receptor subtypes in breast carcinoma, carcinoid tumor, and renal cell carcinoma. J Clin Endocrinol Metab 1995;80:2974–2979.
Kwekkeboom DJ, Teunissen JJ, Bakker WH, et al. Radiolabeled somatostatin analog [177Lu-DOTA0,Tyr3]octreotate in patients with neuroendocrine gastroenteropancreatic tumors. J Clin Oncol 2005;23:2754–2762.
Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of Canada. J Natl Cancer Inst 2000;92:205–216.
Volante M, Bozzalla-Cassione F, Papotti M . Somatostatin receptors and their interest in diagnostic pathology. Endocr Pathol 2004;15:275–291.
Reubi JC, Waser B, Liu Q, et al. Subcellular distribution of somatostatin sst2A receptors in human tumors of the nervous and neuroendocrine systems: membranous vs intracellular location. J Clin Endocrinol Metab 2000;85:3882–3891.
Acknowledgements
The present paper has been supported by grants from the Italian Ministry of University (ex 60% to MV and MP). Antibodies against somatostatin receptors have been provided by an unrestricted grant to MV from Novartis Italia.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure/conflict of interest
The authors have no conflict of interest to declare.
Rights and permissions
About this article
Cite this article
Volante, M., Brizzi, M., Faggiano, A. et al. Somatostatin receptor type 2A immunohistochemistry in neuroendocrine tumors: a proposal of scoring system correlated with somatostatin receptor scintigraphy. Mod Pathol 20, 1172–1182 (2007). https://doi.org/10.1038/modpathol.3800954
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3800954
Keywords
This article is cited by
-
Somatostatin receptor 2 (SSTR2) expression is associated with better clinical outcome and prognosis in rectal neuroendocrine tumors
Scientific Reports (2024)
-
Assessing the safety and activity of cabozantinib combined with lanreotide in gastroenteropancreatic and thoracic neuroendocrine tumors: rationale and protocol of the phase II LOLA trial
BMC Cancer (2023)
-
Gastric Amphicrine Carcinoma Showing Neuroendocrine and Pancreatic Acinar Cell Differentiation. Lesson from a Challenging Case Opening New Perspectives in the Diagnostic Work-Up of Gastric Neuroendocrine Neoplasms
Endocrine Pathology (2023)
-
CT-based nomogram development and validation to predict SSTR2, VEGFR2 and MGMT expression for pancreatic neuroendocrine neoplasms
Chinese Journal of Academic Radiology (2023)
-
Sweat-gland carcinoma with neuroendocrine differentiation (SCAND): a clinicopathologic study of 13 cases with genetic analysis
Modern Pathology (2022)