Abstract
Objective: The reproducibility and clinical reliability of perioperative somatosensory-evoked potentials (SSEP) were prospectively evaluated in uneventful scoliosis surgery. The influence of anesthesia owing to induction of total intravenous anesthesia (TIVA) upon preoperative SSEP and the variability of intraoperative SSEP were calculated. The potential effect of spine surgery was assessed by comparing pre- to postoperative SSEP.
Methods: A total of 2143 pre-, intra- and postoperative tibial and median SSEP recorded in 25 patients undergoing spine surgery owing to idiopathic scoliosis were analyzed. The anesthesia protocol consisted of a computerized target controlled infusion (TCI) device for propofol and intravenous application of an opioid.
Results: Anesthesia induced a significant and comparable prolongation of the tibial SSEP onset, P40 and P60 latencies, while the N50 latency was less changed. Throughout anesthesia, latencies of median (onset, N20, P25 and N35) and tibial (onset, P40, N50 and P60) SSEP showed mean variations of less than 6%. The intraoperative SSEP amplitudes were less stable with a relative standard deviation of 30–40%. In uneventful spine surgery, the postoperative tibial SSEP were not significantly changed in comparison to preoperative recordings.
Conclusions: By using a standardized anesthesia protocol, the impact of anesthesia on preoperative SSEP can be predicted. Furthermore, the controlled application of sedatives and analgesics allows recording of stable SSEP parameters for intraoperative monitoring purposes. As in uneventful spine surgery pre- to postoperative SSEP are unchanged the latter comparison can be applied as an additional perioperative neuromonitoring procedure to assess the influence of spine surgery or other invasive interventions on spinal cord function.
Similar content being viewed by others
Introduction
During spine surgery, that is, scoliosis, neurological deterioration may result from compression, stretching, vascular insufficiency or direct trauma of the spinal cord by instrumentation.1,2,3 To most of these complications, the surgeon is lacking intraoperative reliable warning criteria. To manage this limitation, the Stagnara wake up test is recommended, which, however, reveals inherent serious disadvantages like delayed diagnostic information, time-consuming procedure and discomfort for the patient.4,5,6 To overcome these problems, somato-sensory evoked potentials (SSEP) have been introduced for neurological investigation and monitoring of the integrity of the neural pathways during surgical procedures. This technique allows an on-line surveillance and early diagnosis of spinal cord dysfunction and aims to provide warning signals before an irreversible damage has occurred. Owing to the sensitivity and specificity of SSEP monitoring, the incidence of postoperative paraplegia can be significantly reduced.3,7,8,9,10
However, a reliable intraoperative monitoring demands appropriate procedures of anesthesia, since the anesthetic itself, as well as accompanying hypothermia and hypotension, have a serious influence on evoked potentials. The depressant effect of volatile anesthetics on evoked potentials is well known.11,12,13 While low-dose volatile anesthetics in combination with an opioid is considered as appropriate anesthesia for monitoring purpose, recent studies evaluated the performance of total intravenous anesthesia (TIVA) for intraoperative neuromonitoring with the combination of propofol and fentanyl.3,12,13,14,15,16,17,18
TIVA in combination with a target-controlled infusion (TCI) device allows the determination of the amount of applicated propofol and the estimation of the plasma propofol concentration. This allows long-lasting anesthesia and the possibility of comparable anesthesia.17,19,20
In the present study, the clinical reproducibility and reliability of pre-, intra- and postoperative SSEP recordings were assessed in uneventful scoliosis surgery. Firstly, the impact of anesthesia was calculated in an intersubject comparison of SSEP parameter differences between preoperative and intraoperative SSEP. Secondly, the intraoperative within-case variabilities of SSEP parameters were calculated, statistically analyzed and compared to available data in literature. Thirdly, to estimate the impact of surgical procedures and anesthesia on SSEP, postoperative SSEP were compared to the preoperative SSEP. The analysis of data should outline which SSEP markers can be applied for reliable perioperative (pre–intra–postoperative) monitoring as especially the suitability of postoperative SSEPs in the assessment of spinal cord function after spine surgery is not yet established.
Methods
Patients
In a prospective study, pre-, intra- and postoperative SSEP of 25 patients (mean age 16 (±8) years, range of 6–48 years; females to males=23:2) suffering from idiopathic scoliosis (26 surgical interventions performed between 1997 and 1999) were analyzed. Approval of the local ethic commission was achieved. Only patients suffering from idiopathic scoliosis (mean Cobb angle 60 (±11)°) without evidence of a neurological impairment, based on a full neurological examination, were included. In all patients, additional intraspinal lesions besides spinal deformity were excluded by radiological workup (X-ray and MRI).
In all patients a postoperative full neurological re-examination was performed to ascertain an unchanged normal neurological condition after spine surgery.
SSEP protocol
In all patients, multiple perioperative SSEP recordings consisting of pre-, intra- and postoperative measurements were performed. Preoperative tibial SSEP of the right and left lower limb were recorded 1 day before operation, while the postoperative control of tibial SSEP (at the same conditions as the preoperative SSEP) was performed in about 7 days (range 4–12 days) after spine surgery. Intraoperative monitoring consisted of median and tibial SSEP (left and right side) in parallel, in which the median SSEP was acting as a control for the tibial one.
For intraoperative assessment, a total of 2049 intraoperative SSEP measurements of 25 patients undergoing 26 surgical interventions were analyzed; a mean average of 13 (±6) SSEP recordings of each median nerve and 26 (±14) of each tibial nerve were performed per operation.
For comparison of pre- to intraoperative SSEP, the preoperative left and right tibial SSEP of the same 25 patients were individually compared to the corresponding averaged intraoperative tibial left and right SSEP.
Of the 25 patients, 21 underwent a postoperative control SSEP to compare the pre- to postoperative SSEP (42 tibial (21 left/21 right) postoperative SSEP were compared to the corresponding 42 preoperative tibial SSEP).
For calculation procedures, SSEP parameters were labeled the following way: P1, N1, P2 and N2 corresponding to P40, N50, P60 and N75, respectively, for tibial SSEP and N1, P1, N2 corresponding to N20, P25 and N35, respectively, for median SSEP.
For calculation of SSEP latency changes, latencies (onset, P1, N1, P2 and N2) as well as interpeak latencies (onset −P1, P1−N1, N1−P2 and P2−N2) were determined. The size of amplitudes was calculated by baseline to first peak and peak to peak for the remaining markers. Figure 1 shows the position of the tibial SSEP markers. All markers were set by a single person to reduce variability. He was blinded for the patients history, operative procedures and statistical analysis.
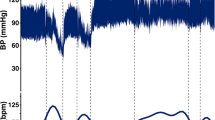
Comparison of pre- and intraoperative tibial SSEP showing the mean changes during stable anesthesia. According to the international nomenclature, positive peaks are represented by downward deflections and labeled P and negative peaks are represented by upward deflections and labeled N. The following latencies were measured: P40 (=P1), N50 (=N1), P60 (=P2) and N75 (=N2). Amplitudes were measured baseline to peak for onset-P1 and peak to peak for the other amplitudes (P1−N1 and N1−P2)
SSEP recordings
The tibial and median SSEP were elicited by electrical stimulation (square-wave stimulation of 200 μs at a frequency of 3 Hz) at the ankle or wrist (using surface electrodes in pre-/postoperative stimulation and needle electrodes during operation; proximally placed cathodes, the anode places 2 cm distally) by a conventional EMG machine (Dantec Keypoint®, Medtronic Functional Diagnostics, Denmark for pre-/postoperative recordings; Neurowacs®, Inomed, Germany for intra-operative recordings). Stimulation intensity in the awake patient was chosen two to three times above the sensory threshold, while during surgery at least 30 mA was applied to induce reproducible SSEP responses.
For recording, scalp electrodes (cup electrodes for pre-/postoperative recordings and needle electrodes for intraoperative recordings) were applied at Cz'/Fz and C3'/C4'/Fz using the International 10/20 electrode system. The electrode impedance was maintained below 5 kΩ. The amplifier was set at 5 μV/division, frequency bandpass was set at 50–2000 Hz. Two sets of 500 replications were averaged to improve the signal-to-noise ratio for latency and amplitude measurements.
Anesthesia
All surgical procedures were performed using TIVA. The patients were premedicated with oral 0.1 mg/kg body weight midazolam (Dormicum®, Roche, Basel, Switzerland). After preoxygenation, anesthesia was induced with intravenous propofol (Disoprivan®, Astra Zeneca, Zug, Switzerland) 4–6 mcg/ml blood concentration using a TCI device based on the pharmacokinetic data set from March and Gepts until loss of consciousness.21 Muscle relaxation was obtained for tracheal intubation by a single intravenous dose of 0.8 mg/kg body weight rocuronium (Esmeron®, Organon Technika AG, Pfäffikon, Switzerland). No other muscle relaxation was performed during the whole surgical procedure. Analgesia was provided 2 min before intubation with intravenous 0.2 mg fentanyl (Sintenyl®, Sintetica, Mendrisio, Switzerland), with repeated increments of 0.1 mg during surgery in order to maintain blood pressure and pulse measurements in a range of 80–120% of the baseline values. The maintenance of the anesthesia occurred at a fixed TCI value of 250% the noted effect site concentration at the time of loss of consciousness, providing a concentration over the known ED99 for propofol anesthesia. After positioning for surgery (prone position or lateral position for dorsal or ventral surgical spine access, respectively), the FiO2 was reduced from 1.0 to 0.4, unless higher values were needed in order to maintain a SpO2 value over 95%.
For maintenance of stable body core temperature, perfusion warming and heating blankets were applied.
Statistics
Statistical evaluations were performed by using a SAS software package (SAS Institute Inc., Cary, NC, USA). To make the comparisons between the pre- and intraoperative and the pre- and postoperative SSEP, a paired t-test was used (P<0.016 was considered as significant). Regression analysis was performed between pre- and intraoperative SSEP. A t-test was used to assess significant intraoperative variation of the SSEP. To evaluate the stability of intraoperative latencies and amplitudes, mean and relative standard deviations were calculated. To compare the intraoperative variation of the median and tibial SSEP, a Wilcoxon test was performed. If not otherwise noted, P<0.05 was considered as significant.
Results
Influence of stable TIVA on preoperative tibial SSEP
After achieving a stable level of anesthesia, the comparison of pre- to intraoperative tibial SSEP was statistically analyzed for latencies and inter-peak latencies. Owing to different recording technique (cup electrodes for preoperative versus needle electrodes for intraoperative recordings), amplitudes could not be statistically calculated.
Intraoperative tibial SSEP latencies (mean±SD) of onset (31.9±2.8–34.4±3.4 ms), P1 (36.7±2.7–37.8±3.7 ms) and P2 (57.1±6.4–65.5±7.3 ms) were significantly prolonged, while the latency of N1 (46.1±3.4–46.4±5.3 ms) showed no significant changes (Figure 1, Table 1). Interpeak latencies showed no changes for P1−N1 (9.3±2.9–8.6±3.3 ms), while the interpeak latency of onset −P1 (4.8±1.6–3.4±1.1 ms) and N1−P2 (11.1±4.3–19±4.5 ms) were significantly altered.
Intraoperative amplitudes were strongly reduced in comparison to preoperative recordings. Although the reduction of amplitudes should be induced by anesthesia, statistical analysis was not performed due to the different recording techniques. Analysis of variance and regression analysis for all the peak and interpeak latencies was performed to assess how far the changes of tibial SSEP parameters can be predicted. We found a significant and linear relation between pre- and intraoperative values for latencies and interpeak latencies of onset, P1 and N1, which allows a prediction of changes due to a stable level of anesthesia (Table 1 and Figure 2).
Intraoperative variability of SSEP
Absolute and relative mean standard deviations of median and tibial SSEP during spine surgery were analyzed to assess the variability of peak and interpeak latencies and amplitudes (Table 3).
In both tibial and median SSEP recordings, the variability of latency markers were in mean less than 4% and for interpeak latencies below 25%, which corresponds to less than 3 ms as absolute values. The amplitudes in general showed a higher variability. Mean changes of early SSEP amplitudes of onset −peak 1 and peak 1 −peak 2 were of about 30% for tibial and median SSEP. The late amplitude of peak 2 −peak 3 of tibial nerve revealed a variability in mean of about 150% in contrast to median SSEP of about 36% (Table 3).
To assess a difference in variability between median and tibial SSEP, the variability (SD) of the corresponding peaks, interpeaks and latencies were compared by Wilcoxon test between the median and tibial SSEP.
All the peak and interpeak latencies (onset, peak 1, peak 2 and peak 3) were significantly (P<0.05) more stable in the median SSEP (see Table 3).
While the variability of amplitude of onset −peak 1 did not show a difference between median and tibial SSEP, the amplitudes of peak 1 −peak 2 and peak 2 −peak 3 were significantly more stable in the tibial SSEP (Table 3).
Comparison of pre- and postoperative tibial SSEP
To assess the reproducibility of tibial SSEP after uneventful surgical treatment, corresponding SSEP obtained pre- and postoperatively were compared. Absolute changes of the calculated peaks (ms), interpeaks (ms) and amplitudes (μV) and relative changes (%) were compared (Table 2).
The postoperative tibial SSEP showed only a significantly increased latency of onset of 0.73±1.19 ms, while the other latency markers were not significantly changed. Comparison of the relative differences between pre- and postoperative SSEP showed that the mean changes of all the latencies, whether the difference was significant (onset) or not (P1, N1, P2 and N2), were less than 3%.
The amplitudes of onset −P1 and N1 −P2 were significantly reduced, while the amplitude P1−N1 was unchanged postoperatively. However, the mean changes of all the amplitudes were less than 10% compared to the preoperative values (Table 2).
Discussion
The assessment of sequential perioperative SSEP recordings (pre-, intra-, postoperative) in scoliosis surgery revealed several clinically relevant findings. Anesthesia by computer-assisted TIVA induces predictable changes of tibial SSEP markers with valuable intraoperative variability of SSEP recordings. The reassessment of early SSEP markers (latencies and amplitudes of tibial SSEP) can be applied for postoperative follow-up examinations, as they remain unchanged in uneventful spine surgery. Therefore, perioperative SSEPs can be applied supplementary to clinical examinations, as postoperative follow-up recordings are able to assess the deterioration of spinal cord function due to surgical or systemic affections.
Although not extensively evaluated, it is assumed that preoperative SSEP are of limited use for monitoring purpose, as several factors are known to affect intraoperative SSEP (ie anesthetic drugs, reduced core temperature, hypotension).22,23,24 However, the present findings reveal that by application of computer-assisted TIVA characteristic changes of early SSEP components can be predicted. This allows to distinguish changes of intraoperative SSEP parameters, which are not induced by the anesthesia. The comparable intersubject levels of anesthesia due to the computer-assisted propofol application induces intraoperative SSEP changes that can be reliably predicted.18,19,20,25 The influence of midazolam used for premedication can be neglected, as several studies showed no or only a transient effect on SSEP latencies.22,26,27 Also the application of low doses of opioids (fentanyl) is not supposed to induce the predictable changes on SSEP latencies.18,22,28
The intraoperative within-case variability of SSEP is of relevance in performing neuromonitoring during surgery.29,30,31 It is of importance to determine the range of SSEP variability, which can be expected due to specific protocols of anesthesia.31 This defines the borders for changes of latency and amplitude for giving relevant warning signals with high sensitivity and specificity to avoid false-negative and -positive warnings.23 Comparing the within-case variability of intraoperative SSEP during scoliosis surgery, the performance of TIVA with application of propofol by TCI showed a favorable low variability of early components competitive to volatile narcosis based on nitrous oxide plus opioid.29 The within-case variability in serial intraoperative SSEP over 60 min in minor spine surgery under propofol in TIVA without computer-assistance showed a comparable extent.31 However, the presented results can only be indirectly compared to data published, as the within-case variability is also dependent on different disorders and clinical conditions.29,31,32,33 The evaluation of intraoperative SSEP variability by using interindividual comparison of SSEP was not applied in this study, as the intraindividual variability should be superior for monitoring purposes.33,34,35
Comparing the intraoperative intraindividual variability of the median and tibial SSEP, a significant smaller variability of median SSEP latencies was found. Whether this difference is due to the different and longer pathways of the tibial SSEP or the influence of surgical procedure on spinal cord is questionable and there are no conclusive data in literature to this point.
The literature is sparse with regards to the influence of spine correction surgery of idiopathic scoliosis on preoperative tibial SSEP markers and the subsequent possibility of follow-up examinations.30,36 This study showed that early SSEP components are not significantly influenced by uneventful spine surgery and can therefore be used for follow-up examinations. This generally enables to assess if spinal cord function is affected by surgery or other invasive interventions. Furthermore, the preservation of spinal cord function can be documented by tibial SSEP in serial follow-up examinations which can be advantageous in specific patients after spinal deformity correction. Patients suffering from idiopathic scoliosis undergoing spine surgery are frequently adolescents and in time may develop neurological deficits due to other clinical diseases, where SSEP recordings can still be used for diagnostic purposes.
In conclusion, SSEP changes because of the effects of anesthesia are predictable and stable during surgery which allows to distinguish SSEP changes due to anesthesia from other compromises. As pre- to postoperative tibial SSEP are not changed in uneventful spine surgery, perioperative SSEP can be applied as an additional perioperative neuromonitoring procedure. This enables to distinguish changes of spinal cord function due to operative procedures from preoperative conditions, and also in time from potentially developing disorders not related to spine surgery.
References
Apel DM et al. Avoiding paraplegia during anterior spinal surgery. The role of somatosensory evoked potential monitoring with temporary occlusion of segmental spinal arteries. Spine 1991; 16(8 Suppl): 365–370.
Loder RT, Thomson GJ, LaMont RL . Spinal cord monitoring in patients with nonidiopathic spinal deformities using somatosensory evoked potentials. Spine 1991; 16: 1359–1364.
Waller CS, Paterson JMH, Edgar MA, Jones SJ . Incidence of spinal cord impairment related to extent of SEP decline and recovery, etiology and instrumentation in operations for scoliosis. In: Shimoij K, Kurokawa T, Tamaki T, Willis Jr WD, (eds). Spinal Cord Monitoring and Electrodiagnosis. Springer-Verlag: Heidelberg 1991, pp 353–359.
Fisher RS, Raudzens P, Nunemacher M . Efficacy of intraoperative neurophysiological monitoring. J Clin Neurophysiol 1995; 12: 97–109.
Padberg AM, Wilson-Holden TJ, Lenke LG, Bridwell KH . Somatosensory- and motor-evoked potential monitoring without a wake-up test during idiopathic scoliosis surgery. An accepted standard of care. Spine 1998; 23: 1392–1400.
Macri S et al. Intra-operative spinal cord monitoring in orthopaedics. Spinal Cord 2000; 38: 133–139.
Lesser RP et al. Postoperative neurological deficits may occur despite unchanged intraoperative somatosensory evoked potentials. Ann Neurol 1986; 19: 22–25.
Chatrian GE, Berger MS, Wirch AL . Discrepancy between intraoperative SSEP's and postoperative function. Case report. J Neurosurg 1988; 69: 450–454.
Epstein NE, Danto J, Nardi D . Evaluation of intraoperative somatosensory-evoked potential monitoring during 100 cervical operations. Spine 1993; 18: 737–747.
Keith RW, Stambough JL, Awender SH . Somatosensory cortical evoked potentials: a review of 100 cases of intraoperative spinal surgery monitoring. J Spinal Disord 1990; 3: 220–226.
McPherson RW, Mahla M, Johnson R, Traystman RJ . Effects of enflurane, isoflurane, and nitrous oxide on somatosensory evoked potentials during fentanyl anesthesia. Anesthesiology 1985; 62: 626–633.
Andoh T, Okumura F . Effect of anaesthetics on somatosensory and motor evoked potentials in humans. In: Stalberg E, Sharma HS, Olsson Y (eds). Spinal Cord Monitoring. Springer: Wien, New York 1998, pp 491–508.
Langeron O et al. Effects of propofol, propofol–nitrous oxide and midazolam on cortical somatosensory evoked potentials during sufentanil anaesthesia for major spinal surgery. Br J Anaesth 1999; 82: 340–345.
Koht A . Anesthesia and evoked potentials: overview. Int J Clin Monit Comput 1988; 5: 167–173.
Kalkman CJ, Traast H, Zuurmond WW, Bovill JG . Differential effects of propofol and nitrous oxide on posterior tibial nerve somatosensory cortical evoked potentials during alfentanil anaesthesia. Br J Anaesth 1991; 66: 483–489.
Taniguchi M, Nadstawek J, Pechstein U, Schramm J . Total intravenous anesthesia for improvement of intraoperative monitoring of somatosensory evoked potentials during aneurysm surgery. Neurosurgery 1992; 31: 891–897.
Ravussin P, de Tribolet N, Wilder-Smith OH . Total intravenous anesthesia is best for neurological surgery. J Neurosurg Anesthesiol 1994; 6: 285–289.
Laureau E et al. Comparative study of propofol and midazolam effects on somatosensory evoked potentials during surgical treatment of scoliosis. Neurosurgery 1999; 45: 69–74.
Fechner J et al. Predictability and precision of “target-controlled infusion” (TCI) of propofol with the “Disoprifusor TCI” system [Article in German]. Anaesthesist 1998; 47: 663–668.
Swinhoe CF, Peacock JE, Glen JB, Reilly CS . Evaluation of the predictive performance of a ‘Diprifusor’ TCI system. Anaesthesia 1998; 53(Suppl): 61–67.
Gepts E, Camu F, Cockshott ID, Douglas EJ . Disposition of propofol administered as constant rate intravenous infusions in humans. Anesth Analg 1987; 66: 1256–1263.
Koht A et al. Effects of etomidate, midazolam, and thiopental on median nerve somatosensory evoked potentials and the additive effects of fentanyl and nitrous oxide. Anesth Analg 1988; 67: 435–441.
Nuwer MR . Spinal cord monitoring. Muscle Nerve 1999; 22: 1620–1630.
Shen WJ et al. Routine preoperative MRI and SEP studies in adolescent idiopathic scoliosis. J Pediatr Orthop 1996; 16: 350–353.
Scheepstra GL, de Lange JJ, Booij LH, Ros HH . Median nerve evoked potentials during propofol anaesthesia. Br J Anaesth 1989; 62: 92–94.
Sloan TB, Fugina ML, Toleikis JR . Effects of midazolam on median nerve somatosensory evoked potentials. Br J Anaesth 1990; 64: 590–593.
Lauer K, Munshi C, Larson S . The effect of midazolam on median nerve somatosensory evoked potentials. J Clin Monit 1994; 10: 181–184.
Loughnan BL et al. Evoked potentials following diazepam or fentanyl. Anaesthesia 1987; 42: 195–198.
Lubicky JP et al. Variability of somatosensory cortical evoked potential monitoring during spinal surgery. Spine 1989; 14: 790–798.
Albanese SA, Spadaro JA, Lubicky JP, Henderson NA . Somatosensory cortical evoked potential changes after deformity correction. Spine 1991; 16(8 Suppl): 371–374.
Kalkman CJ, ten Brink SA, Been HD, Bovill JG . Variability of somatosensory cortical evoked potentials during spinal surgery. Effects of anesthetic technique and high-pass digital filtering. Spine 1991; 16: 924–929.
Adams HP, Kunz S . Inter- and intraindividual variability of posterior tibial nerve somatosensory evoked potentials in comatose patients. J Clin Neurophysiol 1996; 13: 84–92.
Connemann BJ, Koehler J, Presser S, Hopf HC . Latency and amplitude variability in serial median nerve SEP recordings. Clin Neurophysiol 1999; 110: 1664–1668.
York DH, Chabot RJ, Gaines RW . Response variability of somatosensory evoked potentials during scoliosis surgery. Spine 1987; 12: 864–876.
Luk KD, Hu Y, Wong YW, Leong JC . Variability of somatosensory-evoked potentials in different stages of scoliosis surgery. Spine 1999; 24: 1799–1804.
Rappaport M et al. Effects of corrective scoliosis surgery on somatosensory evoked potentials. Spine 1982; 7: 404–406.
Acknowledgements
We are grateful to B Gyr for technical assistance and Th Erni for statistical advice. The study was financially supported by the Swiss National Foundation (3152-062025.00).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Strahm, C., Min, K., Boos, N. et al. Reliability of perioperative SSEP recordings in spine surgery. Spinal Cord 41, 483–489 (2003). https://doi.org/10.1038/sj.sc.3101493
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101493
Keywords
This article is cited by
-
Could extended laminectomy effectively prevent spinal cord injury due to spinal shortening after 3-column osteotomy?
BMC Musculoskeletal Disorders (2023)
-
Value of multi-channel somatosensory evoked potentials recording in patients undergoing scoliosis correction surgery
European Spine Journal (2023)
-
Relationship between the laminectomy extension and spinal cord injury caused by acute spinal shortening: goat in vivo experiment
European Spine Journal (2020)
-
Influence of vertebral column distraction on spinal cord volume: an experimental study in a goat model
Archives of Orthopaedic and Trauma Surgery (2015)
-
The causes and treatment strategies for the postoperative complications of occipitocervical fusion: a 316 cases retrospective analysis
European Spine Journal (2014)