Abstract
Introduction
Dialysis-related amyloidosis (DRA) can lead to various degenerative conditions but rarely involves the spine with a spinal cord compression.
Case report
The authors describe a progressive tetraparesis (AIS-B) in a 57-year-old woman with upper cervical dialysis-related amyloidoma. Magnetic resonance imaging (MRI) showed a solid focal mass lesion at the C2-odotoid level with severe spinal cord compression. Computed tomography (CT) outlined multiple lytic lesions in C1 lateral masses and odontoid process. The patient underwent urgent surgical treatment. A posterior C1-C2 spinal cord decompression with biopsy followed by occipito-cervical posterior fixation was performed. Histopathological examination revealed amyloid deposits representing DRA. An immediately postoperative neurological improvement was observed.
Discussion
Even if the spinal amyloidoma is extremely rare, this condition has to be suspected in a long-term hemodialysis patient suffering from progressive neurological deficits. Differential diagnosis is mandatory between infections, rheumatologic and neoplastic lesions. Imaging evaluation with CT and MRI is recommended in order to assess the characteristics of the pathological mass, the extension of lytic lesions and the entity of neurological compression. Surgical treatment is mandatory if clinical evidence of root or spinal cord compression is present.
Similar content being viewed by others
Introduction
Dialysis-related amyloidosis (DRA) is a common osteoarticular complication in patients with a long-term history of hemodialysis. It is secondary to beta 2 microglobulin (β2M) deposits and is responsible for significant morbidity and potential mortality. DRA usually manifests in osteoarticular structures. When the spine is involved there is evidence of a destructive spondyloarthropathy (DSA). Localized amyloid tumor, also known as amyloidoma, is a nodular mass of amyloid deposits and is a rare manifestation of DRA. Cervical spine is an unusual localization and only few cases have been described in literature [1,2,3]. We report a case of C1-C2 dialysis-related amyloidoma associated with lytic lesions presenting progressive tetraparesis by severe spinal cord compression which required urgent spinal surgery.
Case presentation
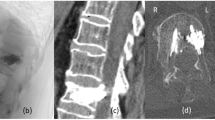
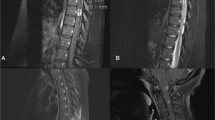
A 57-year-old woman was admitted to our hospital after a progressive worsening of upper and lower limb strength and sensitivity associated to persistent occipital headache. She was affected by end-stage renal disease with a 37-year history of hemodialysis, due to renal transplant failure in glomerulonephritis. She was previously treated for bilateral hip osteonecrosis and underwent a total hip arthroplasty (THA) on the left and a Girdlestone arthroplasty on the right. The main symptom was the acute progressive tetraparesis (AIS-B): right and left sensory level C3, right motor level C6, left motot level C5 [4]. On the cervical CT scan lytic lesions in C1 lateral masses bilaterally, in the odontoid process and in C5-C7-D1 articular masses bilaterally were observed (Fig. 1). The MRI showed a solid mass surrounding odontoid process hypointense in T1, T2 and STIR sequences with a severe spinal cord compression (Fig. 2). On clinical evaluation, considering the NLI (neurological level of injury), the respiratory functions were still fully performing due to very slow onset of the compression, only secondary erythrocytosis was found. Based on imaging, the differential diagnosis included neoplastic pathology, rheumatologic and inflammatory process. Our first diagnostic hypothesis was a synovial pannus but it was rejected by rheumatologic evaluation.
A palliative urgent surgical treatment was performed in order to decompress the spinal cord and give mechanical stability to the occipital-cervical junction. Moreover, intraoperative biopsy from the posterior osteolytic lesions in C1-C2 was obtained for histopathological assessment.
Through a posterior approach a decompressive C1 laminectomy (Fig. 3) following by occipito-cervical fixation with occipital plate, lateral masses screws in C3 and C4 and sublaminar bands in C5 was performed (Fig. 4).
Histopathological examination revealed amyloid deposits, according to the diagnosis of DSA. Specimens were stained in Congo red revealing positive reaction. They mainly showed amorphous substance with few histiocytes and multinuclear giant cells and were positive for β2M immunostaining (Fig. 5).
The neurological deficits immediately improved after surgical treatment and at one-year follow-up clinical recovery was achieved without progression of sign of myelopathy in MRI images.
Discussion
DRA is a clinical syndrome due to the deposition of amyloid made of β2M in the musculoskeletal system (bone and periarticular structures) characterized by pain and disability. This condition is a typical of long-term complication in hemodialysis patients [5]. The necessary conditions for the development of DRA are elevated plasma β2M levels and specific abnormalities encountered in renal insufficiency and/or the process of hemodialysis, but the mechanism of development is still unclear [5].
In other types of amyloidosis, deposition of amyloid is mainly localized in parenchymatous organs. In contrast, accumulation of β2M amyloid in DRA, primarily takes place in osteoarticular tissue. The clinical manifestations include erosive and destructive osteoarthropathy, spondyloarthropathy, cystic bone lesions, fractures and neuropathies leading to joint pain, decreased function, neurological symptoms [5, 6].
In our patient, no sign of systemic amyloidosis was detectable in appendicular skeleton nor internal organs. All the lesions were located in cervical spine, with the typical features of dialysis-related spondyloarthropathy.
DSA has been divided into three types: destructive spondyloarthropathy, amyloid deposition in spinal ligaments and pseudotumor or amyloidoma. Spinal localized amyloidoma is extremely unusual and its extension in epidural space is even more rare [1, 3]. Amyloid deposits are possible in the cervical spine and at the craniocervical junction and its course is unpredictable but generally progressive.
The associated lytic lesions with vertebral body and posterior elements erosion may induce dangerous spinal instability. So, the cervical pain with neurological symptoms in a hemodialysis patient could be the last manifestation in a progressive destroying pathology that could need a prompt surgical treatment [6].
Kuntz first proposed the concept of DSA and described its main diagnostic features:
-
only one spinal segment involved
-
no osteophytosis
-
relatively progressive course
These criteria are useful to differentiate DSA from age spondylotic changes [2].
MRI should be considered the gold standard when DSA is suspected [2]. On MRI, deposits show hypointense or isointense when compared to the spinal cord in T1-weighted sequences and hypointense in T2-weighted sequences [6].
The treatment of beta 2 amyloidosis is challenging. A curative treatment is the restitution of renal function by renal transplantation that would arrest the DRA progression without revert established amyloid deposits. These deposits could sometimes require a surgical solution [3, 5].
Symptomatic medical therapy is recommended. The neurological impairment caused by a mass effect of the amyloidoma is the main indication for a early roots and spinal cord decompression surgical treatment. The spinal stabilization is mandatory when the extension of lytic lesions produce a high pathological instability [1, 3, 6].
DSA is extremely rare. However, it should be considered in the differential diagnosis of spinal mass lesion, particularly in long-term hemodialysis patients.
Our case report highlights how a cervical amyloidoma dialysis-related can cause a severe spinal cord compression requiring urgent surgery for palliative decompression and occipito-cervical fixation.
References
Hsu CW, Wu MS, Leu ML. Dialysis-related cervical amyloidoma presenting with quadriplegia. Ren Fail. 2001;23:135–8.
Nokura K, Koga H, Yamamoto H, Kimura A, Tamai H, Yazaki S, et al. Dialysis-related spinal canal stenosis: a clinicopathological study on amyloid deposition and its AGE modification. J Neurol Sci. 2000;178:114–23.
Takeshima Y, Kotsugi M, Park YS, Nakase H. Hemodialysis-related upper cervical extradural amyloidoma presenting with intractable radiculopathy. Eur Spine J 2012;21:3–6.
Kirshblum SC, Waring W, Biering-Sorensen F, Burns SP, Johansen M, Schmidt-Read M, et al. Reference for the 2011 revision of the International Standards for Neurological Classification of Spinal Cord Injury. J Spinal Cord Med. 2011;34:547–54.
Corlin DB, Heegaard NHH. β2-microglobulin amyloidosis. In: Harris J.R., editor. Protein aggregation and fibrillogenesis in cerebral and systemic amyloid disease, subcellular biochemistry. Dordrecht: Springer Science+Business Media; 2012. pp. 517–40.
Vignes JR, Eimer S, Dupuy R, Donois E, Liguoro D. β2-Microglobulin amyloidosis caused spinal cord compression in a long-term haemodialysis patient. Spinal Cord. 2007;45:322–6.
Acknowledgements
Photomicrograph of a surgical specimen was kindly provided by our Pathological Anatomy Department.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Giorgi, P.D., Pallotta, M.L., Legrenzi, S. et al. Spinal cord compression in dialysis-related upper cervical amyloidoma – a case report. Spinal Cord Ser Cases 7, 40 (2021). https://doi.org/10.1038/s41394-021-00409-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00409-2
This article is cited by
-
Cervical amyloidoma of transthyretin type: a case report and review of literature
BMC Geriatrics (2022)