Abstract
Study design: Retrospective descriptive study.
Objectives: To assess incidence, causes and early outcome of traumatic spinal cord injury (SCI) among children in Sweden, thereby identifying high-risk groups and situations as a basis for preventative measures and improved care.
Methods: Data from population registers, County Habilitation Centers as well as from informal sources were used to estimate the incidence of SCI in Sweden during the years 1985–1996 among children aged 0–15 years. Contacts with the treating hospitals, reviews of medical records and/or personal interviews were used to verify primary data. In total, 92 children were thus identified.
Results: The incidence was found to be 4.6/million children/year (95% CI 3.6–5.5). When excluding prehospital fatalities, the incidence was 2.4 (95% CI 1.8–3.1). The main cause of injury among fatalities was traffic accidents. Associated injuries occurred in 41% of the children. Among survivors (10–15 years), sports-related injuries (43%) were as common a cause as traffic accidents (39%). The survivors were treated in 18 different hospitals.
Conclusion: Pediatric SCI in Sweden is rare, presumably because of effective primary prevention. Preventative measures should be further differentiated for each age group of children in accordance with their differing risk profiles. In contrast to the effective preventative measures that have been implemented in Sweden, care of these patients is still too fractionated and decentralized for sufficient specialization to emerge.
Similar content being viewed by others
Introduction
Since spinal cord injury (SCI) predominately occurs in younger adults, it is not surprising that most research has focused on such populations, while other demographic groups have received less attention.1
During the last decade, especially in the USA, childhood SCI have received increasing coverage in the literature. This subgroup has special needs because of the ongoing physical, intellectual, psychological and social development that characterizes the child and teenager.2,3
Knowledge of the incidence and etiology of pediatric SCI is important in order to identify risk groups, improve prevention and for planning of care and rehabilitation.4
Specifically, the development of the Model Spinal Cord Injury Programs, in addition to systematic trauma registration in the National SCI Database, have contributed to increased knowledge of pediatric SCI.5
However, this database is not population based and does not include persons treated outside the Model Systems.5 Furthermore, children with SCI, especially the youngest, typically receive treatment at children's hospitals rather than at spinal units (personal communication, 24 January 2001).6
Incidence estimates of pediatric SCI are often uncertain because of differing reporting methods, data collection systems and classification patterns.7 Hospital-based clinical series are biased by referral patterns and obviously only include patients admitted to a hospital. SCI patients who die at the scene or are dead on arrival are usually not reported. Clinical series rarely include detailed data from post mortems, the coroner- and birth-related SCI. Thus, incidence estimates often appear to be too low.7 Furthermore, it is difficult to make analyses to identify statistically significant patterns because of small study groups.1
In Sweden, the estimated total incidence of SCI in all age groups is 15/million/year.8 This is a low incidence as compared to the USA, where incidence rates among adults range from 28 to 54.8/million/year.9
Since 1994, a collaboration group representing all university hospitals in Sweden have developed a matrix for documentation and quality assessment of SCI care.8 In 1998, 106 cases of traumatic SCI were thus documented, equaling an incidence of traumatic SCI of 12/million/year. The group also reported that about 20% of all cases were in fact treated outside university hospitals, thus making the documented incidence too low. Four children under the age of 16 years with SCI were reported in 1998 and one child in 1999 (personal communication, February 1999).10
This was the only information to be found about pediatric SCI in Sweden.
The objectives for this study were to assess the incidence, etiology and early outcome of pediatric SCI in Sweden during 1985–1996 in order to identify high-risk groups and situations as a knowledge basis for preventative measures and improved care.
Methods
The incidence estimates of pediatric SCI were calculated on data from population registers and County Habilitation centers for the years 1 January 1985 to 31 December 1996.11
The total population of Swedish children below 16 years of age during the 12 year period was 20 171 823 children, with an average population of 1 680 000 children/year (max/min: 1 767 000/1 613 000).12
Instead of using the total population to estimate the incidence for the total period, it is better to use the information from each year. The incidence for every year can be treated as a random variable over the 12-year period. The expected value and the confidence interval were then based on the incidence from each year.
The pediatric SCI population was assessed according to the following variables: gender, age at injury, cause of injury13,14 and cause of death.15,16 The level of injury and functional outcome according to ASIA/IMSOP standards17 was documented among the survivors by personal contact and medical records between 1999 and 2002.
Definition
In this study, SCI was operationally defined as traumatic lesions of the cauda equina or the spinal cord proper leading to neurological impairment. Lesions with complete sensorimotor restitution were also included, as defined by ASIA Impairment Scale grade E,17 if there was documented evidence of symptoms and signs of SCI with a duration of at least 2 weeks postinjury.18
Sources
Three types of sources were used:
-
1)
Nationwide population-based registers admitted by the Swedish National Board of Health and Welfare, that is,
-
Hospital Discharge Register (HDR),
-
Cause of Death Register (CDR),
-
Medical Birth and Malformation Register (MBR).
-
-
2)
Regional or local registers, that is,
-
County Habilitation Centers in Sweden.
-
-
3)
Media/informal sources, that is,
-
Notification in patient-orientated journals and informal contacts with staff working with SCI patients.
-
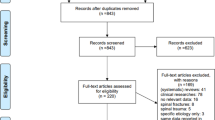
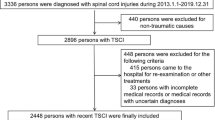
Inclusion criteria and exclusion criteria (Table 1)
The procedure of finding the children and the verification of the diagnosis is fully described in our paper Pediatric Spinal Cord Injury in Sweden. How to identify a cohort of rare events.11
Mortality
Mortality directly related to the SCI was operationally defined as all deaths that occurred within 1 year postinjury.
Subjects that died later than 1 year postinjury were allocated to the survivor group. (In the current study, this occurred in two children who died 3 and 9 years postinjury, respectively.)
Data verification
-
For children dead prior to hospital admission (N=43), data from the Cause of Death Register15,16 were used as verification. Autopsy protocols were not reviewed.
-
For children dead (N=12) within 1 year postinjury, the head of the department at the treating hospital verified the diagnosis by reviewing the medical records. The information originated from the Hospital Discharge Register19 and the Cause of Death Register.15,16
-
For survivors (N=37), retrieved data were checked against the medical records, by requesting such verification from a senior staff physician at the treating hospital. Subjects were then contacted by telephone for further verification of diagnosis, and remaining putative true cases were then subsequently interviewed and examined for final verification and additional data retrieval. The information originated from the Hospital Discharge Register (N=34),19 Habilitation centers (N=2) and informal contacts (N=1).
Etiological classification
Through the interviews, 10 cases classified as fall accidents, and two cases originally classified as traffic accidents were reclassified as sports injuries.
Level of injury
The level of injury was assessed through the registered ICD codes, medical record reviews, interviews and, in some cases, clinical examination.
Functional outcome according to ASIA/MSOP standards
Most assessments were made between the years 1999 and 2002 by personal contact with the survivors. For three children, data from medical records were used to assess their functional outcome.
Care provider
The survivors were treated at county hospitals, university clinics and/or university clinics with specialized SCI units. The sources utilized were data from the Hospital Discharge Register, medical records and the patients. If a child was treated in two or more hospitals, the hospital where the child had been treated the longest period was chosen.
Ethical considerations
The Ethics Committee at Umeå University agreed to the project (permit no. Um dnr 96-289). Permission was also received from the Swedish Data Inspection Board.
Results
Incidence for ages 0–15 years
The estimated incidence was found to be 4.6/million children/year (95% CI 3.6–5.5) for children aged 0–15 years. If prehospital fatalities were excluded, the incidence was 2.4 (95% CI 1.8–3.1).
In all, 21 children (23%) of the total group (N=92) were aged 15 years at the time of the injury.
Out of the survivors (N=37), 12 children were 15 years of age (32%). Out of the children dead prior of hospital admission (N=43), seven children were aged 15 years (16%). Two children out of the group who died within 1 year postinjury were aged 15 years.
Mortality
In all, 55 children (60%) of the total group (N=92) died within 1 year after the SCI.
Deaths prior to hospital admission
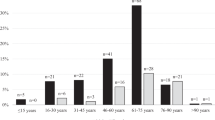
In all, 42 of the 43 children died at the scene of the accident or on the way to hospital were injured in traffic accidents. As main diagnosis three had SCIWORA (ICD 952), and the others were registered as SCI (806.00). Average age at injury was 9 years (SD=4; range 2–15 years), 19 were girls and 23 were boys (Figure 1 and 3).
The retrieved register information gave no information about the level of injury.
Deaths within 1 year postinjury
In total, 12 children died during initial hospitalization; all within 3 months postinjury. All, but one child, were injured by traffic (Figure 1). The average age at injury for this group was 7.3 years (SD=5.3; range 0–15 years), 10 girls and two boys. All had cervical injuries except one child that suffered a thoracic injury, with an additional brain injury (Figure 1 and 3).
The survivors
Children surviving at least the first year postinjury (N=37) had an average age at injury of 11.8 years (SD 4.4; range 2–15 years) (Figure 1).
Associated injuries
Of the total group (N=92), 38 children (41%) had associated injuries, for example, multiple fractures and/or thoracic injuries and/or abdominal injuries and/or head injuries (Table 2). All head injuries but one were caused by traffic.
Causes of injury
Among fatalities, traffic accidents dominated. In the group of survivors (10–15 years), sports injuries were as common as traffic accident (Figure 1).
Traffic accidents
None of the bicyclists survived. The mean age was 9.2 years (SD 3.6; range 4–15). The pedestrians had a mean age of 8.9 years (SD 2.8; range 5–14) (Figure 2; Table 3).
Sports-related injuries
The second leading cause of injury was sports-related injuries. All cases were aged between 13 and 15 years. The causes were: motor-cross/bicycle (competition) N=2, horseback riding N=3, icehockey N=2, diving N=3 and skiing N=2.
Four out of 12 children were females, injured during horseback riding (N=3) and skiing (N=1).
Falls
Out of six injures among the survivors, four children were injured by falling from heights. Only one girl was injured in a falling accident (Figure 1).
Iatrogenic injury
Three children, two girls and one boy, sustained an SCI at surgery for spinal deformity (Figure 1).
Sciwora
Of the total group (N=92), five children were registered as SCIWORA. Among the fully verified survivors, three children had sustained a SCIWORA (aged 3, 4, 9 years).
Gender
There were 47 male and 45 female subjects. The distribution of male subjects increased by age among the survivors (Figure 3).
Types of lesions
Cervical injuries among the survivors were as common as thoracic lesions (N=16). The average age for children with cervical lesions was 12.2 years (SD 4.2; range 3–15 years), for children with thoracic lesions 11.1 years (SD 4.8; range 2–15 years) and for children with lumbar lesions 13.2 years (SD 1.3; range 11–15 years) (Figure 4).
Almost half (N=17) of the group of survivors had a complete SCI (ASIA grade A) (Figure 4, Table 4).
Care provider
The survivors (N=37) were treated in 18 different hospitals.
The average age of children treated at an SCI unit was 14 years (SD 1.3; range 9–15 years), whereas children treated at another ward at a university hospital or at a county hospital had a lower average age, 8 and 8.9 years, respectively (Table 5).
Discussion
Pediatric SCI is rare in Sweden; although this is in accordance with clinical experience, the actual incidence has not been previously established. The incidence is lower than those reported from the USA and New Zealand, except from the article by Woodruff, 199420,21,22,23,24,25,26,27,28,29,30,31,32 (Table 6).
However, there are differences in case definition, case ascertainment and upper age limit making comparisons of incidence and external causes problematic.28,30
The New Zealand study by Dixon31 has been criticized while the data were based on ICD codes and was not further verified, possibly leading to inclusion of false positives.32
Inclusion of patients aged 15 and older will inflate the incidence rate for the pediatric group, since the incidence peak for all SCIs is 15–24 years.24,27
The incidence found in this study may be underestimated because of omission of the SCI diagnosis in cases of severe fatal multitrauma, as discussed by Dickman.7
The mortality was high (60%). Kewalramani also found high mortality (58%) because of the commonly severe, multiple injuries sustained in traffic accidents.30 Orenstein et al33 reported that the high mortality in younger patients was not only caused exclusively by the preponderance of more rostral cervical injury levels, but also, and more importantly, because of concomitant head and multiple trauma.33 In the present study, associated injuries occurred frequently among children who died prior to hospital admission.
The external causes found in this study were largely in accordance with those found in earlier reports1,34,35,36,37 except from violence9,38,39 and perinatal injury,40,41,42 which did not occur in the present study.
Traffic was the main cause of injury among Swedish children. Further studies are needed in order to assess whether the children were properly restrained and if the injuries could have been prevented. The current study showed an increased mortality in children aged 5–9 years. This may be a result of insufficient parental supervision in the traffic environment and also increasing objection among children as regards the use of restraints in cars. All injured bicyclists in the group died. Further studies are warranted to ascertain as to when children are mature enough to ride a bicycle in the traffic environment. Only two children, out of the eight children injured in a bicycle accident, were older than 11 years.
Sport was the second leading cause of injury among the surviving teenagers, this in accordance with earlier reports.1,34,35,36,37
All sport-related injuries, but two, (a bicyclist and a motor-cross accident during competition), were registered as falls. Through interviews with the survivors these errors in classification could be corrected. Among the deceased this was not possible, and either of the two deaths registered as an injury because of fall could have been sports related. There are difficulties comparing the causes of SCI reported in published studies, since there is no detailed standard for categorization. Causes of injury can often fit into several etiological groups26 and the ICD codes for external causes do not include sports-related injuries as a discrete category.13,14 The distribution of gender did not differ from previous reports. With increasing age, males have higher SCI morbidity.43
The current study could not confirm among the survivors, the previously documented tendency for children to sustain upper cervical level injuries.7,33,44 On the other hand, there was no information about the level of injury among the children who died prior to hospital admission.
The assessment of functional outcome among survivors was in accordance with the findings of DeVivo, et al.35
For pediatric SCI, the additional problems related to ongoing physical and emotional growth are superimposed on the generic consequences of such an injury. This may create quality problems of care when the incidence is low and the children are treated at many different hospitals.
Traffic accident was the main cause of injury. Prevention of pediatric SCI is part of the overall prevention of accidents in children and adolescents. The incidence of accidents among Swedish children is among the lowest in the world. This is likely a result of vigorous preventative work performed for over 50 years. Laws and regulations have made the environment for the child safer, in addition to information and education of the parents.45
The low incidence of pediatric SCI together with the overall low incidence of SCI in Sweden further support that prevention in traffic can be effective.
Still, accidents are the most common cause of death in Sweden among children and adolescents aged 1–14 years.45
Children are vulnerable in traffic when complex situations exceed their cognitive, developmental, behavioral, physical and sensory abilities. Children are impulsive and have difficulty judging speed, spatial relations, distance and velocity. These abilities develop gradually and individually. The teenagers tend to take more risks as they are influenced by their emotions, stress and peer pressure.46 They move more frequently in the adult environment, but they lack the experience and mature behavior of an adult.
As sport was the second leading cause of injury among the teenagers, preventative measures, especially information of safer sports rules and equipment in schools and for sport organizations, must be undertaken in sports carrying a risk for SCI.
Consequently, SCI prevention must be tailored according to the specific risk profile of each age group.
Conclusions
Pediatric SCI in Sweden is rare, presumably because of effective primary prevention. Preventative measures should be further differentiated for each age group of children in accordance with their differing risk profiles. In contrast to the effective preventative measures that have been implemented in Sweden, care of these patients is still too fractionated and decentralized for sufficient specialization to emerge.
References
Apple D, Anson C, Hunter J, Bell R . Spinal cord injury in youth. Clin Pediatr 1995; 34: 90–95.
Betz R, Vogel L . Introduction to the child with a spinal cord injury. In: Betz R. Mulcahey M (eds). The Child with a Spinal Cord Injury. American Academy of Orthopaedic Surgeons: Rosemont, IL 1996, XXI–XXIV.
Flett PJ . The rehabilitation of children with spinal cord injury. J Paediatr Child Health 1992; 28: 141–146.
Vogel L, DeVivo MJ . Etiology and demographics. In: Betz R, Mulcahey M (eds). The Child with a Spinal Cord Injury. American Academy of Orthopaedic Surgeons: Rosemont, IL 1996, pp 3–12.
Stover S, DeVivo M, Go B . History, implementation, and current status of the national spinal cord injury database. Arch Phys Med Rehabil 1999; 80: 1365–1371.
DeVivo MJ . Incidence of Pediatric spinal cord injury. National Spinal Cord Injury Statistical Center: Birmingham, Alabama 2001.
Dickman CA, Rekate HL, Sonntag VKH, Zambramski JM . Pediatric spinal trauma: vertebral column and spinal cord injuries in children. Pediatr Neurosci 1989; 15: 237–256.
Levi R, Ertzgaard P . Quality indicators in spinal cord injury care: a Swedish Collaborative Project. Scand J Rehabil Med Suppl 1998; 38: 1–80.
Carroll C . Spinal cord injuries in Arkansas due to violence: 1980–1989. Spinal Cord 1997; 335: 341–348.
Stålhammar D . Administrator for the SCI Register in Sweden. Sahlgrenska University Hospital: Göteborg 1999.
Augutis M, Malker H, Levi R . Pediatric spinal cord injury in Sweden. How to identify a cohort of rare events. Spinal Cord 2003; 41: 337–346.
SCB. Population Statistics. Part III, Distribution by Sex, Age Marital Status and Citizenship by Municipality etc. Statistics Sweden: Stockholm 1985–1996.
Welfare S-TSNBoHa. Klassifikation av sjukdomar, systematisk förteckning (International Classification of Diseases, Ninth Revision ICD-9), Swedish version. 1:a edn. Socialstyrelsen: Stockholm 1987.
Welfare S-TSNBoHa. Klassifikation av sjukdomar mm systematisk förteckning. 4:e edn. Socialstyrelsen: Stockholm 1968.
Statistics NBo. Causes of death 1995. Official Statistics of Sweden. Statistics Sweden: Stockholm 1995.
Statistics NCBo. Cause of Death 1983. Statistics Sweden: Stockholm 1985.
Ditunno J, Young W, Donovan W, Creasey G . The International Standards Booklet for neurological and functional classification of spinal cord injury. Paraplegia 1994; 32: 70–80.
Levi R . The Stockholm spinal cord injury study: medical, economical and psycho-social outcomes in a prevalence population [Doctoral dissertation]. Karolinska, Institute: Stockholm 1996.
Statistics NCBo. In-patient Statistics 1981 in Somatic Hospitals. Statistics Sweden: Stockholm 1984.
Surkin J et al. Spinal cord in Mississippi, findings and evaluation, 1992–1994 . Spine 2000; 25: 716–721.
Buechner J, Speare M, Fontes J . Hospitalizations for spinal cord injuries, 1994–1998. Med Health Res Inst 2000; 83: 92–93.
Martins F et al. Spinal cord injuries – epidemiology in Portugal's central region. Spinal Cord 1998; 36: 574–578.
Warren S, Moore M, Johnson MS . Traumatic head and spinal cord injuries in Alaska (1991–1993). Alaska Med 1995; 37: 11–19.
Thurman D et al. Surveillance of spinal cord injuries in Utah, USA. Paraplegia 1994; 32: 665–669.
Thurman D . Incidence pediatric spinal cord injury 1989–1991 Utah, USA. National Center for Chronic Disease Prevention and Health Promotion: Atlanta, GA, USA 2001.
Price C, Makintubee S, Herdon W, Istre G . Epidemiology of traumatic spinal cord injury and acute hospitalization and rehabilitation charges for spinal cord injuries in Oklahoma, 1988–1990. Am J Epidemiol 1994; 139: 37–47.
Woodruff BA, Baron RC . A description of nonfatal spinal cord injury using a hospital-based registry. Am J Prev Med 1994; 10: 10–14.
Acton P et al. Traumatic spinal cord injury in Arkansas 1980–1989. Arch Phys Med Rehabil 1993; 74: 1035–1040.
Farley T . Incidence of Pediatric Spinal Cord Injury in Arkansas 1980–1989. Arkansas Spinal Cord Comission Little Rock: Little Rock AR, USA 2002.
Kewalramani LS, Kraus JF, Sterling HM . Acute spinal-cord lesions in a pediatric population: epidemiological and clinical features. Paraplegia 1980; 18: 206–219.
Dixon G, Danesh J, Caradoc-Davies T . Epidemiology of spinal cord injury in New Zealand. Neuroepidemiology 1993; 12: 88–95.
van Asbeck F, Post M, Pangalila R . An epidemiological description of spinal cord injuries in The Netherlands in 1994. Spinal Cord 2000; 7: 420–424.
Orenstein J et al. Age and outcome in pediatric cervical spine injury: 11-year experience. Ped Emerg Care 1994; 10: 132–137.
Hamilton M . Pediatric spinal injury: review of 174 hospital admissions. J Neurosurg 1992; 77: 700–704.
DeVivo M et al. The Influence of age at time of spinal cord injury on rehabilitation outcome. Arch Neurol 1990; 47: 687–691.
Kewalramani LS, Orth MS, Tori J . Spinal trauma in Children. Spine 1980; 5: 11–18.
Stover LS DJ, Whiteneck GG . Spinal Cord Injury Clinical Outcomes from the Model System. 1st edn. Aspen Publisher Inc: Gaithersburg, MD 1995.
Montes L . Firearm Injuries in the child: Demographics, Management and prevention. In: Betz R, Mulcahey M (eds). The Child with a Spinal Cord Injury. American Academy of Orthopaedic Surgeons: Rosemont, IL 1996, pp 179–185.
Vogel L, DeVivo M . Etiology. In: Betz R, Mulcahey M (ed). The Child with a Spinal Cord Injury. American Academy of Orthopaedic Surgeons: Rosemont, IL 1996, pp 888.
Medlock MD, Hanigan WC . Neurological birth trauma. Clin Perinatol 1997; 24: 845–857.
Perlman M . Neonatal spinal cord injury in the infant: etiology, diagnosis, treatment and outcome. In: Betz R, Mulcahey M (eds). The Child with a Spinal Cord Injury. American Academy of Orthopaedic Surgeons: Rosemont, IL 1996; pp 161–167.
Koch B, Eng G . Neonatal spinal cord injury. Arch Phys Med Rehabil 1979; 60: 378–381.
Vogel L . Unique management needs of pediatric spinal cord injury patients: etiology and pathophysiology. J Spinal Cord Med 1997; 20: 10–13.
Pang D . Spinal Cord injury without radiographic abnormality (SCIWORA). In: Betz R, Mulcahey M (eds). The Child with a Spinal Cord Injury. American Academy of Orthopaedic Surgeons: Rosemont, IL 1996, p 139–160.
Berfenstam R . Barnolycksfall. The Swedish Council on Technology Assessment in Health Care: Stockholm 1997. Report No.: 132.
Administration UDoTNHTS. Traffic Safety Facts 1999. NHTSA www.nhtsa.dot.gov, 1999.
Acknowledgements
This work was supported by a grant from Cancer och Trafikskadades Riksförbund, Permobil and the Mid Sweden Research and Development Center, Vasternorrland County Council, Sweden.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Augutis, M., Levi, R. Pediatric spinal cord injury in Sweden: incidence, etiology and outcome. Spinal Cord 41, 328–336 (2003). https://doi.org/10.1038/sj.sc.3101478
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101478
Keywords
This article is cited by
-
A systematic review and meta-analysis of the global epidemiology of pediatric traumatic spinal cord injuries
European Journal of Pediatrics (2023)
-
Temporal changes in demographic and injury characteristics of traumatic spinal cord injuries in Nordic countries - a systematic review with meta-analysis
Spinal Cord (2022)
-
Global mapping for the epidemiology of paediatric spinal cord damage: towards a living data repository
Spinal Cord (2019)
-
Risk factors in iatrogenic spinal cord injury
Spinal Cord (2017)
-
Coping strategies recalled by young adults who sustained a spinal cord injury during adolescence
Spinal Cord (2012)