Abstract
Study design: Case report of a rare form of hypertrophy of the thoracic posterior longitudinal ligament (HPLL), causing paraparesis.
Objective: To describe this very rare pathological condition in the thoracic spine and the results of surgical intervention.
Setting: A department of orthopaedic surgery in Japan.
Methods: A 61-year-old man presented with acute paraparesis associated with HPLL in the thoracic region. A radiographic and pathological review of the case was conducted. Anterior decompression was performed, and he was followed for 3 years after the operation.
Results: Pathologic examination of the surgical specimen revealed proliferation of fibrocartilage and calcification. The patient's paraparesis ameliorated after the operation.
Conclusion: For this case of myelopathy due to HPLL in the thoracic spine, urgent decompression gave excellent results. Clinical awareness of HPLL may aid correct diagnosis and prompt therapy.
Similar content being viewed by others
Introduction
Hypertrophy of the posterior longitudinal ligament (HPLL) has been reported as a specific but relatively rare pathological condition of the spinal column. HPLL causes many different symptoms, including back pain,1 radiculopathy,2,3,4 and myelopathy.3,5,6 The myelopathy varies in its severity from subtle motor and sensory changes5 to paraparesis with bladder incontinence and spastic gait.6 It occurs mostly in the cervical spine, and rarely in the thoracic4,5 and lumbar1 spine. In the thoracic spine, only two cases of HPLL have been reported in the Japanese literature, without any available documentation in the English literature. We report a very rare case of sudden-onset thoracic myelopathy due to thoracic HPLL.
Case report
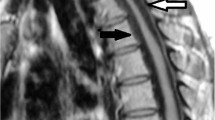
The patient, a 61-year-old man, noticed numbness and motion difficulty in his right foot when he woke up. There was no history of trauma. A neurological examination in the evening of the same day revealed paraparesis, with decreased manual muscle testing in the left extensor hallux longus down to 2/5 and hyperactive deep-tendon reflexes in the lower limbs. Hypesthesia and hypalgesia below the left L1 dermatome and anesthesia and analgesia below the right Th8 dermatome were observed. A Foley catheter was applied because of urinary incontinence. Radiological studies demonstrated thick tissue with isointensity at the Th6–7 disc level, where slight disc protrusion was noted, upon T1-weighted MRI. At the Th6-7 disc level, considerable stenosis of the spinal canal and resultant spinal cord compression were revealed. Although the thick tissue showed similar MRI signal intensity to the intervertebral discs, it was clearly distinguished from them by sagittal MRI scan. Myelography and computed tomography-myelogram of the whole spine revealed that the spinal cord was compressed at only the Th6 to Th7 vertebral levels (Figure 1a,b,c). Having confirmed that this lesion was the cause of the myelopathy, we performed decompressive Th6–7 partial corpectomy via a right antero-lateral thoracotomy and rib grafting without instrumentation.
(a) Sagittal T1-weighted magnetic resonance image showing deformity of the spinal cord due to compression by thick tissue in the spinal canal. The tissue shows isointensity with the intervertebral discs. (b) Axial T1-weighted magnetic resonance image through the Th6–7 disc level. (c) Computed tomography-myelogram through the Th6–7 disc level. A thick soft tissue mass with an extradural complete type of contrast block and slight calcification is shown
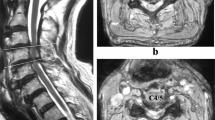
At surgery, after removal of the disc, a hypertrophic deep layer of posterior longitudinal ligament showing no continuity with the disc was observed. This was excised piece by piece until the dural tube appeared to be entirely decompressed. Histological examination of the resected material showed proliferation of fibrocartilage and calcification in some areas, which confirmed the diagnosis of HPLL (Figure 2). No ossification of the ligament was found in any part of the specimen.
After surgery, the patient exhibited neurological improvement. Four weeks later he was able to perform active straight leg raising, and three years later there is no sensory and motor disturbance, while deep-tendon reflexes in the bilateral lower limbs are slightly hyperactive. He is able to walk with a cane and control his urination.
Discussion
Hypertrophy of the posterior longitudinal ligament was first described by Kamikozuru et al. in 1974.7 Since then, more than 50 cases have been reported.1,2,3,4,5,6,7,8,9 Among them, only two involved the thoracic spine,4,5 and one the lumbar spine;1 the majority involved the cervical spine. All of the cases showed chronic progression of the symptoms. Our case was noteworthy for its unusual location and sudden onset of paraparesis, perhaps because of the slight disc protrusion at the same level of the HPLL, although we were unable to find further evidence of this. Some previous reports2,4,5,9 have argued that HPLL is a precursor of ossification of the posterior longitudinal ligament (OPLL), and in fact our surgical specimen and radiographic studies demonstrated slight calcification that might progress to OPLL.10
In this case, disc herniation was considered in the differential diagnosis. Indeed, histologically, it is somewhat difficult to discriminate HPLL from disc herniation on the basis of a specimen obtained by piecemeal resection, as both show fibrocartilage tissue. However, MR imaging showed that the Th6–7 disc was only protruding, not extruding, and no continuity was observed between the disc and the HPLL during the operation, thus confirming the diagnosis of HPLL.
In the surgical treatment of thoracic HPLL, where the anatomical structure is characterized by a kyphotic shape, direct removal of the HPLL via an anterior approach, as described in this report, is recommended to achieve a sufficient decompression effect on the spinal cord.
When a clinician faces this kind of thoracic myelopathy, awareness of HPLL, including its unique clinical symptoms and radiographic findings with conventional MRI scans, may aid correct diagnosis. If the myelopathy is severe enough to manifest motor disturbance, the authors believe surgical treatment with anterior decompression should be performed at an early stage in order to prevent deterioration and obtain neurological improvement.
References
Matsumoto T et al. Lumbar canal stenosis caused by hypertrophy of the posterior longitudinal ligament: case report. Spine 2001; 15: E576–E579.
Hase H et al. Severe cervical myelopathy due to diffuse hypertrophy of the cervical posterior longitudinal ligament. Spine 1992; 17: 1417–1421.
Mizuno J, Nakagawa H & Hashizume Y . Analysis of hypertrophy of the posterior longitudinal ligament of the cervical spine, on the basis of clinical and experimental studies. Neurosurgery 2001; 49(5): 1091–1098.
Toguchi A et al. An operative case of hypertrophy of the posterior longitudinal ligament in thoracic spine. East Jpn J Clin Orthop 1991; 3: 524–528 (in Japanese).
Nakamitsu K et al. Thoracic myelopathy caused by hypertrophy of thoracic posterior longitudinal ligament: A case report. Clin Orthop Surg 1990; 25: 1087–1090 (in Japanese).
Yamazaki A et al. Magnetic resonance imaging and histologic study of hypertrophic cervical posterior longitudinal ligament. Spine 1991; 16: 1262–1266.
Kamikozuru M & Yamaura I . Hypertrophy of the cervical posterior longitudinal ligament (a provisional name) causing myelopathy: A case report. Clin Orthop Surg 1975; 10: 1097 (in Japanese).
Epstein NE . Ossification of the posterior longitudinal ligamentin evolution in 12 patients. Spine 1994; 19: 673–681.
Kondo S et al. Hypertrophy of the posterior longitudinal ligament is a prodromal condition to ossification. Spine 2001; 26: 110–114.
Ono K et al. Pathology of ossification of the posterior longitudinal ligament and ligamentum flavum. Clin Orthop 1999; 359: 18–26.
Acknowledgements
We thank Prof. T Inuzuka of Dept. of Geriatrics and Neurology, Gifu University, and Drs T Nishimoto, T Hiramatsu, and N Suzuki of Yoro Central Hospital.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Nozawa, S., Shimizu, K., Miyamoto, K. et al. Sudden onset of paraparesis caused by hypertrophy of the thoracic posterior longitudinal ligament. Spinal Cord 41, 53–55 (2003). https://doi.org/10.1038/sj.sc.3101396
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101396
Keywords
This article is cited by
-
Hypertrophied posterior longitudinal ligament and ligamentum flavum causing myelopathy: a case report and literature review
Spinal Cord Series and Cases (2023)
-
Hypertrophy of the posterior longitudinal ligament in the thoracic spine
Spinal Cord (2006)