Abstract
INSM1 is a diagnostic marker for neuroendocrine tumors originating in multiple anatomic sites. In the lung, INSM1 shows 76–97% sensitivity for neuroendocrine tumors overall. Our aim was to characterize INSM1 as a diagnostic marker for small cell carcinoma in the context of its epithelial, lymphoid, and mesenchymal morphologic mimics. Immunohistochemistry was performed on 231 tumors, including lung neuroendocrine tumors, nonneuroendocrine carcinomas of the thoracic cavity, diffuse large B-cell lymphomas, and small round cell sarcomas, using an anti-INSM1 mouse monoclonal antibody. Extent (0–100%) and intensity (1–3+) of nuclear INSM1 staining was multiplied in each case to calculate an H-score. Demographic and clinical information was obtained from the medical record. INSM1 had an overall sensitivity and specificity of 81.5% and 82.7% for small cell carcinoma, respectively, using a threshold established with a receiver operating characteristic curve. 40/48 (82.7%) small cell carcinomas were positive for INSM1, including 19/24 (79%) small cell carcinomas that were negative for chromogranin and synaptophysin. 5/5 carcinoids and 21/28 (75%) large cell neuroendocrine carcinomas showed INSM1 expression. Among nonneuroendocrine tumors, 7/38 (18%) lung adenocarcinomas, 2/17 (12%) lung squamous cell carcinomas, 4/10 (40%) thymic carcinomas, 4/12 (33%) adenoid cystic carcinomas, 1/19 (5%) diffuse large B-cell lymphomas, 4/11 (36%) alveolar rhabdomyosarcomas, and 4/23 (17%) Ewing sarcomas were positive for INSM1. No synovial sarcomas or desmoplastic small round cell tumors were positive. Weak, focal INSM1 expression alone is insufficient as a diagnostic marker for small cell carcinoma, but is sensitive and specific, easy to interpret in small biopsies, and makes a valuable addition to a diagnostic panel.
Similar content being viewed by others
Introduction
Neuroendocrine tumors of the lung are classified as carcinoid tumor, large cell neuroendocrine carcinoma, or small cell carcinoma based on histology, mitotic index, and expression of neuroendocrine markers [1]. Traditional immunohistochemical markers of neuroendocrine differentiation include chromogranin, synaptophysin, and CD56, all of which have varying diagnostic sensitivity and specificity for pulmonary neuroendocrine tumors. Small cell carcinoma accounts for ~15% of lung tumors [2, 3], and requires a significantly different clinical and chemotherapeutic management approach compared with other neuroendocrine and nonneuroendocrine tumors of the lung [4]. Although positive in nearly all carcinoid tumors [1], traditional markers of neuroendocrine differentiation can be negative in 15–40% of small cell carcinoma, depending on the marker and specimen size [3, 5, 6], and 15% of small cell carcinomas can be negative for multiple neuroendocrine markers [3]. TTF-1, which is typically positive in pulmonary adenocarcinomas and neuroendocrine tumors, may also be negative in 15–23% of small cell lung carcinomas [1, 7].
INSM1 is a zinc finger transcription factor and marker of neuroendocrine differentiation initially isolated from normal human pancreatic tissue and mouse insulinoma cell lines [8]. Nuclear expression of INSM1 protein has been observed in neuroendocrine tumors from multiple organ systems, including the pancreas, head and neck sites, gynecologic tract, and prostate, with a high degree of diagnostic sensitivity and specificity [9,10,11,12]. Among primary pulmonary tumors, INSM1 also shows promise as a diagnostic marker for neuroendocrine tumors, with a sensitivity of 92–97% and specificity of 96–100% [13,14,15,16,17,18]. This has prompted some groups to propose INSM1 as a stand-alone diagnostic marker for neuroendocrine differentiation [14]; other groups, however, have demonstrated INSM1 expression in some nonneuroendocrine tumors, suggesting a more cautious approach to diagnostic application [18].
INSM1 positivity has been reported in a small number of small cell lung carcinomas negative for other neuroendocrine markers [14], and shows high sensitivity for small cell carcinoma in cytology specimens [16, 17, 19]. Our aim was to evaluate INSM1 as a diagnostic marker for pulmonary small cell carcinoma, including tumors negative for other neuroendocrine markers, in the context of its histologic mimics.
Methods
Patient and sample selection
This study was conducted with approval by the Brigham and Women’s Hospital Institutional Review Board. Small cell carcinomas positive for at least one traditional neuroendocrine marker diagnosed between 2005 and 2015 with available formalin fixed paraffin-embedded material were included. All cases of pulmonary small cell carcinoma that were negative for chromogranin and synaptophysin diagnosed during this time period were also included in the study group to determine the utility of INSM1 in cases negative for other markers of neuroendocrine differentiation. Mimics of small cell carcinoma reviewed at Brigham and Women’s Hospital during the same time period were also obtained from the Department of Pathology archives, to include: typical and atypical carcinoid tumors, large cell neuroendocrine carcinoma, poorly differentiated lung adenocarcinoma, basaloid squamous cell carcinoma, thymic carcinoma, adenoid cystic carcinoma, diffuse large B-cell lymphoma, NUT carcinoma, Ewing sarcoma, alveolar rhabdomyosarcoma, desmoplastic small round cell tumor, and poorly differentiated synovial sarcoma. Lung adenocarcinomas included were restricted to poorly differentiated cases with a solid component comprising greater than or equal to 50% of the tumor to focus on cases that demonstrate morphologic overlap with small cell carcinoma. 14/23 Ewing sarcomas had confirmation of EWSR1 rearrangement via FISH or RT-PCR. 3/11 alveolar rhabdomyosarcomas had evidence of FOXO1 rearrangement by FISH. The remaining cases of Ewing sarcoma and alveolar rhabdomyosarcoma were diagnosed using immunohistochemistry for CD99, FLI1, NKX2-2 or desmin and myogenin, respectively, by experts in soft tissue pathology. Combined primary pulmonary tumors were not included. Cases that had undergone neoadjuvant treatment were excluded to avoid treatment-related changes in morphology and antigenicity. Demographic and clinical information was obtained from the electronic medical record.
Immunohistochemistry
Formalin fixed paraffin-embedded tissue was sectioned at 5 μm, deparaffinized, and subjected to antigen retrieval using pressure cooker pretreatment in citrate buffer (pH 6.1; Target Retrieval Solution, DAKO, Carpinteria, CA). Immunohistochemistry for INSM1 was performed on all study cases using a mouse monoclonal antibody (Santa Cruz Biotechnology, Dallas, TX; clone A-8). Intensity of INSM1 staining was evaluated in each case as absent (0), weak (1+), moderate (2+), or strong (3+), and extent evaluated as a percentage of all tumor cells. Appropriate positive and negative controls were reviewed throughout the study.
All small cell carcinoma cases were stained for chromogranin (Thermo Fisher Scientific, Waltham, MA; clone LK2H10) and synaptophysin (Leica Biosystems, Buffalo Grove, IL; clone 27G12) as part of routine diagnostic workup. To compare INSM1 staining to traditional neuroendocrine markers, all study cases that were positive for INSM1 were also stained for chromogranin and synaptophysin if paraffin-embedded material was available. Cases of small cell carcinoma that demonstrated absent staining for chromogranin, synaptophysin, TTF-1, and INSM1 were stained with CD56 (Cell Marque, Rocklin, CA; clone 123C3.D5), p40 (Biocare Medical, Concord, CA; clone BC28), CD45 (DAKO, Carpinteria CA; clones PD7/26 and 2B11), and NUT (Cell Signaling Technology, Danvers, MA; clone C5B1) to exclude morphologic mimics of small cell carcinoma if not previously performed as part of the diagnostic workup, and RB1 (BD Biosciences, San Jose, CA; clone G3-245) to support a diagnosis of small cell carcinoma, if sufficient paraffin-embedded material was available.
Statistical analysis
Descriptive statistics were performed using Prism software (Graphpad Prism, version 5.02, GraphPad Software, San Diego, CA). Categorical data were analyzed via Chi Square analysis or the Fisher exact test as appropriate. Continuous variables were analyzed between study groups using the Kruskal–Wallis test with Dunn’s post-hoc analysis. Intensity and extent of INSM1 staining were multiplied to calculate an H-score for all cases, which was then used to generate a receiver operating characteristic curve using the R programming language (R Foundation for Statistical Computing, Vienna, Austria) to determine an optimal diagnostic threshold to differentiate small cell carcinoma from morphologic mimics.
Results
Demographic and specimen characteristics are described in Table 1. In total, 231 cases were included in the study, including 24 small cell carcinomas (obtained from 23 patients) that were negative for chromogranin and synaptophysin, 24 small cell carcinomas positive for at least one conventional neuroendocrine marker, and 183 non-small cell mimics of small cell carcinoma. Age was significantly different between these three groups (p = 0.0002), accounted for by older age at presentation of marker-negative small cell carcinomas. Small cell carcinomas were more likely to be sampled by biopsy than resection (p < 0.0001). No differences in sex distribution or site of tumor sampling were present between groups (p > 0.5 for all).
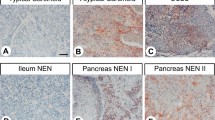
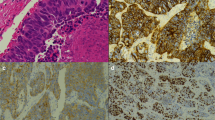
The distribution of H-scores among patients with each tumor type is summarized in Fig. 1a. A receiver operating characteristic curve (Fig. 1b) yielded an optimal diagnostic cutoff H-score of 50 (Fig. 1c, d) to distinguish between small cell carcinoma and morphologic mimics, with a sensitivity of 81.5% and specificity of 82.7%. INSM1 expression in small cell lung carcinoma and morphologic mimics is summarized in Table 2. Overall, 40 of 48 (83%) small cell carcinomas were positive for INSM1 at our established diagnostic threshold, most commonly with a diffuse and strong staining pattern (Fig. 2). Of 24 small cell carcinomas negative for chromogranin and synaptophysin, 13 of which were also negative for TTF-1, 19 (79%) were positive for INSM1 (Fig. 2a, b). Five chromogranin- and synaptophysin-negative small cell carcinomas were also INSM1 negative. Among these, three of four cases subsequently stained for CD56 were positive, one of five cases was TTF-1 positive, four of five showed RB1 loss, and one demonstrated positivity only for keratins, with retained RB1 expression, but presented morphologic, radiologic, and clinical findings consistent with small cell carcinoma and was lost to clinical follow-up. All five carcinoids and 75% of large cell neuroendocrine carcinomas were positive for INSM1. Among other thoracic carcinomas, 18% of adenocarcinomas with 50% or more solid component (Fig. 3a, b), 12% of basaloid squamous cell carcinomas (Fig. 3c, d), 40% of thymic carcinomas (Fig. 3e, f), and 33% of adenoid cystic carcinomas (Fig. 3g, h) were positive for INSM1. One of 19 diffuse large B-cell lymphomas demonstrated strong, diffuse staining (Fig. 4); this tumor expressed LCA, PAX5, CD20, CD30, MUM1, Bcl-2, Bcl-6, and MYC, and was negative for keratins, chromogranin, and synaptophysin. Of the sarcomas, 17% of Ewing sarcomas (Fig. 5) and 36% of alveolar rhabdomyosarcomas (Fig. 6), one of which presented as a mediastinal mass without extrathoracic disease, also demonstrated INSM1 positivity. No cases of NUT carcinoma, synovial sarcoma, or desmoplastic small round cell tumor showed INSM1 staining.
a Distribution of H-score in small cell carcinoma and morphologic mimics. SCLC* small cell lung carcinoma negative for chromogranin and synaptophysin, SCLC small cell carcinoma positive for chromogranin, synaptophysin, or both, LCNEC large cell neuroendocrine carcinoma, Pr. Solid ACA predominantly solid ACA, SqCC squamous cell carcinoma, Thymic Carc thymic carcinoma, EWS Ewing sarcoma, ARMS alveolar rhabdomyosarcoma, DSRCT desmoplastic small round cell tumor, PDSYS poorly differentiated synovial sarcoma, DLBCL diffuse large B-cell lymphoma. b A receiver operating characteristic curve yields a diagnostic H-score cutoff of 50 as optimal for the distinction between small cell carcinoma and morphologic mimics. Examples of study cases with an H-score of 50, taken at ×400 magnification, including (c) a case with 10% 3+ and 10% 2+ staining and (d) a case with diffuse, 1+ staining in ~50% of tumor cells.
Poorly differentiated or basaloid tumors arising in the thoracic cavity may show morphologic similarity to small cell carcinoma and express neuroendocrine markers. a Adenocarcinoma with a solid component (inset: glandular architecture), demonstrating (b) strong INSM1 expression. c Basaloid squamous cell carcinoma with (d) weak to moderate, diffuse INSM1 expression. e Thymic carcinoma, undifferentiated type, with (f) strong INSM1 expression. g Adenoid cystic carcinoma demonstrating (h) weak diffuse INSM1 expression. All images taken at ×400 magnification.
Ewing sarcoma, presenting as an isolated right middle lobe nodule. a Hematoxylin and eosin stain demonstrates a proliferation of small round cells that are positive for b CD99 and negative for c WT-1. D INSM1 demonstrated multifocal, moderate to strong nuclear reactivity. Images taken at ×400 magnification.
a Brain metastasis in a smoker who initially presented with a mediastinal mass and was treated for small cell carcinoma (H&E, ×400). b Desmin (×400) and c MyoD1 (×400) were positive in tumor cells, allowing reclassification as alveolar rhabdomyosarcoma. d INSM1 demonstrated patchy moderate nuclear positivity, with occasional strongly positive cells (×400).
The results of immunohistochemical staining for chromogranin and synaptophysin with respect to INSM1 in neuroendocrine and nonneuroendocrine tumors are summarized in Supplementary Fig. 1. All five carcinoid tumors were positive for all three markers. Twenty-six of 28 large cell neuroendocrine carcinomas, including two that were INSM1 negative, stained for either chromogranin, synaptophysin, or both. Two large cell neuroendocrine carcinomas were negative for chromogranin, synaptophysin, and INSM1, but were focally positive for CD56. Among 23 INSM1-positive nonneuroendocrine tumors, 11 demonstrated at least focal staining with either chromogranin, synaptophysin, or both: 3/4 Ewing sarcomas, 2/4 thymic carcinomas, 4/5 lung adenocarcinomas, and 2/3 alveolar rhabdomyosarcomas.
Discussion
Immunohistochemistry for markers of neuroendocrine differentiation is often incorporated into the diagnostic workup for pulmonary neuroendocrine tumors, and increases diagnostic accuracy and interobserver agreement [20]. Timely and accurate diagnosis is essential for optimal management of patients with small cell lung carcinoma, who primarily present with advanced disease and require a specific chemo- and radiotherapeutic approach [4, 21]. The diagnosis of small cell lung carcinoma is frequently made on small biopsy samples, and presents unique challenges including crush artifact and limited evaluation of morphology and mitotic index. Ancillary diagnostic workup to support neuroendocrine differentiation and exclude other tumors is therefore crucial. Chromogranin A, synaptophysin, and CD56 (NCAM) are currently recommended as first-line neuroendocrine markers based on favorable performance characteristics [1]. The sensitivity of each marker for pulmonary neuroendocrine tumors ranges from 58 to 98%, depending on tumor type and specimen size [22,23,24]; however, chromogranin A, synaptophysin, and CD56, can be seen in up to 5.5%, 17%, and 28% of non-small cell lung carcinomas, respectively [25, 26], including poorly differentiated tumors that can resemble small cell carcinoma. Neuroendocrine markers may also be positive in other potential morphologic mimics of small cell carcinoma including thymic carcinoma [27], alveolar rhabdomyosarcoma [28, 29], Ewing sarcoma [30], synovial sarcoma [28], desmoplastic small round cell tumor [31], and rarely in diffuse large B-cell lymphoma (CD56) [32].
Several studies have demonstrated INSM1 to be a promising marker of neuroendocrine differentiation [14,15,16,17, 33, 34]. INSM1 is a transcriptional repressor with zinc finger DNA-binding motifs that is transiently expressed in the endocrine tissues and nervous system during embryonal organogenesis and reduced or absent in normal adult tissues [35, 36]. In neuroendocrine tumors, INSM1 protein expression is upregulated by sonic hedgehog signaling (shh) via the MEK/ERK pathway and activation of MYCN, which is frequently also amplified in high grade neuroendocrine tumors [37]. INSM1 in turn stabilizes MYCN, resulting in continuous shh-MEK/ERK-MYC signaling and cell proliferation [37]. INSM1 also appears to directly regulate expression of the traditional neuroendocrine markers chromogranin, synaptophysin, and CD56, and may play a direct role in neuroendocrine differentiation [13].
Sensitivity of INSM1 for all four types of pulmonary neuroendocrine tumors ranges from 76 to 97%, and specificity from 97 to 100% [14,15,16,17, 34, 38]. Nearly all small cell carcinomas demonstrate INSM1 positivity [14, 17]; in a study of 267 thoracic tumors, Rooper et al. furthermore demonstrated that eight small cell carcinomas negative for all three traditional markers were INSM1 positive [14]. To date, however, no studies have specifically evaluated expression in morphologic mimics of small cell lung cancer. Our study supports a diagnostic H-score threshold of 50 for the diagnosis of small cell lung carcinoma and demonstrates good sensitivity (81.5%) and specificity (82.7%) within this context. Although we found a lower sensitivity for small cell carcinoma than seen in most studies [14,15,16,17, 19], this is likely due to the fact that approximately half of the included small cell carcinomas were negative for chromogranin and synaptophysin, half of which in turn were also negative for TTF-1. Small cell carcinomas negative for TTF-1 are less likely to stain for traditional neuroendocrine markers [7], and may inherently have a reduced neuroendocrine phenotype. Indeed, five of the six INSM1-negative small cell carcinomas were negative for chromogranin and synaptophysin, and three of those were also TTF-1 negative. Our findings therefore likely underestimate the sensitivity of INSM1 in small cell carcinoma in general; however, we included an expanded subset of marker-negative small cell carcinomas, as they may present a particular diagnostic challenge, especially in small biopsies with altered or obscured morphology. The majority of the 24 small cell carcinomas in our study that were negative for chromogranin and synaptophysin were nevertheless positive for INSM1. Five small cell carcinomas negative for chromogranin and synaptophysin, however, were also negative for INSM1. Four of these cases were stained for CD56, and three showed membranous positivity.
Among morphologic mimics of small cell carcinoma, a subset of poorly differentiated lung adenocarcinomas, basaloid squamous cell carcinomas, thymic carcinomas, adenoid cystic carcinomas, alveolar rhabdomyosarcomas, and Ewing sarcomas demonstrated significant INSM1 positivity. Most of the INSM1-positive Ewing sarcomas, thymic carcinomas, and alveolar rhabdomyosarcomas that were also stained for chromogranin and synaptophysin were positive for at least one traditional neuroendocrine marker. The proportion of INSM1-positive adenocarcinomas and squamous cell carcinomas is higher than noted in previous studies [14,15,16, 18]. Four of five INSM1-positive adenocarcinomas that were also stained for traditional neuroendocrine markers also showed either chromogranin or synaptophysin positivity, or positivity for both. These findings are likely due to our inclusion only of poorly differentiated adenocarcinomas and basaloid squamous cell carcinomas, as studies of poorly differentiated lung tumors have shown a higher rate of positivity for neuroendocrine markers [39]. While INSM1 positivity in the non-small cell tumors included in our study may therefore indicate some amount of true, morphologically inapparent neuroendocrine differentiation, our findings nonetheless emphasize the importance of caution in interpreting INSM1 in poorly differentiated tumors that may mimic small cell carcinoma.
Finally, our results also suggest that rare diffuse large B-cell lymphomas may demonstrate aberrant INSM1 expression. The underlying pathogenesis of aberrant INSM1 expression has not been well characterized and likely arises in heterogeneous ways; one case report of chronic lymphocytic leukemia demonstrated the possibility of a chromosomal translocation bringing ASCL1, a master regulator of neurogenesis, into the proximity of an enhancer, thereby leading to upregulation of its target INSM1 [40].
Although CD56 has not routinely been performed at our institution for evaluation of neuroendocrine tumors, and sufficient material was not available to perform the stain on all study cases, the fact that three of four INSM1-negative small cell carcinomas in our study group were CD56 positive supports the use of multiple neuroendocrine markers as part of a complete diagnostic panel. Similarly, although calculating an H-score has limited value in day-to-day practice, small amounts of INSM1 reactivity were seen in multiple tumor types in our study, and INSM1 positivity greater than our minimum diagnostic threshold was seen in common and rare thoracic tumors that show morphologic overlap with small cell carcinoma. Focal and weak INSM1 positivity alone is therefore insufficient for definitive diagnosis of small cell carcinoma. Our study shows, however, that it is still a sensitive and specific marker even in the context of a challenging differential diagnosis, and as nuclear stain, it is especially suited to interpretation in small biopsies. INSM1 is thus a valuable addition to a diagnostic panel for small cell lung carcinoma, when necessary, as long as it is interpreted cautiously within the context of morphologic, radiologic, and clinical findings.
References
WHO. Classification of tumours of the lung, pleura, thymus, and heart. 4th ed. Travis WBE, Burke A, Marx A, Nicholson AE, editors. Lyon: IARC; 2015.
Filosso PL, Falcoz PE, Solidoro P, Pellicano D, Passani S, Guerrera F, et al. The European Society of Thoracic Surgeons (ESTS) lung neuroendocrine tumors (NETs) database. J Thorac Dis. 2018;10:S3528–32.
Nicholson SA, Beasley MB, Brambilla E, Hasleton PS, Colby TV, Sheppard MN, et al. Small cell lung carcinoma (SCLC): a clinicopathologic study of 100 cases with surgical specimens. Am J Surg Pathol. 2002;26:1184–97.
Jett JR, Schild SE, Kesler KA, Kalemkerian GP. Treatment of small cell lung cancer: diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143:e400S–19S.
Guinee DG Jr., Fishback NF, Koss MN, Abbondanzo SL, Travis WD. The spectrum of immunohistochemical staining of small-cell lung carcinoma in specimens from transbronchial and open-lung biopsies. Am J Clin Pathol. 1994;102:406–14.
Brambilla E, Veale D, Moro D, Morel F, Dubois F, Brambilla C. Neuroendocrine phenotype in lung cancers. Comparison of immunohistochemistry with biochemical determination of enolase isoenzymes. Am J Clin Pathol. 1992;98:88–97.
Iida Y, Masuda S, Nakanishi Y, Shimizu T, Nishimaki H, Takahashi M, et al. Clinicopathological characteristics of thyroid transcription factor 1-negative small cell lung cancers. Hum Pathol. 2018;79:127–34.
Goto Y, De Silva MG, Toscani A, Prabhakar BS, Notkins AL, Lan MS. A novel human insulinoma-associated cDNA, IA-1, encodes a protein with “zinc-finger” DNA-binding motifs. J Biol Chem. 1992;267:15252–7.
Kuji S, Watanabe R, Sato Y, Iwata T, Hirashima Y, Takekuma M, et al. A new marker, insulinoma-associated protein 1 (INSM1), for high-grade neuroendocrine carcinoma of the uterine cervix: analysis of 37 cases. Gynecol Oncol. 2017;144:384–90.
Tanigawa M, Nakayama M, Taira T, Hattori S, Mihara Y, Kondo R, et al. Insulinoma-associated protein 1 (INSM1) is a useful marker for pancreatic neuroendocrine tumor. Med Mol Morphol. 2018;51:32–40.
Xin Z, Zhang Y, Jiang Z, Zhao L, Fan L, Wang Y, et al. Insulinoma-associated protein 1 is a novel sensitive and specific marker for small cell carcinoma of the prostate. Hum Pathol. 2018;79:151–9.
Rooper LM, Bishop JA, Westra WH. INSM1 is a sensitive and specific marker of neuroendocrine differentiation in head and neck tumors. Am J Surg Pathol. 2018;42:665–71.
Fujino K, Motooka Y, Hassan WA, Ali Abdalla MO, Sato Y, Kudoh S, et al. Insulinoma-associated protein 1 is a crucial regulator of neuroendocrine differentiation in lung cancer. Am J Pathol. 2015;185:3164–77.
Rooper LM, Sharma R, Li QK, Illei PB, Westra WH. INSM1 demonstrates superior performance to the individual and combined use of synaptophysin, chromogranin and CD56 for diagnosing neuroendocrine tumors of the thoracic cavity. Am J Surg Pathol. 2017;41:1561–9.
Mukhopadhyay S, Dermawan JK, Lanigan CP, Farver CF. Insulinoma-associated protein 1 (INSM1) is a sensitive and highly specific marker of neuroendocrine differentiation in primary lung neoplasms: an immunohistochemical study of 345 cases, including 292 whole-tissue sections. Mod Pathol. 2019;32:100–9.
Doxtader EE, Mukhopadhyay S. Insulinoma-associated protein 1 is a sensitive and specific marker of neuroendocrine lung neoplasms in cytology specimens. Cancer Cytopathol. 2018;126:243–52.
Rodriguez EF, Chowsilpa S, Maleki Z. Insulinoma-associated protein 1 immunostain: a diagnostic tool for pulmonary small cell carcinoma in cytology. Acta Cytol. 2018;62:333–8.
Kriegsmann K, Zgorzelski C, Kazdal D, Cremer M, Muley T, Winter H, et al. Insulinoma-associated protein 1 (INSM1) in Thoracic tumors is less sensitive but more specific compared with synaptophysin, chromogranin A, and CD56. Appl Immunohistochem Mol Morphol. 2018. [Online ahead of print].
Nakra T, Nambirajan A, Guleria P, Phulware RH, Jain D. Insulinoma-associated protein 1 is a robust nuclear immunostain for the diagnosis of small cell lung carcinoma in cytology smears. Cancer Cytopathol. 2019;127:539–48.
Thunnissen E, Borczuk AC, Flieder DB, Witte B, Beasley MB, Chung JH, et al. The use of immunohistochemistry improves the diagnosis of small cell lung cancer and its differential diagnosis. An international reproducibility study in a demanding set of cases. J Thorac Oncol. 2017;12:334–46.
Stinchombe T. Current treatments for surgically resectable, limited-stage, and extensive-stage small cell lung cancer. Oncologist. 2017;22:1510–7.
Kaufmann O, Georgi T, Dietel M. Utility of 123C3 monoclonal antibody against CD56 (NCAM) for the diagnosis of small cell carcinomas on paraffin sections. Hum Pathol. 1997;28:1373–8.
Lyda MH, Weiss LM. Immunoreactivity for epithelial and neuroendocrine antibodies are useful in the differential diagnosis of lung carcinomas. Hum Pathol. 2000;31:980–7.
Mlika M, Zendah I, Braham E, El Mezni F. CD56 antibody: old-fashioned or still trendy in endocrine lung tumors. J Immunoass Immunochem. 2015;36:414–9.
Howe MC, Chapman A, Kerr K, Dougal M, Anderson H, Hasleton PS. Neuroendocrine differentiation in non-small cell lung cancer and its relation to prognosis and therapy. Histopathology. 2005;46:195–201.
Ionescu DN, Treaba D, Gilks CB, Leung S, Renouf D, Laskin J, et al. Nonsmall cell lung carcinoma with neuroendocrine differentiation-an entity of no clinical or prognostic significance. Am J Surg Pathol. 2007;31:26–32.
Weissferdt A, Moran CA. Neuroendocrine differentiation in thymic carcinomas: a diagnostic pitfall: an immunohistochemical analysis of 27 cases. Am J Clin Pathol. 2016;145:393–400.
Miettinen M, Cupo W. Neural cell adhesion molecule distribution in soft tissue tumors. Hum Pathol. 1993;24:62–6.
Bahrami A, Gown AM, Baird GS, Hicks MJ, Folpe AL. Aberrant expression of epithelial and neuroendocrine markers in alveolar rhabdomyosarcoma: a potentially serious diagnostic pitfall. Mod Pathol. 2008;21:795–806.
Hafezi S, Seethala RR, Stelow EB, Mills SE, Leong IT, MacDuff E, et al. Ewing’s family of tumors of the sinonasal tract and maxillary bone. Head Neck Pathol. 2011;5:8–16.
Ordonez NG. Desmoplastic small round cell tumor: II: an ultrastructural and immunohistochemical study with emphasis on new immunohistochemical markers. Am J Surg Pathol. 1998;22:1314–27.
Stacchini A, Barreca A, Demurtas A, Aliberti S, di Celle PF, Novero D. Flow cytometric detection and quantification of CD56 (neural cell adhesion molecule, NCAM) expression in diffuse large B cell lymphomas and review of the literature. Histopathology. 2012;60:452–9.
Rosenbaum JN, Guo Z, Baus RM, Werner H, Rehrauer WM, Lloyd RV. INSM1: a novel immunohistochemical and molecular marker for neuroendocrine and neuroepithelial neoplasms. Am J Clin Pathol. 2015;144:579–91.
Rodriguez EF, Fite JJ, Chowsilpa S, Maleki Z. Insulinoma-associated protein 1 immunostaining on cytology specimens: an institutional experience. Hum Pathol. 2019;85:128–35.
Liu WD, Wang HW, Muguira M, Breslin MB, Lan MS. INSM1 functions as a transcriptional repressor of the neuroD/beta2 gene through the recruitment of cyclin D1 and histone deacetylases. Biochem J. 2006;397:169–77.
Lan MS, Breslin MB. Structure, expression, and biological function of INSM1 transcription factor in neuroendocrine differentiation. FASEB J. 2009;23:2024–33.
Chen C, Breslin MB, Lan MS. Sonic hedgehog signaling pathway promotes INSM1 transcription factor in neuroendocrine lung cancer. Cell Signal. 2018;46:83–91.
Viswanathan K, Siddiqui MT, Borczuk AC. Insulinoma-associated protein 1 is a sensitive and specific marker for lung neuroendocrine tumors in cytologic and surgical specimens. J Am Soc Cytopathol. 2019;8:299–308.
Visscher DW, Zarbo RJ, Trojanowski JQ, Sakr W, Crissman JD. Neuroendocrine differentiation in poorly differentiated lung carcinomas: a light microscopic and immunohistologic study. Mod Pathol. 1990;3:508–12.
Malli T, Rammer M, Haslinger S, Burghofer J, Burgstaller S, Boesmueller HC, et al. Overexpression of the proneural transcription factor ASCL1 in chronic lymphocytic leukemia with a t(12;14)(q23.2;q32.3). Mol Cytogenet. 2018;11:3.
Acknowledgements
The authors would like to acknowledge the Brigham and Women’s Hospital Department of Pathology, Histology Laboratory, and Immunohistochemistry Laboratories for providing funding and technical support for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
HKT has no disclosures. JLH is a consultant to Eli Lilly and Epizyme. These relationships are not relevant to the subject of this study. MV performs consulting work for Merck Pharmaceuticals. This relationship is not relevant to the subject of this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Tsai, H.K., Hornick, J.L. & Vivero, M. INSM1 expression in a subset of thoracic malignancies and small round cell tumors: rare potential pitfalls for small cell carcinoma. Mod Pathol 33, 1571–1580 (2020). https://doi.org/10.1038/s41379-020-0517-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-020-0517-0
This article is cited by
-
Neuroendocrine and squamous cell phenotypes of NUT carcinoma are potential diagnostic pitfalls that discriminating it from mimickers, such as small cell and squamous cell carcinoma
Diagnostic Pathology (2024)
-
Lung neuroendocrine neoplasms: recent progress and persistent challenges
Modern Pathology (2022)
-
Insulinoma-associated-1 (INSM1) expression in thymic squamous cell carcinoma
Virchows Archiv (2022)
-
Overview of the 2022 WHO Classification of Neuroendocrine Neoplasms
Endocrine Pathology (2022)