Abstract
Study design: Report of an epidermoid cyst with intramedullary localization.
Objective: To describe an atypical presentation of intramedullary epidermoid cyst.
Summary of background data: Intramedullary epidermoid cysts are rare entities with a marked variability in the clinical presentation, essentially of neurological pertinence.
Methods: Case report of a spinal epidermoid cyst in a 13-year-old girl presenting with urological symptoms: she had a 12-month history of recurrent low urinary tract infections, urinary frequency and nocturnal enuresis. A urodynamic evaluation was performed and showed the presence of involuntary bladder contractions with detrusor instability and low bladder compliance. Magnetic resonance imaging of the spine demonstrated an intramedullary lesion of the dorsal spinal cord.
Results: The mass was excised and 6 months after surgical excision, urological manifestations improved with decreased detrusor hyper-reflexia, increased bladder capacity and compliance and no later report of urinary tract infections.
Conclusions: In our patient, unusual clinical manifestations of the tumor have delayed the diagnosis, but its complete removal has led to remission of symptoms. Detailed neurological examination and investigations are indicated in patients with clinical and urodynamic features, suggestive of neuropathic bladder.
Similar content being viewed by others
Introduction
Epidermoid cyst in the spinal cord is a rare condition, constituting only 0.6–1.1% of all spinal tumors.1 The majority of spinal epidermoid cysts are subdural and extramedullary, while intramedullary localization is very rare.
Intramedullary epidermoid cyst is common in lumbosacral and thoracic regions; two frequent localizations are T4–T6 and T11–T12, while only three cases have been reported with cervical cord involvement.2,3,4
The symptoms at presentation of epidermoid cysts in the lower thoracic and upper lumbar regions are usually neurologic, such as progressive paraparesis and motor–sensory complaints; sphincter troubles may occur later.1,2,3,4,5
We report a case of a 13-year-old patient with an intramedullary epidermoid cyst presenting with urological manifestations.
Case report
This 13-year-old girl was referred to our hospital with a 12-month history of recurrent low urinary tract infections (UTI), urinary frequency and nocturnal enuresis.
The first diagnostic evaluation had included renal ultrasonography and voiding cystouretrography that were normal. In addition, urological studies had been completed with cystometrography in order to evaluate compliance, involuntary detrusor contractions, bladder volume and desire to void. Urodynamic findings had shown detrusor instability, defined as presence of uninhibited contractions of the bladder muscle at pressure more than 15 cm/H2O, occurring during the filling phase of the cystometric curve, with worsening bladder compliance. Urological symptoms persisted despite antibiotic and anticholinergic treatment with oxybutynin chloride (0.1 mg/kg/die).
At the admission to Department of Pediatrics of our Hospital, the neurological examination of the patient was normal without any cutaneous spine lesion. Moreover, she had no prior history of lumbar punctures.
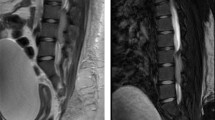
Although neurological examination was remarkably negative and no cutaneous stigmata were present at physical examination, as a consequence of the recent onset of urinary symptoms without history of congenital malformation or traumatic lesions, the patient underwent a magnetic resonance imaging (MRI) of the spine, mainly to rule out any ‘occult’ spinal dysraphism, such as ‘tight’ filum terminale, etc. Surprisingly, MRI revealed an intramedullary lesion of the dorsal spinal cord that extended from T10 to T11 vertebral body (Figure 1). The lesion was hypointense in the T1-weighted images and hyperintense in the T2-weighted ones, suggesting an epidermoid cyst. On these grounds, a laminotomy was performed at T10–T12 levels. After dural opening, the lower tract of the spinal cord and the conus medullaris appeared overdistended by an intrinsic lesion. By performing a limited dorsal split, the whitish tumor capsule was immediately reached. The capsule was dissected free from the neural tissue and then opened to allow partial removal of the soft, pearly content. Thereafter, a progressive careful dissection of the cyst wall was accomplished until its complete removal. Macroscopically, a well-demarcated and unilocular soft cyst, filled with friable contents, was observed. Histological examination confirmed an epidermoid cyst (Figure 2).
Postoperative course was uneventful, without any neurological deterioration. Postoperative MRI taken approximately 2 months after surgery confirmed total tumor removal (Figure 3). At 6 months after the operation, urodynamic findings and urological manifestations improved significantly with decreased detrusor bladder contractions and increased bladder capacity and compliance as showed in Figures 4 and 5, without occurrence of UTI.
No significant modification of bowel movements, characterized by mild constipation, was appreciated before and after surgery.
Discussion
Epidermoid tumors rarely occur in the central nervous system and are even rarer in the spinal canal.1,6
The pathogenesis of spinal epidermoid cysts is mainly congenital, as they take origin from the epithelial tissue displaced during the closure of the neural tube between the 3rd and 5th weeks of gestation.7 There is the possibility of acquired forms resulting from iatrogenic penetration of skin fragments after single or multiple lumbar spinal punctures8,9,10 or after meningomyelocele repair.11,12 However, also under these circumstances, it is questionable whether a congenital origin can be excluded. The congenital epidermoid cysts are most frequently associated with other congenital abnormalities, such as dermal sinus, spina bifida and hemivertebrae.
The slow growth of epidermoid cysts often leads to a delay in their diagnosis: duration of symptoms before diagnostic recognition may extend for many years.5
Signs and symptoms at presentation are usually neurological, such as progressive paraparesis, sensory loss and back/leg pain that can be variably intermingled according to the specific tumor localization.2,4,5,13 Urological manifestations are observed as an expression of the interference of the mass with different mechanisms responsible for voiding. Normal voiding relies on a complex neurophysiological system between the cerebral cortex and the sacral spinal cord. Any lesion in this area results in neurourological changes, which are clearly understood in the case of spinal cord lesions.10,14,15,16
The peculiarity of our patient's history is that she had urological symptoms as initial manifestations, consisting mainly of urge incontinence combined with recurrent UTI, leading to a 1-year diagnostic delay. The absence of neurological deficits is also remarkable.
In the last decade, MRI has undoubtedly revolutionized the diagnosis of intramedullary tumors, reducing the interval between onset of symptoms and diagnosis. Epidermoids are usually slightly hyperintense as opposed to cerebrospinal fluid, and their lobulated aspect helps differentiating these lesions from arachnoid cysts. On the contrary, dermoid cysts show variable signal intensity. This disparity in signal intensity most likely reflects variable lipid and protein composition in the lesions. Other features include absence of edema in the surrounding tissues, well-defined limits and presence of calcifications. An intravenous injection of gadolinium may also demonstrate a peripheral enhancement.17,18
In our case, MRI showed the typical pattern of epidermoid cysts, that is, a well-circumscribed mass, hypointense on T1-weighted and hyperintense on T2-weighted images.
Diagnosis of epidermoid as well as dermoid cysts is usually based on inspection due to typical aspect of their content. Histologically, epidermoid and dermoid cysts are lined by stratified squamous epithelium supported by an outer layer of collagenous tissue; progressive desquamation of keratin from epithelial lining toward the interior of the cyst produces a soft white material.6 Differentiation between the two forms is based on the presence of skin adnexa present only in dermoid cysts.
The treatment of an intramedullary epidermoid cyst is surgical. Emptying of the cyst material is normally performed without difficulty, but the thin tumor capsule is usually tightly adherent to the surrounding neural tissue and its complete removal can cause neurological deficits; so when the cyst wall is intimately attached to the spinal cord, it should be left in place.2 In our case, microsurgical dissection of the cyst wall enabled us to achieve total capsule removal without producing any neurological deterioration.
Conclusions
Epidermoid cysts are rare tumors without specific clinical presentation. In our patient, atypical clinical manifestations delayed the diagnosis, although removal of the tumor resulted not only in cessation of clinical progression but even in the remission of symptoms. Detailed neurological examination and investigations are indicated in patients with clinical and urodynamic features suggestive of neuropathic bladder when urological symptoms are present, such as UTI, urinary frequency and nocturnal enuresis, especially if unresponsive for long times to conventional therapy.
References
Lunardi P et al. Long term results of the surgical treatment of the spinal dermoid and epidermoid tumors. Neurosurgery 1989; 25: 860–864.
Tekkok IH et al. Intramedullary epidermoid cyst of the spinal cord associated with an extraspinal neuroenteric cyst: case report. Neurosurgery 1992; 31: 121–125.
Zavanone M et al. A cervico-dorsal intramedullary epidermoid cyst: case report and review of literature. J Neurosurg Sci 1991; 35: 111–115.
Jadhav RN, Khan GM, Orth D, Palande DA . Intramedullary epidermoid cyst in cercicodorsal spinal cord. J Neurosurg 1999; 90: 161.
Roux A et al. Intramedullary epidermoid cyst of the spinal cord. J Neurosurg 1992; 76: 528–533.
Guidetti B, Gagliardi FM . Epidermoid and dermoid cysts. Clinical evaluation and late surgical results. J Neurosurgery 1977; 47: 12–18.
Russel DS, Rubinstein LJ . Pathology of Tumors of the Nervous System. Vol. 99, 5th edn. Wiliams and Wiliams: Baltimore, 1989. pp 693–695.
Halcrow SJ, Crawford PJ, Craft AW . Epidermoid spinal cord after lumbar puncture. Arch Dis Child 1985; 60: 978–997.
Shaywitz BA . Epidermoid spinal cord tumors and previous lumbar punctures. J Pediatr 1972; 80: 638–640.
Potgieter S et al. Epidermoid tumours associated with lumbar punctures performed in early neonatal life. Dev Med Child Neurol 1998; 40: 266–269.
Kirsch WM, Hodges III FJ . An intramedullary epidermoid inclusion cyst of the thoracic cord associated with a previously repaired meningocele. Case report. J Neurosurg 1996; 24: 1018–1020.
Song JM, Kim MH, Shin KM . Intraspinal epidermoid cyst occurring 15 years after lipomyelomeningocele repair. J Neurosurg 1999; 90: 252–254.
Elazhari A et al. Kyste épidermoide médukkaire dorsal. A propos d'un cas avec IRM at revue de la littèreture. Neurochirurgie 1996; 42: 309–311.
Gallina P et al. Un cas rare de kiste épidermoide intramédullaire observé a l'IRM. Neurochirurgie 1992; 38: 372–375.
Kaplan SA, Chancellor MB, Blaivas JG . Bladder and sphyncter behavior in patients with spinal cord lesions. J Urol 1991; 146: 113.
Fone PD et al. Urodynamic findings in the tethered spinal cord syndrome: does surgical release improve bladder function?. J Urol 1997; 157: 604–609.
Vion-Dury J et al. Magnetic resonance imaging of epidermoid cysts. Neuroradiology 1987; 29: 333–338.
Phillips J, Chiu L . Magnetic resonance imaging of intraspinal epidermois cyst: a case report. J Comput Assist Tomogr 1987; 11: 181–183.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ferrara, P., Costa, S., Rigante, D. et al. Intramedullary epidermoid cyst presenting with abnormal urological manifestations. Spinal Cord 41, 645–648 (2003). https://doi.org/10.1038/sj.sc.3101482
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101482
Keywords
This article is cited by
-
Thoracic intramedullary epidermoid cyst-timely fashion diagnosis and treatment
Child's Nervous System (2015)
-
Bildgebung bei demyelinisierenden und tumorösen Erkrankungen des Rückenmarks
Der Radiologe (2010)