Abstract
Study design
Retrospective multicenter study.
Objectives
Although surgery is frequently selected for the treatment of idiopathic spinal cord herniation (ISCH), its impact on functional outcomes has yet to be fully understood given the limited number of patients in previous studies. This study aims to evaluate the symptomatic history and surgical outcomes of ISCH.
Setting
Three institutions in Japan.
Methods
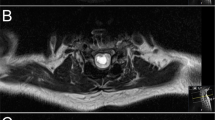
A total of 34 subjects with ISCH were retrospectively enrolled and followed up for at least 2 years. Demographic information, imaging findings, and clinical outcomes were collected. Functional status was assessed using the JOA score.
Results
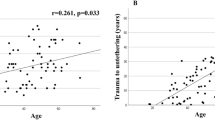
The types of neurologic deficit were monoparesis, Brown–Sequard, and paraparesis in 5, 17, and 12 cases, with their mean disease duration being 1.2, 4.2, and 5.8 years, respectively. Significant differences in disease duration were observed between the monoparesis and Brown–Sequard groups (p < 0.01) and between the monoparesis and paraparesis groups (p = 0.04). Surgery promoted significantly better recovery rates from baseline. Correlations were observed between age at surgery and recovery rate (p < 0.01) and between disease duration and recovery rate (p = 0.04). The mean recovery rates were 82.6%, 51.6%, and 29.1% in the monoparesis, Brown–Sequard, and paraparesis groups, respectively. The monoparesis group had a significantly higher recovery rate than did the Brown–Sequard (p = 0.045) and paraparesis groups (p < 0.01).
Conclusions
Longer disease duration was correlated with the progression of neurologic deficit. Older age, and worse preoperative neurologic status hindered postoperative functional recovery. These results highlight the need to consider surgical timing before neurologic symptoms deteriorate.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
References
Wortzman G, Tasker RR, Rewcastle NB, Richardson JC, Pearson FG. Spontaneous incarcerated herniation of the spinal cord into a vertebral body: a unique cause of paraplegia. Case report. J Neurosurg. 1974;41:631–5.
Barrenechea IJ, Lesser JB, Gidekel AL, Turjanski L, Perin NI. Diagnosis and treatment of spinal cord herniation: a combined experience. J Neurosurg Spine. 2006;5:294–302.
Berg-Johnsen J, Ilstad E, Kolstad F, Zuchner M, Sundseth J. Idiopathic ventral spinal cord herniation: an increasingly recognized cause of thoracic myelopathy. J Cent Nerv Syst Dis. 2014;6:85–91.
Groen RJ, Middel B, Meilof JF, de Vos-van de Biezenbos JB, Enting RH, Coppes MH, et al. Operative treatment of anterior thoracic spinal cord herniation: three new cases and an individual patient data meta-analysis of 126 case reports. Neurosurgery. 2009;64:ons145–59.
Hassler W, Al-Kahlout E, Schick U. Spontaneous herniation of the spinal cord: operative technique and follow-up in 10 cases. J Neurosurg Spine. 2008;9:438–43.
Imagama S, Matsuyama Y, Sakai Y, Nakamura H, Katayama Y, Ito Z, et al. Image classification of idiopathic spinal cord herniation based on symptom severity and surgical outcome: a multicenter study. J Neurosurg Spine. 2009;11:310–9.
Maira G, Denaro L, Doglietto F, Mangiola A, Colosimo C. Idiopathic spinal cord herniation: diagnostic, surgical, and follow-up data obtained in five cases. J Neurosurg Spine. 2006;4:10–9.
Massicotte EM, Montanera W, Ross Fleming JF, Tucker WS, Willinsky R, TerBrugge K, et al. Idiopathic spinal cord herniation: report of eight cases and review of the literature. Spine. 2002;27:E233–41.
Nakamura M, Fujiyoshi K, Tsuji O, Watanabe K, Tsuji T, Ishii K, et al. Long-term surgical outcomes of idiopathic spinal cord herniation. J Orthop Sci. 2011;16:347–51.
Prada F, Saladino A, Giombini S, Erbetta A, Saini M, DiMeco F, et al. Spinal cord herniation: management and outcome in a series of 12 consecutive patients and review of the literature. Acta Neurochir. 2012;154:723–30.
Watanabe M, Chiba K, Matsumoto M, Maruiwa H, Fujimura Y, Toyama Y. Surgical management of idiopathic spinal cord herniation: a review of nine cases treated by the enlargement of the dural defect. J Neurosurg. 2001;95:169–72.
Groen RJM, Lukassen JNM, Boer GJ, Vergeer RA, Coppes MH, Drost G, et al. Anterior thoracic spinal cord herniation: surgical treatment and postoperative course. an individual participant data meta-analysis of 246 Cases. World Neurosurg. 2019;123:453–63.e15.
Hirabayashi K, Miyakawa J, Satomi K, Maruyama T, Wakano K. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine. 1981;6:354–64.
Aizawa T, Sato T, Tanaka Y, Kotajima S, Sekiya M, Kokubun S. Idiopathic herniation of the thoracic spinal cord: report of three cases. Spine. 2001;26:E488–91.
Nakazawa H, Toyama Y, Satomi K, Fujimura Y, Hirabayashi K. Idiopathic spinal cord herniation. Report of two cases and review of the literature. Spine. 1993;18:2138–41.
Zappala M, Lightbourne S, Heneghan NR. The relationship between thoracic kyphosis and age, and normative values across age groups: a systematic review of healthy adults. J Orthop Surg Res. 2021;16:447.
Ohtake Y, Senoo M, Fukuda M, Ishida Y, Yoshihara R, Ishikawa K, et al. Symptomatic interdural cerebrospinal fluid collections after surgery for idiopathic spinal cord herniation: illustrative case. J Neurosurg Case Lessons. 2021;2:CASE21232.
Gaudino S, Colantonio R, Schiarelli C, Martucci M, Calandrelli R, Botto A, et al. Postoperative MR imaging of spontaneous transdural spinal cord herniation: expected findings and complications. AJNR Am J Neuroradiol. 2016;37:558–64.
Nakashima H, Kanemura T, Yagi H, Kato F, Sato K, Kamiya M, et al. Factors affecting the severity of neurological disorders in thoracic idiopathic spinal cord herniation. Spine. 2018;43:1552–8.
Funding
No funds were received in support of this work.
Author information
Authors and Affiliations
Contributions
YH and NN designed the research. YH, NN, HK, TI performed data collection. YH and NN analyzed the data and wrote the paper. OT, HK, TI, SS, YT, SN, MY, MM, MN, and KW supervised the study. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics
This study received ethical approval from the institutional review boards of the participating institutions (20110142). Informed consent was obtained from all subjects
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hirose, Y., Nagoshi, N., Tsuji, O. et al. Natural history and surgical outcomes of idiopathic spinal cord herniation. Spinal Cord 61, 441–446 (2023). https://doi.org/10.1038/s41393-023-00904-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-023-00904-3