Abstract
Study design: Research was conducted through the use of semi-structured patient interviews. Subjects were recruited through the Saskatchewan branch of the Canadian Paraplegic Association (CPA) and through the clinical practice of the primary investigator. A total of twenty-one patients were interviewed. A qualitative outcome analysis was performed on information collected.
Objectives: Advance directives (or living wills) serve to communicate the wishes of individuals in the event that they should no longer be capable of making those wishes known. This can include directives on issues such as resuscitation status and withdrawal or withholding of care. The goal of this study was to determine the present level of knowledge and interest of spinal cord injured (SCI) patients on the topic of advance directives, and to determine what specific issues they felt need to be addressed in such a document in this population.
Setting: The study was performed in Saskatoon, Saskatchewan, Canada. Although design and analysis were done in a tertiary care centre, the interviews themselves were conducted in the homes of the participants.
Results and conclusion: The results show that spinal cord injured patients have some knowledge of what is involved in the preparation of an advance directive and that they feel these documents are important. A relatively small percentage have completed their own written directives but a large percentage planned to do so after completing this survey. There is some disagreement about when after the injury the topic should first be discussed. Information about medical conditions which are more likely to arise following a SCI should be included in an SCI-specific document. A template for an SCI-specific living will (the SCIAD) is provided.
Similar content being viewed by others
Introduction
Advance directives allow patients to put into writing their wishes regarding future care decisions, should they become incompetent to make those decisions for themselves. Many recent studies have examined topics ranging from the attitudes of physicians and patients towards advance directives1,2,3 to those advocating greater use4 or providing a guide for decision making.5 The University of Toronto Joint Centre for Bioethics website6 allows the user to download and print an outline of an advance directive to help guide the patient in drafting his or her document. However, this outline is quite broad and general, and is designed for members of the general public rather than persons with specific illnesses or conditions who may have particular medical issues which need to be addressed in more depth. The website also provides disease-specific documents for patients with cancer or for those who are HIV-positive.
Several specific patient populations have been examined with regards to their attitudes toward, and use of, advance directives. These have included pulmonary rehabilitation,7,8 renal failure,9,10 palliative care11 and chronic obstructive pulmonary disease12 patients. A recent survey of patients enrolled in a cardiac rehabilitation program concluded that these patients want to learn more about end of life care and need more opportunities to discuss advance care planning.13 A survey of outpatients at a general medicine clinic has been performed to determine their attitudes and understanding regarding the topic.14 Berry and Singer have recently published ‘The cancer specific advance directive’.15 The majority of these studies indicate that patients may not be well informed about the content or importance of advance directives and would be more likely to use them if properly educated. By and large, patients seem to consider it a very important topic that is not always properly addressed by the medical profession.
Martin, Thiel and Singer have also recently published work highlighting the importance of advance directives in the HIV population.16 This qualitative study showed that the primary goal of advance care planning in this population was to prepare for death, which entailed facing death, achieving a sense of control, and strengthening relationships. Although not all of these are applicable to the spinal cord injured (SCI) population, the emphasis on discussion of issues with family members and loved ones is likely to be of importance.
Of specific concern for SCI patients is the recent publication of an editoral in ‘Caliper’, the newsletter for the Canadian Paraplegic Association.17 This article suggests that some patients with spinal cord injuries (and other disabilities) have been given ‘Do not resuscitate’ status without their knowledge or consent, possibly because the physician involved felt that the patient's quality of life was sufficiently low so as to justify not resuscitating them. This serves to further emphasize the importance of providing advance directives in this population in order to make the patient's wishes clearly known.
As Berry15 points out, condition-specific advance directives have several advantages over generic forms: they present patients with clinical scenarios that they are likely to encounter, better prognostic information can be included and possible clinical scenarios and choices are less hypothetical.
A recent study by Prince et al18 demonstrated that patients with spinal cord injuries who feel they have greater control over their day-to-day lives and decisions have a higher self-perceived quality of life. The ability to provide directives on future care issues would certainly enhance this ‘locus of control’. Another study19 found that many factors influenced the quality of life for quadriplegic persons, including the ability to be assertive and to have inner strength, also traits that would be enhanced by the ability to provide advance directives.
Methods
The study consisted of a series of semi-structured interviews examining the knowledge and attitudes of SCI patients towards advance directives. The interview questions were designed based on results of past studies in other patient populations and experience at our Centre with the SCI population (see Appendix 1). Approval for the study was obtained from the University of Saskatchewan Research Ethics Committee.
Patients were accessed through the Saskatchewan branch of the Canadian Paraplegic Association, and through the clinical practice of the primary author. In addition to answering specific questions, participants reviewed a generic living will form available on the website of the University of Toronto Joint Centre for Bioethics6 and were asked to identify specifc parts of the document which would be of concern and relevance to SCI patients. They were also asked to make recommendations with regards to what information should be included in a spinal cord injury-specific advance directive (the SCIAD).
Twenty-one patients participated in the study. All patients approached about the study were interested in participating. They were told that a counsellor or social worker would be made available to them should they find the content of the discussion to be emotionally troubling. Following the discussion, they were directed to appropriate resources where they could learn more about advance directives, and how to prepare one of their own, if they so desired.
Evaluation methodology of the questionnaire consisted primarily of a qualitative outcome analysis using Ethnograph softwear.20 Answers to questions regarding advance directives were grouped and coded in terms of similarity and consistency of the various responses. This allowed for more appropriate handling and analysis of the data using the Ethnograph softwear. Simple statistical analysis (number and percentage) was performed on relevant demographic data.
Results
Demographic results are shown in Table 1. Of the 21 patients surveyed, 15 (71.4%) were male. The average age of the study participant was 39.9 years, and the average age at the time of injury was 24.2 years with a range of 10–56 years. Most injuries were caused by motor vehicle accidents (66.7%) followed by sports injuries and falls.
Chi-Square tests were performed to see if the demographic data (specifically the sex of the subject, marital status, living situation, time since the injury and level of education) had any effect on the subsequent answers of the study participants. Three questions in particular were analyzed: (1) the accuracy of the definition of living will; (2) whether participants had discussed their future wishes with anyone; and (3) whether they would now complete a living will. These results are shown in Table 2. The only variables which showed a statistically significant correlation were gender and the likelihood that the participant had discussed their future wishes with anyone, with females (6/6) being more likely to have done so than males (8/15) (P=0.04). There was a general trend that patients who had suffered their injury longer ago were more likely to have discussed their future wishes with someone, but it was not statistically significant (P=0.067). Of interest, there was no correlation between the educational levels of the participants and their ability (or inability) to correctly define the term ‘living will’ (P=0.159).
When asked ‘What do the terms advance directive or living will mean to you?’, there was a fairly wide variety of responses. The response was compared to the ‘gold standard’ answer: ‘Completed by the patient when he or she is capable, the advance directive is invoked in the event that the patient becomes incapable. Advance directives indicate whom the patient would want to make treatment decisions on his or her behalf and what interventions the patient would or would not want in various situations’.21 Results are shown in Table 3.
All of the subjects, after a discussion of the above definition of advance directives, felt that these documents were important. The reasons for this belief varied somewhat (Table 4).
Fourteen of the 21 patients (66.7%) had discussed their wishes in terms of future medical treatment with others. In most cases, discussion occured because they wanted these wishes known and respected (4/14) or because of a recent experience with death (4/14). In three cases the subject arose unexpectedly. Of the 14 patients who discussed the topic with others, two of them prepared a written advance directive following the conversation. Four participants noted that they had verbally made their wishes known to others and now felt that they would be respected, while two participants noted that the discussion seemed to make the other participants uncomfortable, and they were forced to stop.
Of the seven participants who had not discussed their future medical wishes with anyone, five planned to do so at some point in the future, one was unsure and one did not wish to discuss the subject. In all cases the subjects had simply not thought of bringing up the topic.
Only two of the 21 subjects (9.5%) had actually prepared a living will.
Participants were asked to identify those persons with whom they would be most likely to have these discussions. Not unexpectedly, the majority of subjects chose their spouse or common law partner (42.9%) followed by a parent (33.3%) (Table 5). They chose them because these people were close to them and would understand their wishes (14/21) or simply so that someone would know what their wishes were (7/21).
Study subjects were asked to identify who they would choose to make decisions for them in the event they were no longer capable of doing so (ie their proxy decision makers). Eight chose their spouse or common law partner and seven chose a parent (Table 6). Interestingly, none of the participants identified their physician or lawyer, although one noted he would want his ‘executor’ as his proxy without further elaboration. Ten people chose their proxy because they trusted that person to follow their wishes, seven because they have a close relationship with that person and four were unsure why they chose that particular person.
Subjects were asked how long after the spinal cord injury discussion about this topic should take place. Answers to this question varied significantly (Table 7), with six participants feeling it should take place during acute care or the rehabilitation process, 10 feeling it should be delayed until after discharge from rehabilitation and five subjects noting that the decision should depend upon the circumstances of that individual patient.
Towards the end of the discussion, subjects were asked if they would be interested in receiving more information about advance directives. Twenty participants said yes, and one said no. Nine of the subjects wanted more information because they did not know enough about the topic, and seven specifically so that they could prepare an advance directive of their own. When asked if they would now be likely to prepare such a document, after the survey and discussion, 2/21 noted they had already prepared one. Of the 19 remaining subjects, 17 said they would definitely, or most likely, prepare a living will, and only two of the 19 felt that they were unlikely to do so.
Participants were asked to review a generic living will form available on the website of the University of Toronto's Joint Centre for Bioethics.6 They were asked to identify which areas on the form are relevant to spinal cord injured patients, and to discuss issues which would be important to this patient population but are not included on the form (Table 8). Seventeen out of the 21 participants (80.9%) felt that they would be more likely to use a spinal cord injury-specific advance directive rather than a more generic document.
Discussion
In terms of patient demographics, both patient sex (71.4% were male) and patient age at the time of the injury (average 24.2 years) are fairly similar to published values of SCI patients, being 80% male with an average age at the time of injury of 26 years.22,23 The most common cause of injury was motor vehicle accidents, also consistent with the general SCI population.22 Overall, the study population appears to be a good representation of the SCI population at large.
Females were more likely to have discussed their future wishes regarding medical treatment than were males. This is consistent with a previous study involving 214 patients in a general medical clinic, which revealed that 73.1% of females had had discussions with family members versus 49.5% of males.14 The reasons for this discrepancy are unclear, although it may be that females overall are less hesitant to discuss issues of death and dying than are males. More research may be needed to clarify this point.
Although not statistically significant, there was a trend that patients who had suffered their injury longer ago were more likely to have had discussions with others concerning their future wishes. This can likely be explained simply by the fact that these patients had been living with their injuries for a longer period of time and subsequently had more time to talk to others about their wishes.
Only 14.3% of patients were able to convey all of the most important concepts with regards to the definition of a living will, and 42.9% were not able to convey any of the important concepts. While it may seem like SCI patients are therefore poorly informed about living wills, these results are actually comparable to those obtained in the non-SCI population. A study of 105 patients in a general medicine clinic revealed that only 16% of patients were able to define the term ‘living will’.24 Therefore, SCI patients appear to be no worse (or better) informed about living wills than the population at large. One subject fairly accurately described a living will as ‘a pre-judgement on my circumstances at the point of my being unable to communicate my wishes in situations where there are medical decisions to be made’. On the other hand, one subject described a living will as ‘being independent, being healthy, having a healthy lifestyle and living traditionally’. This illustrates the fairly wide variation in responses to this question.
All of the subjects interviewed felt that the topic of advance directives was an important one. This is also consistent with previous studies, which have shown that despite a relatively low level of knowledge about the topic, most people feel that it is an important issue to discuss.14,24 Reasons for feeling this way varied in our study, but a typical response was ‘these documents are important because what you want and what your family wants aren't always the same, and you often have different beliefs. So, between family members and doctors, they can decide what is best for you based on what your wishes are’.
A fairly high percentage of subjects (66.7%) had actually discussed their future wishes with others. This is higher than the percentage of subjects in other studies, which has varied from 19 to 53%.14,24 This indicates that SCI patients seem to be more likely to have discussed their future wishes regarding medical care with someone else, generally because the injury had given them reason to consider the broad topic of end of life issues, and because they wanted to make sure that their loved ones would respect their wishes when the time came.
Subjects prefered to discuss their preferences for future care with their spouse, their parent/s or their sibling/s (in that order). Interestingly, this is somewhat different from at least one study, which showed that the order of preference was doctor, spouse and child.24 Only one SCI patient identified their physician as someone with whom they might have these discussions. The significance of this finding is unclear. However, at least one previous study has shown that the advance care planning process occurs primarily outside of the context of the patient–physician relationship, and rather within the family setting.25 Our findings are consistent with this view.
In general, subjects chose a person with whom to discuss the topic because that person was closest to them and would be most likely to understand their wishes. One participant stated that he had chosen his wife because ‘(she) is most in a position to see that my wishes are followed through’.
When asked why they had discussed these wishes with others, most subjects indicated, in a broad sense, that it was to ensure that their future wishes would be respected. Examples included: ‘So that, hopefully, my wishes would be followed’ and ‘Because I want her to know that's what my wishes are’. Others indicated that they were more aware of end of life issues because of the severity of their injury; for example, ‘Because my life is uncertain because of the medical complications due to my spinal cord injury’.
Those who had not discussed the topic with others stated, for the most part, that it had simply never occurred to them to do so. For example, ‘It has never occurred to me to do such a thing. Now, it is something to think about’ and ‘I never really thought about it’.
The outcome of the discussion was generally quite positive. Only two of the subjects noted that the discussions made the other participants uncomfortable. Most of the subjects felt that the discussions had been helpful in clarifying their future wishes, and one stated that ‘The discussion had a positive outcome, in that they seemed to agree. I can't be sure that they will follow my wishes in the end, but most likely they will’.
SCI patients appear to be equally likely to have prepared an actual written document as those in the general population. Two of the subjects (9.5%) had prepared such a document. This compares favourably to a 1995 study showing that 10% of the general population has prepared a living will.26 However, other studies have shown that only between 0 and 4% of the general internal medicine population has prepared such a document.14,24
In terms of their proxy decision maker, the order of preference for SCI patients was again spouse, parent/s and sibling/s. This contrasts with a previous study24 which showed that the order of preference for general medical patients was spouse, child and doctor. None of the SCI patients identified their physician as someone they might chose as their proxy decision maker.
Most subjects chose their proxy decision maker because they would trust that particular person to make decisions for them. One study subject stated that he had chosen his proxy decision maker because ‘even though she may have reservations about it, she would make the decisions I want’. Others felt that a very close relationship was the most important factor. For example, one subject stated that he would choose his spouse because ‘she's the closest to me, the one who's been with me, she has the closest emotional ties to me and it would be easier for her to decide’.
There was fairly significant variability in terms of when subjects thought the topic of advance directives should be broached with patients following a new spinal cord injury. Overall, six subjects felt that discussion on the topic should occur in acute care or during the rehabilitation process, 10 felt that it should occur after the rehabilitation process and five felt that it depended on the circumstances of the individual patient, and that no specific timeline should be identified.
Those who felt that it should occur earlier on in the recovery process made statements such as: ‘It should be brought up in the last month or so of rehabilitation. At this point, most clients will have come to terms with their injury’ and ‘In acute care would be ideal, but I can't see doing it then because the person would not be able to be objective … Probably in rehabilitation would be appropriate, just to get the discussion going’.
Arguments for delaying the discussion included the following: ‘After discharge. During rehabilitation, the focus should be on getting that person ‘back on their feet’. The focus should be on getting them productive again, and to focus on living, not death. So, after that adjustment had been made’ and ‘After discharge, because it takes a period of time to adapt to your situation. If it's too early on, a person's attitude may be to ‘just let me go’. In rehabilitation, you're still improving your quality of life and your attitude’.
Some felt that the decision should be based on that individual's particular circumstances. They noted that the discussion should occur ‘whenever the individual is comfortable with it; a certain time level cannot be judged’, and ‘whenever that person is comfortable with it. It will vary for everyone, as everyone's different’.
Overall, there was no concensus on when these discussions should take place. Most of the subjects answering the questionnaire were many years post-injury, and were still not able to agree on this point, despite the benefit of hindsight and reflection on their own experiences. It would therefore seem reasonable to make the decision as to when to approach patients about preparing a living will early on during the process, likely during their rehabilitation stay, with the understanding that the patient may want to wait some time before receiving more information. If the health care team feels that the patient is not yet prepared for this discussion, it should be deferred.
For example, the physician (or other team member) might say to the patient: ‘Some individuals in your position have wanted to prepare a living will, which tells us what you would want us to do medically in case you aren't able to do so. For example, whether you would want to be resuscitated if your heart stopped, or whether you would want antibiotics if you developed pneumonia. If you are ready to discuss this now, we can go ahead. If not, we can wait until you have had some more time to adjust to your injury, and discuss it at some point in the future.’ This allows the patient to make the decision and maintain control of the process, while making them aware of the topic in a non-threatening or intimidating way.
Nearly all of the study subjects (95.2%) wanted to receive more information about preparing an advance directive. For most, it was because they did not have enough knowledge about the topic, and to assist them in preparing a document of their own. For example, one subject stated that ‘it's a topic that I need to cover at this point in my life now that I have a family and responsibilities’, while another noted that ‘I have no idea how to go about setting one up and what the legalities are’.
Of the 19 subjects who had not yet completed an advance directive, 17 said that they would definitely or most likely complete one following the discussion and interview. This demonstrates that patients with spinal cord injuries feel that this is an important topic, and recognize the importance of preparing an advance directive, especially after they have received information on the topic.
Subjects were shown an example of a generic living will, and were asked to identify areas on the form which might be relevant to SCI patients. The responses varied significantly, but most subjects agreed that an SCI-specific form should include a section on proxy decision makers and on personal care decisions. One noted that one would have to ‘make a lot of changes to make it relevant or specific to people with spinal cord injuries’.
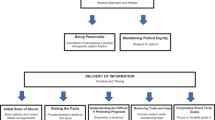
When asked to discuss issues not included on the generic form which might be needed in a SCI-specific form, nearly all the subjects noted that more information should be included about specific medical complications which are more likely to occur in the SCI population. For example, ‘You need further explanation of certain medical scenarios and situations, and their outcomes, specific to spinal cord injuries’. However, only one subject specifically identified such a medical situation, that being autonomic dysreflexia. The authors have prepared an SCI-specific advance directive document (the SCIAD) by including information about potentially life-threatening medical complications and scenarios most likely to occur in the SCI population (see Appendix 2).
The majority of patients (81.0%) felt that they would be more likely to use a SCI-specific document, if one were available, versus a more generic, non-specific document. This compares favourably with results showing that 83% of cancer patients would be more likely to use a cancer-specific advance directive.15 Reasons that subjects would be more likely to use the SCI-specific document included ‘because it would take into account more factors unique to spinal cord injuries’, ‘because so many things are different for a person with a spinal cord injury’ and ‘because it would be specific to me and because it' most likely that any medical complications I would have would be related to my spinal cord injury’.
Study limitations
This study was partly limited by the relatively small number of patients interviewed. This was made necessary by the length of time required to conduct each interview.
Another limitation was the fact that the study sample was essentially a convenience sample, not a randomized sample across the entire spectrum of SCI patients. Although the demographics were in general representative of this population, there were more tetraplegic patients than would be expected in a random sample and patients were relatively well-educated. They were selected from consecutive visits to the primary author's clinic and also from the local branch of the Canadian Paraplegic Association. A more randomized sample may have been preferable, but the sample obtained should not invalidate the results of the study or their generalizability.
Summary
The results of this study show that SCI patients have some knowledge of what is involved in the preparation of an advance directive, and that they feel these documents are very important. A relatively small percentage have completed their own written directives, but nearly all subjects planned to do so after completing this survey.
There is some disagreement about when after the injury the topic should first be discussed. In general, it appears to be reasonable to approach patients during the Rehabilitation process, and be prepared if necessary to delay in-depth discussion until the patient is mentally and emotionally ready.
Patients with a spinal cord injury seem to be more likely to complete a SCI-specific document rather then a more generic one. The SCIAD includes information about medical conditions which are more likely to arise following a SCI and is now available for SCI patients to complete so that their future care wishes will be clear to their families, loved ones and health care providers.
References
Blondeau D et al. Comparison of patients' and health care professionals' attitudes toward advance care directives J Med Ethics 1998 24: 328–335
Nolan MT, Bruder M . Patients' attitudes toward advance directives and end-of-life treatment decisions Nurs Outlook 1997 45: 204–208
Davidson KW, Hackler C, Caradine DR, McCord RS . Physicians' attitudes in advance directives JAMA 1989 262: 2415–2419
Emanuel LL et al. Advance directives for medical care–a case for greater use N Engl J Med 1991 324: 889–895
Miller DL, Bolla LR . Patient values: The guide to medical decision making Clin Geriatr Med 1998 14: 813–829
Heffner JE, Fahy B, Hilling L, Barbieri C . Outcomes of advance directive education of pulmonary rehabilitation patients Am J Respir Crit Care Med 1997 155: 1055–1059
Heffner JE, Fahy B, Hilling L, Barbieri C . Attitudes regarding advance directives among patients in pulmonary rehabilitation Am J Respir Crit Care Med 1996 154: 1735–1740
Holley JL, Nespor S, Rault R . The effects of providing chronic hemodialysis patients written materials on advance directives Am J Kidney Dis 1993 22: 413–418
Sehgal A et al. How strictly do dialysis patients want their advance directives followed? JAMA 1992 267: 59–63
Voltz R et al. End-of-life decisions and advance directives in palliative care: a cross-cultural survey of patients and health care professionals J Pain Symptom Management 1998 16: 153–162
Heffner JE . End-of-life ethical issues Respir Care Clin N Am 1998 4: 541–559
Heffner JE, Barbieri C . End-of-life care preferences of patients enrolled in cardiovascular rehabilitation programs Chest 2000 117: 1474–1481
Joos SK, Reuler JB, Powell JL, Hickman DH . Outpatients' attitudes and understanding regarding living wills J Gen Intern Med 1993 8: 259–263
Berry SR, Singer PA . The cancer specific advance directive Cancer 1998 82: 1570–1577
Martin DK, Thiel EC, Singer PA . A new model of advance care planning: Observations from people with HIV Arch Intern Med 1999 159: 86–92
Vargo J . Do not resuscitate orders: have you had yours? Caliper 1998 53: 36
Prince JM, Manley MS, Whiteneck GG . Self-managed versus agency-provided personal assistance care for individuals with high level tetraplegia Arch Phys Med Rehabil 1995 76: 919–923
Bach CA, McDaniel RW . Quality of life in quadriplegic adults: a focus group study Rehabil Nurs 1993 18: 364–367
Ethnograph v5.0. Qualis Research Associates, Scolari Sage Publications Softwear Ltd 1998
Singer PA, Robertson G, Roy DJ . Bioethics for clinicians: 6. Advance Care Planning CMAJ 1996 155: 1689–1692
National Spinal Cord injury Statistical Center. Spinal Cord Injury: Facts and Figures at a Glance 1998 Birmingham, University of Alabama at Birmingham 1998
Berkowitz M et al.. The Economic Consequences of Traumatic Spinal Cord Injury New York, Demos 1992
Sam M, Singer PA . Canadian outpatients and advance directives: poor knowledge and little experience but positive attitudes CMAJ 1993 148: 1497–1502
Singer PA et al. Reconceptualizing advance care planning from the patient's perspective Arch Intern Med 1998 158: 879–884
Singer PA et al. Public opinion regarding end of life decisions: influence of prognosis, practice and process Soc Sci Med 1995 41: 1517–1521
Acknowledgements
The authors wish to thank the University of Saskatchewan for their assistance through the provision of a Young Investigator's Research Grant. The primary author wishes to thank Susan Blackmer for her assistance and support with preparation and revision of the manuscript.
Author information
Authors and Affiliations
Appendices
Appendix 1
SCIAD questionnaire
-
1)
Demographics
-
a)
Name
-
b)
Sex
-
c)
Age
-
d)
Date of injury
-
e)
Cause of injury
-
f)
Level of injury
-
g)
Complete or incomplete
-
h)
Marital status
-
i)
Educational level
-
j)
Living situation
-
a)
-
2)
Knowledge of advance directives
-
a)
What do the terms ‘advance directive’ or ‘living will’ mean to you?
-
b)
Why do you think these documents are, or are not, important?
-
c)
Have you discussed your future wishes with anyone?
-
– If yes: Why? What was the outcome?
-
– If no: Why not? Had you planned to do so in the future?
-
-
d)
With whom would you most want to discuss these issues and why?
-
e)
Who would you choose to make decisions for you (proxy, substitute decision maker) and why?
-
f)
When do you think discussion about advance directives should be initiated (ie how long after the injury – in acute care, on rehab or after discharge)?
-
g)
Are you interested in receiving more information about advance directives?
-
– Why?
-
– Why not?
-
-
h)
Do you think you will now complete an advance directive document?
-
– Why?
-
– Why not?
-
-
a)
-
3)
SCI-specific advance directives
-
a)
After having reviewed the U of T Joint Centre for Bioethics form, which areas or problems identified on the form are relevant to SCI patients?
-
b)
Please discuss some issues which are not included on this form but which you feel are of importance to yourself specifically and other SCI patients generally.
-
c)
Do you feel you would be more likely to use a SCIAD form then a generic form if one were available?
-
– Why?
-
– Why not?
-
-
a)
Appendix 2
The Spinal Cord Injury Advance Directive (SCIAD)
This living will is a legal document. Although you can complete this form without a lawyer, it may be helpful to consult a lawyer with experience in this area.
The SCIAD contains medical information to help you make decisions. This medical information is directed specifically towards patients with spinal cord injuries (SCI). If you have questions about the descriptions of health situations or treatments, or about your own medical conditions and what might happen to you in the future, you should discuss these with your doctor.
Make copies of your SCIAD for yourself and your proxy (the person you are going to designate to make decisions for you in the event you are no longer able to do so). If you change your mind about who you want to be your proxy, or about your wishes regarding treatment, change your living will and give copies of the new one to anyone who has a copy of the old one. Then, destroy all copies of your old living will.
Proxies
The proxy must follow the wishes of the person making the living will. In situations for which the person has not specified a wish, the proxy would make the decision based on the person's best interests, taking into consideration the person's values and beliefs.
If you name more than one person to act as your proxy, you should say how they will make decisions. There are two options:
First, you can have your proxies make decisions individually, in the order that you list them in your living will. If the first named proxy is unavailable, or has died, then the next proxy listed in your living will would make the necessary decisions on your behalf, and so on.
Second, you can say in your living will that you want your proxies to make decisions as a group. If you want your proxies to make decisions as a group, you should indicate how you would like disagreements between your proxies to be resolved. This could be by majority vote or by giving your first-named proxy the final say.
The wishes contained in this living will are intended to help your proxy(ies) understand what you want. You can also say how much leeway your proxy should have in interpreting your wishes; ie, do you want your instructions followed exactly or used only as a guideline?
Rights and permissions
About this article
Cite this article
Blackmer, J., Ross, L. Awareness and use of advance directives in the spinal cord injured population. Spinal Cord 40, 581–594 (2002). https://doi.org/10.1038/sj.sc.3101352
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101352
Keywords
This article is cited by
-
Experiences with euthanasia requests of persons with SCI in Belgium
Spinal Cord Series and Cases (2018)
-
Knowledge, attitudes, and influencing factors of cancer patients toward approving advance directives in China
Supportive Care in Cancer (2016)