Abstract
Study design:
Retrospective case study.
Objectives:
Report a rare case of cervical myelopathy induced by calcium pyrophosphate dehydrate (CPPD) deposition in multiple cervical levels.
Setting:
An area teaching hospital in Taiwan.
Method:
A patient with cervical myelopathy was evaluated by computerized tomography (CT) scan and magnetic resonance (MR) image. CPPD deposition known as pseudogout was diagnosed and approved by a polarized microscope.
Result:
A prominent hypertrophy of ligmentum flavum and a retro-odontoid bulging mass induced cord compression were found in CT scan and MR image. CPPD deposition was confirmed by the histological examinations in the ligamentum flavum at the spinal levels of C3–C6. After decompression surgery of spine and comprehensive rehabilitation, the patient's neurological symptoms subsided and her neurological functions improved leading to a good prognosis.
Conclusion:
CPPD deposition in cervical spine occurring at multiple levels is rare. Image studies with CT scan and MR are complementary in the diagnosis of CPPD-induced myelopathy. Surgical decompression is always required and expected to have a good outcome.
Similar content being viewed by others
Introduction
Calcium pyrophosphate dehydrate (CPPD) deposition disease, also known as pseudogout, was first recognized as a distinct disease by McCarty and Hollander in 1962.1 They used a compensated polarized microscope to investigate CPPD crystal and found the character of weakly positive birefringence. It was called pseudogout because it might be clinically indistinguishable from gout.
CPPD deposition disease occurred commonly at the knee, elbow, wrist, hip and shoulder joints. However, it was rarely known to affect the spine and became symptomatic. In the previous report of patients with pseudogout in the spine,2, 3, 4, 5 most of them had a retro-odontoid mass with a spinal cord compression. In a recent report of Yoshida et al,6 they found two patients with pseudogout having severe neck pain and CPPD deposition in the ligamentum flava among the levels of C3–C6 and at the transverse ligament of the atlas. Previous report of pseudogout involving cervical spine were always found at one segment. Here, we present the first case of pseudogout-induced cervical myelopathy with CPPD deposition in multiple levels of ligamentum flavum of and a retro-odontoid mass.
Case report
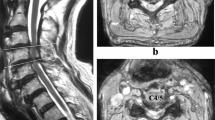
A 74-year-old woman had progressive weakness more pronounced in the upper extremities in recent years without any history of trauma. Paresthesia over both hands and painful knee swelling accompanied with gait difficulties were noted during the disease course. Physical examination showed no fever. There was a prominent limitation of motion range in cervical spine. Muscle power in bilateral upper extremity muscles was 2/5 in Medical Research Council (MRC) scale and 3/5 in lower extremities. Muscle atrophy was noted over the distal lower extremities. Sensory impairment in light touch and pinprick was found below C5 dermatome level. Her muscle tone was increased and deep tendon reflexes were hyperactive in upper and lower extremities. However, her jaw jerk was negative. Laboratory tests showed her serum C-reactive protein (CRP) concentration was 0.31 mg/dl. Uric acid level was 6.3 mg/dl. White blood cell count was 7500/cmm. Erythrocyte sedimentation rate (ESR) was 66 mm at first hour and 99 mm at second hour. X-ray examination of cervical spine showed a spondylotic change with spur formation and a mild subluxation at C5 on C6 level. MR imaging study of the cervical spine revealed a marked spinal stenosis at C3–C4, C4–C5 and C5–C6 levels with the findings of bulging herniated discs and hypertrophic ligmentum flavum (Figure 1). Sausage appearance of the thecal sac between the levels of C3 and C4 and between the levels of C5 and C6 was found. In the same time, there was a bulging mass lesion with hypointensity on T1-weighted image and an isointensity with areas of hyperintensity signal posterior to the odontoid process on T2-weighted image (Figure 2). The retro-odontoid mass with a compression of the cervical cord and narrowing of the spinal canal was found. Otherwise, a mild erosion of the odontoid process was noted in the imaging studies (Figure 3).
Decompression surgery was performed with a laminectomy at C3–C6 levels and removal of the ligamentum flavum extended to the posterior arch of the atlas. Histopathologic examination of the specimen revealed a prominent hyaline degeneration and calcification in the fragment of ligamentum flava and the cartilaginous tissue. CPPD deposition with rod-shaped crystals were demonstrated under the polarized microscope (Figure 4) and the crystal was shown in hematoxylin and eosin stain.
The patient's neurological symptoms were improved gradually after surgery. Paresthesia and pain over the extremities subsided later. Her muscle strength improved to 4/5 MRC scale in all extremities and her functional activities of daily living improved to totally independent after rehabilitation.
Discussion
A mild erosion of odontoid in CT scan and a subluxation of cervical spine between C5 and C6 levels were found in the present case. These findings are the distinct features of CPPD deposition disease. CPPD was known to occur frequently in the various soft tissues including cartilage, joint capsule, synovium, bursae, tendons, and ligaments. However, it is important to aware that the deposits of CPPD can occur within the facet joints, ligamentum flavum, or other tissues in proximity to the spinal canal. This manifestation may cause spinal cord or nerve root compression and also may progressively result in vertebral destruction, spondylolisthesis, and odontoid erosion as shown in our patient. The destructive process of the disease may further progress and lead to a severe result of atlanto-axial subluxation or a pathologic fracture of odontoid.
In our patient with cervical myelopathy, differentiation of the risk from the CPPD deposition or from the pre-existing degenerated bulging disc should be performed. In CT scan and MR image, there were prominent central herniated disc at the cervical spinal levels of C3–C4, C4–C5 and C5–C6. However, the thecal sacs at these levels were patent. From the MR image with a different density, a prominent hypertrophic ligamentum flavum at C3–C4 level and widely extended to the C5 and C6 levels was found. These hypertrophic tissues noted as CPPD deposition were close to the cord. Otherwise, the MR image at C1 level showed a displacement and compression sign of the cord by the retro-odontoid mass. These evidences suggested that the cervical cord compression in this patient was mainly due to the CPPD deposition mass. Clinically, it was possible that the degenerative disc herniation was a precipitating factor and the clinical syndrome of myelopathy was related to its association with chronic CPPD deposition.
From the study report of Sushil and Anant,7 they stated that CT scan and MR image were the optimal diagnostic methods of CPPD deposition disease. They found that the CPPD deposition was scattering in small masses and a cause of large, symptomatic mass lesion in the peri-odontoid area was rare. Their study demonstrated four important diagnostic features of CPPD deposition disease in seven patients including: (1) a mostly isointense mass on the T1-weighted MR image, (2) areas of calcification within the mass on the CT scan, (3) a mixed density mass with the signal ranging from hypo- to hyperintense in T2-weighted MR image, and (4) a peripheral enhancement of the mass on the postcontrast MR image. On the base of these findings, the retro-odontoid CPPD deposition lesions could be diagnosed with a high degree of certainty preoperatively. Recently, Kakitsubata et al8 report nine patients with CPPD deposition in and around the atlanto-axial joint associated with a type II odontoid fracture. Their findings were strongly dependent on the MR image. Otherwise, the MR image and CT scan were important for differentiation of the acute and chronic CPPD disease. The imaging findings of perifocal edema or mass effect around the CPPD deposition may represent an acute inflammation; whereas the areas of calcification in the mass and erosion or destruction of the surrounding bony tissue may suggest a chronic CPPD disease.
Conclusion
CPPD deposition may occur at multiple spinal levels and present as a progressive myelopathy. Image studies with CT scan and MR are complementary and polarized-light microscopy examination may assist in the diagnosis of this disease. Decompression surgery is always required and good prognosis is expected.
References
McCarty Jr DJ, Kogn NN, Faires JS . The significance of calcium phosphate crystals in the synovial fluid of arthritic patients: ‘The pseudogout syndrome’ I. Clinical aspects. Ann Intern Med 1962; 56: 711–737.
Zunkeler B, Schelper R, Menezes AH . Periodontoid calcium pyrophosphate dihydrate deposition disease: ‘pseudogout’ mass lesion of the craniocervical junction. J Neurosurg 1996; 85: 803–809.
Ciricillo SF, Weinstein PR . Foramen magnum syndrome from pseudogout of the atlanto-occipital ligament: case report. J Neurosurg 1989; 71: 141–143.
Ishida T, Dorfmann HD, Bullough PG . Tophaceous pseudogout (tumoral calcium pyrophosphate dihydrate crystal deposition disease). Hum Pathol 1995; 26: 587–593.
Wells CR, Morgello S, Dicarlo E . Cervical myelopathy due to calcium pyrophosphate dihydrate deposition disease. J Neurol Neurosurg Psychiatry 1991; 54: 658–659.
Yoshida T, Sekijima Y, Hoshi K, Kaneko K, Hashimoto T . Two patients with pseudogout manifested by severe neck pain. Rinsho Shinkeigaku 2002; 42: 308–312.
Sushil P, Anant K . Ossified-calcified ligamentum flavum causing dorsal cord compression with computed tomography-magnetic resonance imaging features. Surg Neurol 1994; 41: 441–442.
Kakitsubata Y, Boutin RD, Theodorou DJ . Calcium pyrophosphate dihydrate crystal deposition in and around the atlantoaxial joint: association with type II odontoid fractures in nine patients. Radiology 2000; 216: 213–219.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Lin, SH., Hsieh, ET., Wu, TY. et al. Cervical myelopathy induced by pseudogout in ligamentum flavum and retro-odontoid mass: a case report. Spinal Cord 44, 692–694 (2006). https://doi.org/10.1038/sj.sc.3101890
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101890
Keywords
This article is cited by
-
Multilevel calcium pyrophosphate dihydrate deposition in cervical ligamentum flavum: clinical characteristics and imaging features
BMC Musculoskeletal Disorders (2021)
-
Cervical myelopathy due to subaxial calcium pyrophosphate dihydrate (CPPD) deposition with simultaneous asymptomatic crowned dens syndrome: two case reports
BMC Musculoskeletal Disorders (2020)
-
Recovery After Cervical Decompression Surgery for the Treatment of Crowned Dens Syndrome Causing Progressive Neurological Decline: A Case Report
HSS Journal ® (2014)
-
Headaches Related to Rheumatologic Disease
Current Pain and Headache Reports (2013)