Abstract
Objective:
To report a case of brachial diplegia with normal lower limb power, after a cervical cord injury.
Design:
Case report of a 63-year-old man who sustained a neck trauma following a fall.
Setting:
Department of Neurology, University Hospitals of Leicester, Royal Infirmary, Leicester, UK.
Case report:
The mechanism of the injury was probably one of hyperflexion resulting in central cervical cord contusion. Initial neurological examination revealed brachial diplegia, with posterior column sensory involvement of the lower limbs which had normal power. The patient was also in urinary retention but had no respiratory involvement. Magnetic resonance imaging (MRI) of the spinal cord showed a hyperintense signal in the central mid-cervical cord.
Conclusion:
Pure brachial diplegia represents a rare clinical presentation of cervical cord pathology, including trauma, of which clinicians should be aware.
Similar content being viewed by others
Introduction
Isolated brachial diplegia is a rare but known potential consequence of cervical spinal cord pathology. It was described initially by Dide and Lhermitte1 as early as 1917, and has been thought to relate to central spinal cord injury by Schneider et al.2 We here report the case of a man who after a neck trauma, had such a clinical presentation, with magnetic resonance imaging (MRI) findings compatible with central cervical cord contusion.
Case report
A 63-year-old man was admitted to our unit with weak upper limbs and unsteady gait, after a fall at his home, which had occurred in the stairs and which had resulted in an occipitonucchal injury. He had a history of diabetes, alcohol abuse and chronic obstructive pulmonary disease. On admission, he complained of severe neck pain. He was unable to perform any movement with the right upper limb, all myotomes from C5 to T1 being affected. The power in the left upper limb was, for all muscles, of grade 2 on the Medical Research Council (MRC) scale. Lower limb power was entirely normal. Sensation was reduced to pin-prick in the arms in a patchy distribution, but severely impaired to all modalities in the legs, with total loss of joint position sense and vibration sense, a positive Romberg's sign, impaired heel on shin testing on eye closure, and gait ataxia of the sensory type. There was no clear sensory level. Reflexes were absent in the upper limbs but brisk in the lower limbs with extensor plantar responses. The patient was found to be in urinary retention and was catheterized. Respiratory function was unimpaired. Cranial nerve functions were preserved and no Horner's syndrome was present on either side.
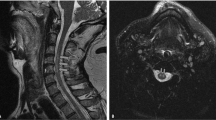
MRI demonstrated advanced degenerative changes in the cervical spine with dehydration of the discs and protrusions at C5/C6 and C6/C7 levels. Hyperintensity on sagittal T2-weighted images was visible within the cord substance between C4 and C6 (Figure 1). Transverse sections images were severely degraded by artifact (not shown). All routine blood investigations were otherwise normal. A MRI brain scan was performed to exclude a cerebral lesion in view of the clinical picture, and revealed a small right thalamic infarct, and mild generalized atrophy. The cervicomedullary junction was entirely normal. Nerve conduction studies were compatible with a mild generalized sensori–motor polyneuropathy consistent with the patient's diabetic condition. Electromyography, performed 3 weeks after presentation, showed no spontaneous activity in upper limb muscles, but severely reduced activation on voluntary contraction.
The patient was started on intravenous dexamethasone at the dose of 16 mg daily, which was tapered over 3 weeks. Very slow improvement took place, essentially for the left upper limb, which had reached a global power of 3 on the MRC scale 4 weeks after presentation. Right upper limb strength improved very little initially, and the patient did not recover normal bladder function. The sensory impairment remained unchanged. On review 9 months later, further improvement was observed. Upper limb power was of 4–5 on the MRC scale on the left, and 3–4 proximally on the right, although remaining of grade 1 for distal hand muscles, which were atrophied. Marked sensory loss was still present in the lower limbs, with persistent sensory ataxia, brisk reflexes and extensor plantar responses.
Discussion
We have here described a patient with brachial diplegia developing acutely, temporally related to a closed neck injury, which occurred as a result of a fall. The arm weakness, brisk lower limb reflexes, bilateral extensor plantars and urinary retention had led to the suspicion of a cervical cord lesion. However, man-in-the-barrel syndromes are generally caused by bilateral supratentorial involvement of the prerolandic cortical and subcortical area.3 This term was coined by JP Mohr because such patients appear as if their arms and trunk are constrained within a barrel, while their facial and leg muscles are free to move normally.4 The differential diagnosis otherwise also included cruciate paralysis due to a cervicomedullary lesion,5 which can be difficult to distinguish from a central cord syndrome purely on clinical grounds. A MRI brain scan was therefore also performed in this patient; however, not revealing any such findings to explain the presentation. The possibility of an acute bilateral brachial plexus involvement was excluded on the basis of nerve conduction studies and EMG. The cervical MRI findings were suggestive of a cord contusion, and compatible with an injury caused by hyperflexion of the neck, suggested by the occipitonucchal injury.
Brachial diplegia with normal leg strength has been rarely reported as presenting symptom of cervical cord lesions. Infarction,5, 6 and trauma1, 2, 7 have been described as underlying causes of such presentations. Fuentes et al.7 in 1984 described 10 patients in a series of 28 having sustained a cervical cord injury as presenting with brachial diparesis or diplegia without lower limb weakness. They mentioned variable underlying mechanisms, with hyperextension responsible in about half of all cases, and hyperflexion in a third.
Initially described by Dide and Lhermitte,1 brachial diplegia due to myelopathy has been attributed to acute central spinal cord injury by Schneider et al.2 These authors hypothesized that during hyperextension, the cervical cord is trapped anteriorly by an osteophytic bar and posteriorly by hypertrophied ligamentum flavum, resulting in central hematomyelia and necrosis with surrounding edema. This was based on what was believed to be the topographic arrangement of corticospinal tracts, with fibers subserving arm function being anteromedial and those subserving leg function, posterolateral. The anterior horn cells would be involved, resulting in a lower motor neuron type of injury, as in our patient, who had flaccid upper limb weakness and areflexia. As in this patient, the classic presentation is that of an older adult with pre-existing cervical spondylosis. The injury would result in predominantly upper limb weakness with preservation of lower limb power, sensory impairment of variable nature below the lesion and sphincter dysfunction.
Schneider et al's theory appears now debatable. Anatomical studies have shown intermingling of corticospinal tracts and MRI and postmortem studies have failed to demonstrate central cord necrosis, gray matter injury to motor neurons supplying hand muscles, or hematomyelia.8, 9 Interestingly, the injury was shown in these more recent studies to involve the white matter tracts, including but not limited to the cortocospinal tracts with the lesions appearing concentrated along the posterolateral aspect of the cord.
Although clinical presentations can clearly vary in central cord syndromes depending on the extent of the lesion and tracts affected, involvement being frequently very patchy,7 our case is a reminder that pure brachial diplegia mimicking a man-in-the-barrel syndrome of cerebral origin, can be a presenting symptom of cervical cord injury with central cord contusion. Despite its relative rarity, this clinical syndrome needs to be readily recognized by clinicians, and the relevant differentials excluded by brain and cervicomedullary junction imaging. Cervical traction, use of hard collars when cord edema is present and eventual decompressive surgery when underlying acute disc herniation or fracture/dislocation is present,10 all represent potential therapeutic measures to be offered without delay to such patients. It is impossible to say whether the steroid therapy, offered to our patient did or not have an impact on recovery which, in his case too, as in other previously reported cases, was unfortunately incomplete.
References
Dide M, Lhermitte J . La diplégie brachiale spasmodique consécutive aux blessures par coups de feu de la région cervicale. Progrès Méd 1917; 1: 1–3.
Schneider RC, Chery G, Pantek H . The syndrome of acute central cervical spinal cord injury. With special reference to the mechanism involved in hyperextension injuries of cervical spine. J Neurosurg 1954; 11: 546–577.
Georgiadis D, Schulte-Mattler WJ . Cruciate paralysis or man-in-the-barrel syndrome? Report of a case of brachial diplegia. Acta Neurol Scand 2002; 105: 337–340.
Mohr JP . Distal field infarction. Neurology 1969; 19: 279.
Berg D, Mullges W, Koltzenburg M, Bendszus M, Reiners K . Man-in-the-barrel syndrome caused by spinal cord infarction. Acta Neurol Scand 1998; 97: 417–419.
Renard JF et al. Diplégie brachiale par ischémie médullaire cervicale. Un cas. Rev Neurol (Paris) 1997; 153: 690–693.
Fuentes JM, Vlahovitch B, Negre C . La diplégie brachiale d’origine traumatique consécutive aux atteintes de la moëlle cervicale. Neurochirurgie 1984; 30: 165–170.
Quencer RM et al. Acute traumatic central cord syndrome: MRI-pathological correlations. Neuroradiology 1992; 34: 85–94.
Collignon F, Martin D, Lenelle J, Stevenaert A . Acute traumatic central cord syndrome: magnetic resonance imaging and clinical observations. J Neurosurg Spine 2002; 96: 29–33.
Guest J, Eleraky MA, Apostolides PJ, Dickman CA, Sonntag VK . Traumatic central cord syndrome: results of surgical management. J Neurosurg Spine 2002; 97: 25–32.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Rajabally, Y., Hbahbih, M., Messios, N. et al. Brachial diplegia as a result of cervical cord injury. Spinal Cord 43, 389–391 (2005). https://doi.org/10.1038/sj.sc.3101716
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101716