Abstract
Study Design:
A case report.
Objectives:
To report two cases of intraradicular disc herniation.
Setting:
Kocatepe University Faculty of Medicine, Department of Neurosurgery, Afyon, Turkey, Vakif Gureba Training Hospital, Department of Neurosurgery, Istanbul, Turkey and Yeditepe University Faculty of Medicine, Department of Neurosurgery, Istanbul, Turkey.
Methods:
Two cases with intraradicular disc herniation at L2–3 level in one, and at L5–S1 level in the other were presented. Both patients were admitted with complaints of severe leg pain and motor weakness. In both cases, intradicular disc herniation was diagnosed during surgery.
Results:
The patients had uneventful recovery. They had no complaints or neurological deficits 6 and 3 months after surgery, respectively.
Conclusions:
The possibility of an intradural disc herniation should be kept in mind for the success of the management of lumbar disc herniation. In some patients who did not benefit from surgery, intraradicular or intradural disc herniations may be the cause of failure.
Similar content being viewed by others
Introduction
Intradural lumbar disc herniation is a rare condition. It was reported that it accounted for 0.04–1.5% of lumbar disc herniations.1, 2 Intradural lumbar disc herniation was first described by Dandy in 19423 who reported the clinical characteristics of this rare phenomenon in his article. Intraradicular disc herniation is much rarer than the intradural herniation. There are reported 101 cases with intradural disc herniation in literature to date,2, 3, 4, 5, 6, 7, 8, 9 and only 17 of these herniations are intraradicular.2, 5, 7, 8, 9 Owing to the limited experience with this condition, and to its nonspecific presentation, the diagnosis of intradural disc herniation is difficult, and it is frequently diagnosed during surgery.
We report two cases with lumbar intraradicular disc herniation diagnosed during surgery.
Case reports
Case 1: A previously healthy 46-year-old man was admitted with complaints of low-back-pain and right sciatica for one and half month. The pain did not relieve with medical therapy. Initial neurological examination revealed that the abnormal signs were confined to the legs. There was no wasting but weakness of right knee extension. Knee jerks were symmetrical but the right ankle jerk was diminished. Plantar reflexes were flexor. Sensory testing showed reduced sensation to touch, and pin prick on the right L3 dermatoma. Straight leg raising was limited to 60° on the right side because of pain.
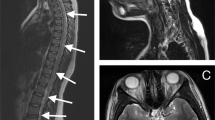
Magnetic resonance imaging (MRI) revealed a large disc herniation at the L2–3 level on sagittal sections (Figure 1a). There was an irregularity between the disc fragment and the root on axial section (Figure 1b). The patient was operated on under magnification with a binocular loop and headlight. Right L2–3 interlaminar fenestration and foraminotomy were performed to remove ruptured disc. The disc fragment was tightly adherent to the ventral dura and posterior longitudinal ligament. Exploration revealed that extruded disc fragment penetrated the dural sleeve of the right L3 root. The fragment was removed in toto. The anterior dural tear of the root sleeve was repaired with a piece of muscle. The patient had an uneventful recovery and was discharged on the second day of the operation. At the last follow-up examination, 6 months after the operation, the patient had no complaints and no neurological deficits.
Case 2: A 37-year-old woman was admitted with complaints of low-back pain and severe left sciatica that have started immediately after lifting a heavy object three days ago. She had been operated for left L5–S1 lumbar disc herniation by left L5–S1 interlaminary fenestration in another center 4 years ago. On neurological examination, there was weakness of plantar flexion of left ankle. Knee jerks were symmetrical but the left ankle jerk was abolished. Plantar reflexes were flexor. Sensory testing showed reduced sensation to touch, and pin prick on the left S1 dermatoma. Straight leg raising was limited to 60° on the right side because of pain.
Lumbar MRI examination showed a large disc herniation with irregular contours at L5–S1 level (Figure 2a and b).
The patient was operated on, and left L5–S1 interlaminary fenestration and foraminotomy were performed under illumination of a headlight and magnification of a binocular loop. There was no extruded fragment or protrusion of disc. The left S1 nerve root was found to be swollen and immobile, and the disc fragment could not be seen. Therefore, a longitudinal incision was made on the dural sleeve of left S1 root and the free intradural disc fragment was removed. The compressed S1 root was relieved. The dural tear of the root sleeve was repaired with a piece of muscle and primary suturing. Patient was free of pain postoperatively and was discharged on the second day of the operation. At the last follow-up examination, 3 months after operation, the patient had no complaints and no neurological deficits.
Discussion
Intradural disc herniation is a rare clinical entity, and intraradicular disc herniation, as a special type of intradural heniation, is much rarer. However, intradural and intraradicular disc herniations must be considered in the differential diagnosis of the lesions causing nerve root compression or cauda equina syndrome. Intraradicular disc herniation was first described in 1984 by Barbera et al.9 Since then, 17 cases were reported in literature.2, 5, 7, 8
Mut et al7 classified intradural disc herniations as type A and type B. In type A, the herniation is into the dural sac, and in type B, is into the dural sleeve at the preganglionic region of the nerve root.
The pathophysiology of intradural disc herniations is not known clearly. The postulated mechanism is adhesions between the dura mater and the posterior longitudinal ligament due to spondylotic changes, chronic inflammation, repeated minor trauma or previous surgery in both Type A and Type B.7, 10 An anatomical investigation revealed nonseparable dense adhesions between the ventral dura and the posterior longitudinal ligament at the L4–5 level in eight of 40 cadavers.11 Intradural disc herniations are most frequently seen at that level.6 Yildizhan et al12 found loose connections between the dura and the posterior longitudinal ligament in most cases, but in some cases there are tight connections at the lower lumbar, lower thoracic and lower cervical regions, most frequently at the L4–5, L3–4, L5–S1, C5–6 and C6–7 interspaces.12 A fresh cadaver study in adults by Spencer demonstrated presence of dural ligaments from the main dural sac to the posterior longitudinal ligament and to the vertebral body periosteum proximal to the intervertebral disc that fix the dura and nerve roots at their exits.13 Therefore, extruded fragment of the disc may tear the ventral side of the dura. These adhesions may be congenital,9 or acquired, and acquired adhesions are especially seen in previously operated cases.7, 10 The second case presented here had also undergone a previous lumbar disc surgery at same level and same side with the intraradicular disc herniation.
The involved levels with intraradicular disc herniation are L5–S1 and L4–5 in most of the cases.2, 7, 8 In one of our cases, the herniation was at L5–S1 level, but in the other, at L2–3 level. This is the first case with L2–3 intraradicular disc herniation in literature.
Owing to the limited experience with this condition, and to its nonspecific presentation, the diagnosis of intradural disc herniation is difficult, and it is frequently diagnosed during surgery as in our cases.6 There were only a few MRI reports of intradural disc herniations. Jenkins14 reported good MRI visualization of the intradural fragment as a hyperintense mass which continued from the intervertebral space to the spinal canal in a case of recurrent lumbar disc herniation. Holtas15 reported that coronal images were useful to detect the widening of the subarachnoid space, and that T2-weighted images showed an increased signal intensity area indicating the presence of adhesions and inflammatory reaction. Hida et al4 in their case revealed the usefulness of Gd-DTPA enhanced MRI, which showed a beak-like mass with ring-like enhancement except at the ventral surface at the level of intervertebral space. They reported that this ring-like enhancement was not due to the inflammatory process but due to venous plexus covering the disc fragment.
In the first case reported here, the disc fragment was seen as a beak-like hypointense mass with irregular contours on T2-weighted MRI, and in the other, it was seen as an irregular contoured, heterogeneous lesion. In the last one, the fragment had a hyperintense center with hypointense rim. However, there were not MRI sections with contrast injection, because we did not suspect intraradicular disc herniation preoperatively. Intraradicular disc herniations were also diagnosed during surgery in all reported cases in literature.2, 5, 7, 8
In our cases, we used headlight and binocular loop in operation, because we frequently use these instruments in lumbar disc herniation operations. In our opinion, illumination and magnification with headlight and magnifier, or with operation microscope are mandatory in the cases with intradural disc herniations.
It is not clear that it is necessary to repair dural openings in such cases because the reported cases are only unique case reports in literature. However, in many of the cases, it was reported that the dura was repaired with either primary suturing, or glue application.3, 4, 6, 7 We repaired the dura in the first patient with a piece of muscle, and in the second case, with primary suturing and a piece of muscle, and glue was not used. In both patients, cerebrospinal fluid leakage was not seen. Therefore, we recommend dural repair in these cases, if possible.
Conclusions
In treatment of lumbar disc disease, the possibility of an intradural disc herniation should be kept in mind for the success of the management of lumbar disc. In some patients who did not benefit from surgery, intraradicular or intradural disc herniations may be the cause of failure. If protruded or extruded disc fragment is not seen during operation, if the root is swollen, and if the level is right, intradural or intraradicular disc herniation must be considered and intradural exploration must be done carefully.
References
Schisano G, Nina P . Intraradicular lumbar disc herniation: case report and review of the literature. Neurosurgery 1998; 43: 400.
Suzer T, Tahta K, Coskun E . Intraradicular lumbar disc herniation: case report and review of the literature. Neurosurgery 1997; 41: 956–959.
Hidalgo-Ovejero AM, Garcia-Mata S, Gozzi-Vallejo S, Izco-Cabezon T, Martinez-Morentin J, Martinez-Grande M . Intradural herniation and epidural gas: Something more than a causal association? Spine 2004; 29: E463–E467.
Hida K, Iwasaki Y, Abe H, Shimazaki M, Matsuzaki T . Magnetic resonance imaging of intradural lumbar disc herniation. J Clin Neurosci 1999; 6: 345–347.
Mercier P et al. Intradural lumbar disk hernias. Apropos of 6 cases and review of the literature. Neurochirurgie 1997; 43: 142–147.
Mithöfer K, Rachlin JR, Kleefield J, Mendel JB, Glazer PA . Intradural lumbar vertebral disk herniation: a case report and review. Orthopedics 2002; 25: 437–439.
Mut M, Berker M, Palaoglu S . Intraradicular disc hernations in the lumbar spine and a new classification of intradural disc herniations. Spinal Cord 2001; 39: 545–548.
Schisano G, Franco A, Nina P . Intraradicular and intradural lumbar disc herniation: experiences with nine cases. Surg Neurol 1995; 44: 536–543.
Barbera J, Gonzales-Darder J, Garcia-Vazquez F . Intraradicular herniated lumbar disc: case report. J Neurosurg 1984; 60: 858–860.
Epstein NE, Syrquin MS, Joseph JA, Decker RE . Intradural disc hemiations in the cervical, thoracic, lumbar spine: report of three cases and review of the literature. J Spinal Disord 1990; 3: 396–403.
Blikra G . Intradural herniated lumbar disc. J Neurosurg 1969; 31: 676–679.
Yildizhan A, Pasaoglu A, Otken T, Ekinci N, Aycan K, Aral O . Intradural disc herniations pathogenesis, clinical picture, diagnosis and treatment. Acta Neurochir 1991; 110: 160–165.
Spencer DL, Irwin GS, Miller JA . Anatomy and significance of fixation of the lumbosacral nevre roots in sciatica. Spine 1983; 8: 672–679.
Jenkins LE, Bowman M, Coder HB, Gildenberg PL . Intradural herniation of a lumbar intervertebral disc. J Spinal Disord 1989; 2: 196–200.
Holtas S, Nordstorm CH, Larsson EM, Petterson H . MR imaging of intradural disk herniation. Comput Assist Tomogr 1987; 11: 353–356.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Karabekir, H., Karagoz Guzey, F., Kagnici Atar, E. et al. Intraradicular lumbar disc herniation: report of two cases. Spinal Cord 44, 318–321 (2006). https://doi.org/10.1038/sj.sc.3101860
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101860