Abstract
Study design
Mixed-method study (small group discussions and online literature search).
Objectives
Identify the ethical issues and dilemmas faced by rehabilitation professionals involved in the service delivery to the persons with spinal cord injury (SCI) in the low income and lower-middle-income countries (LIC/LMIC) located in Asia.
Setting
Small group discussions in three biomedical conferences in Dhaka, Bangladesh and Kualalampur, Malaysia.
Methods
Three small group discussions (30–45 min each) were held during three international conferences in 2019. The conferences brought together experts in the fields of neurology, rehabilitation, neurorehabilitation, and bioethics. A summary of SCI practice points and dilemmas were documented including goals of care, duties of rehabilitation professionals, health care worker-patient relationships, roles, and expectations of family members at different care settings.
Results
There is a paucity of literature on this topic. The application of the principles of contemporary bioethics in the pluralistic societies of LIC/LMIC can be challenging. The ethical dilemmas faced by rehabilitation professionals working in LIC/LMIC are diverse and different from those reported from the Western and developed countries. Ethical issues and dilemmas identified were understanding patient autonomy in decision making, lack of insurance for SCI rehabilitation, financial challenges, challenges of providing emerging technology in SCI rehabilitation and SCI rehabilitation during disasters.
Conclusions
We have summarized the possible ethical issues and dilemmas which rehabilitation professionals in LIC/LMIC may encounter during delivery of SCI rehabilitation services. We hope it generates a discussion on an often-neglected aspect of SCI care in the LIC/LMIC and helps identify the complexities of ethical dilemmas unique to persons with SCI living in a developing country.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) is a devastating neurological injury. Depending upon the level and severity of the injury it can result in varying levels of disability and restriction of mobility. The cost of treatment of an individual with SCI is high and their quality of life particularly in the low- and middle-income countries (LIC/LMIC) is generally poor [1, 2]. Rehabilitation of people with SCI is challenging, time intensive and costly. Rehabilitation of SCI is typically a team-based task led by a rehabilitation medicine physician. Depending upon the available expertise and resources, the team may include physiotherapist, occupational therapist, rehabilitation nurse, nutritionist, speech language therapist, social worker, clinical psychologist, and other rehabilitation professionals, as necessary. Comprehensive SCI management and integrated rehabilitation have substantially improved in the developed countries. But there still are challenges in the continuum of team care starting from the site of injury, acute or critical care and rehabilitation at home or community level follow-up and inclusions [3, 4]. Most of the available literature on persons with SCI is on medical issues like pain, depression, fatigue, pressure ulcer, spasticity, bladder, and bowel dysfunction [5] and newer rehabilitation interventions like robotics and neuroprosthetics [6, 7]. The literature on dilemma and ethical issues and dilemmas in SCI care and rehabilitation is scant and have been published from the developed world only [8, 9]. Recent recognitions of moral dilemmas related to care in rehabilitation medicine has increased interest in ethical aspects in persons with SCI. However, developments in ethical aspects of SCI did not keep pace with the technological and service developments. A discussion of ethical aspects of rehabilitation care in SCI is relatively new amongst clinicians particularly those based in the LIC/LMIC.
The contemporary bioethics as understood and practiced around the globe started in the USA in the latter half of the twentieth century [10]. The most common approach to clinical ethical analysis is principlism, which was proposed first by the “Belmont Report” [11] and then popularized by Beauchamp and Childress in their influential book on contemporary bioethics [12]. The four principles include respect for autonomy, beneficence, nonmaleficence, and justice. Although these principles were created in the Western society with their own culture and social issues, they are widely used and applied all around the globe in different contexts [13]. However, as Moazam pointed out that the application of Principlism without considering the local context and culture can be problematic and even counterproductive [14].
SCI management and rehabilitation presents with a particular set of ethical dilemmas and challenges which need to be considered carefully during service delivery and interaction with the patient and the care givers [8]. These have been discussed in the international SCI literature as early as 1987 [15]. However, there is no discussion or documentation of the ethical issues related to SCI management and rehabilitation of the persons based in the LIC/LMIC. There is evidence that the demographics, clinical profile, and functional outcomes of persons with SCI in the low resource developing countries are different from those reported from the developed world [16,17,18]. Therefore, as professionals based in LIC/LMIC we believe that the ethical dilemmas and challenges of these persons with SCI will also be different.
We conducted this study to highlight the ethical issues which rehabilitation professionals in the developing countries, particularly Asian countries may encounter during delivery of SCI rehabilitation services and suggest some possible solutions. The aim is to initiate a discussion on this often-neglected aspect of SCI care in the developing world and to identify the ethical dilemmas unique to persons with SCI living in a developing country.
Methods
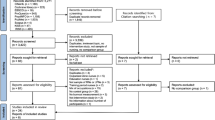
This was a mixed-method study combining results from three small group discussions with an online literature search. The three international meetings, where small group discussions were held included Asian Spinal Cord Network Meeting, 2019, Malaysia, Asian Bioethics Conference 2019, Dhaka, Bangladesh and International Conference on Neuromodulation 2019 Dhaka, Bangladesh. These conferences brought together experts in the fields of neurology, rehabilitation, neurosurgery, neurorehabilitation, and bioethics over a course of 2–4 days. The small group discussions lasted from 30–60 min. It was moderated and the minutes of the discussions/meetings were recorded by the principal author. There was no specific layout plan for these meetings. All participants were encouraged to share their experiences and express their concerns regarding the ethical issues in the rehabilitation management of persons with SCI. Participants were also asked to recommend possible solutions to these ethical dilemmas. Most of the participants of these meetings were physicians from the LIC/LMIC including Bangladesh, India, Myanmar, Nepal and Sri-Lanka who were actively working with persons with SCI in indoor and outdoor settings.
Online literature search was carried out on Medline, PubMed Central and Google Scholar using keywords “bioethics”, “dilemmas”, “spinal injuries”, “spinal cord injury”, “persons with disability”, “neurological rehabilitation”, “developing countries”, “biomedical ethics”,” paraplegia”, “tetraplegia” and “quadriplegia”. Boolean operators (“AND”, “OR” and “NOT”) were used to combine search terms. Search was limited only to English language manuscripts with no time and manuscript type limits. The literature search was last done on 15th Sept 2020.
Results
All participants had experience of managing patients with SCI either in the acute, sub-acute, long-term, rehabilitation and follow-up phase. The work experience of the participants in their respective fields ranged from 7–20 years. The most common causes of SCI in the LIC/LMIC reported by the participants were road traffic accident, fall from height, gunshot injury, inflammation and infections which is like the data reported in the literature [4, 16]. Participants mentioned that the initial care of SCI in their countries was inadequate and there were few centers providing a comprehensive multi-disciplinary SCI rehabilitation. Table 1 presents a summary of SCI practice points along with the dilemmas and ethical issues being faced.
Discussion
SCI is a complex and disabling condition associated with high mortality and morbidity. The noticeable improvements in SCI services and outcomes over the years have mostly occurred in the high-income regions of the world. Patients with SCI in the LIC/LMIC still face medical, social, cultural and economic challenges [19]. Ethics are reflections of the societal and cultural norms, which is also related to the time and place. While some principles are advocated as universal principles [20], their on-ground application differs according to the context.
For example, a great emphasis is placed on personal autonomy and individualism in the Western countries. A person with SCI may independently choose the treatment and rehabilitation plan she/he considers appropriate without any external influence or involvement of the family members [8]. However, this concept of autonomy has been critiqued as it does not consider other cultures outside the Western societies [21]. In addition in most of the developing countries, particularly Asian and Eastern cultures, “a person does not exist as an individual but as a member of the family, community or society” [22].
Family is considered an important part of the decision-making process and are actively involved in all medical decision making. Many family members and relatives are available with the patient throughout their stay in the rehabilitation wards. They actively participate in the medical decision making and often are seen communicating on the behalf of the patient. This is particularly seen in children and elderly with SCI. This is due to the societal norms, where taking care of the children and elderly is considered social, moral and religious responsibility of the parents and children respectively. Many a times decisions are taken and communicated to the rehabilitation team on their behalf are, mostly without involving them.
In addition, after discharge from the hospital, for most patients with SCI family members are the primary caregivers for majority of the patients with SCI. This may result in a conflict with the physician or the rehabilitation team if they emphasize on the patient’s autonomy and do not involve family and relatives in the decision-making process. The concept of autonomy is not only related to the decision-making process while the patient is admitted to the hospital. Autonomy, at least in the Western view also determines how much independence or caregiving by the family is desired ultimately by the patient. As mentioned previously due to the hierarchical structure of the society and the socio-cultural norms patients usually do not decide about these issues and have to depend upon the family, caregiver and parents to make this decision.
Medical paternalism is generally looked down upon in the West. Patient autonomy and choice are now an integral part of patient care pathways. There has been a steady shift in patient counseling and consent toward supporting patient autonomy over medical paternalism [23]. However, some have argued the extremes of autonomy and paternalism are not compatible in a responsive, responsible and moral health care environment, and thus some compromise of these values is unavoidable [24]. Soft medical paternalism is still practiced in most of the LIC/LMIC where the patients often allow, actively ask or even expect their physicians to make decisions on their behalf. This may appear problematic to many bioethicists, but it should be considered as more of a cultural norm than the ethical dilemma.
The core ethical principles of beneficence (do good), nonmaleficence (do not harm), autonomy (control by the individual), and justice (fairness) [12] also apply to the decision making and service provision in SCI rehabilitation. There have been some remarkable advances in the SCI management and rehabilitation in the few decades and all of these are only available in the Western and developed countries [7, 25]. Due to the access to the internet, patients in the LIC/LMIC are often aware of these advances and may ask the rehabilitation medicine physician to recommend these latest technologies. This becomes a dilemma when the patient has resources to secure funds from the government which are not routinely available to all persons with SCI. The principle of beneficence supports recommending these novel technologies, but it violates the principle of distributive justice as it only favors the provision of service to those with connections and resources to secure funds. In addition, none of these have been tested or used in the LIC/LMIC, the outcomes are not clear, and safety not established. Considering the principle of nonmaleficence recommending these technologies might not be an appropriate choice in such cases.
After SCI, for some patients particularly high tetraplegic life becomes difficult, sedentary with often chronic intractable pain requiring costly medications and treatment. They may be totally dependent on their care givers, confined to a powered wheelchair, needing permanent artificial respiration and a complicated, computerized environmental control system. As autonomous beings, they may request an end to their prolonged suffering in form of medically assisted dying or euthanasia [26]. Euthanasia is a controversial issue in SCI, practiced in the Western world but unheard of in LIC/LMICs [26, 27]. Some participants of the workshops reported that few of their patients with cervical SCI expressed that they were exhausted and would like to end their lives. However, none requested active euthanasia and such expressions were attributed to low mood and depression. A request for active euthanasia will be likely be refused by a rehabilitation professional in a LIC/LMIC due to the religious beliefs, cultural issues or medico-legal issues. All participants agreed upon this.
Persons with SCI are considered vulnerable population due to the nature of their disability. Special care must be taken while conducting research in this group to avoid any ethical conflicts. The International Campaign for Cures of Spinal Cord Injury Paralysis has established a panel to review methods for clinical trials for SCI. They recommend undertaking clinical trials with prospective blinded design maintaining highest ethical standards, obtaining adequate and a clear informed consent [28]. It is important to note that many of the issues identified by the experts were not specific to SCI alone. Patients with other neurological disabilities and rehabilitation professionals residing in these countries can also face the same ethical challenges.
Another potential issue faced by women with SCI is of discrimination. Men are usually the main bread earners in the LMIC located in this region and may get preferential treatment by the family. There is anecdotal evidence that women with SCI do not get the same level of attention and care in the long term after discharge from the hospital. For example, the Oct 2005 earthquake in Pakistan resulted in hundreds of patients with SCI, mainly paraplegia. Irhsad et al. documented the long-term gendered consequences of SCI on women [29]. The findings show that 3 years after the disaster, paraplegic women are socially, emotionally, and financially isolated. The small stipend they received was a significant source of income, but also led to marital distrust, violence, and abuse. In contrast, men received full social and emotional support [29].
The ethical challenges faced by health care professionals dealing with SCI are also complicated by the fact that hospital ethics committees do not exist or have not been appropriately established in some developing countries [30]. In some places they are only exist on paper without performing any actual task. Therefore, the professionals are unable to obtain timely ethical consult and solution to a dilemma arises during SCI rehabilitation. A proposed framework for solving ethical dilemmas arising during SCI rehabilitation is presented in Fig. 1.
There are certain limitations which warrant mention. The focused group discussions were not based on a structured format and the discussions varied in different meetings. The minutes were recorded by one person using a paper and pen instead of recording the conversation and transcribing it verbatim. It might have resulted in some of the point of views being missed from the final compilation. The dilemmas and ethical issues identified are from the physicians and rehabilitation professional perspectives only. No persons with SCI or their care givers were part of the discussions. There is a possibility that those who are living the experience may identify or prioritize different ethical issues than the ones mentioned here.
Conclusion
This is one of the first report to document the ethical issues and dilemmas unique to SCI rehabilitation in the LIC/LMIC located in Asia. It appears that these ethical issues are common, unique to these areas, underreported and do not receive much attention. They can adversely affect the patient motivation to participate in the long-term rehabilitation program and the relationship between the SCI patient and the rehabilitation professionals involved. There is a need to formally document the ethical dilemmas and challenges faced both by the persons with SCI and their rehabilitation providers using well designed studies. In addition, a discussion of ethical issues related to SCI care and rehabilitation must be a part of the training curriculum of different rehabilitation professionals.
References
Hossain MS, Rahman MA, Bowden JL, Quadir MM, Herbert RD, Harvey LA, et al. Psychological and socioeconomic status, complications and quality of life in people with spinal cord injuries after discharge from hospital in Bangladesh: a cohort study. Spinal Cord. 2016;54:483–9. https://doi.org/10.1038/sc.2015.179.
Hossain MS, Islam MS, Rahman MA, Glinsky JV, Herbert RD, Ducharme S, et al. Health status, quality of life and socioeconomic situation of people with spinal cord injuries six years after discharge from a hospital in Bangladesh. Spinal Cord. 2019;57:652–61. https://doi.org/10.1038/s41393-019-0261-9.
Chhabra HS, Sharma S, Arora M. Challenges in comprehensive management of spinal cord injury in India and in the Asian Spinal Cord network region: findings of a survey of experts, patients and consumers. Spinal Cord. 2018;56:71–77. https://doi.org/10.1038/sc.2017.102.
Rathore MF, Hanif S, Farooq F, Ahmad N, Mansoor SN. Traumatic spinal cord injuries at a tertiary care rehabilitation institute in Pakistan. J Pak Med Assoc. 2008;58:53–7.
Sweis R, Biller J. Systemic complications of spinal cord injury. Curr Neurol Neurosci Rep. 2017;17:8. https://doi.org/10.1007/s11910-017-0715-4.
Kinnett-Hopkins D, Mummidisetty CK, Ehrlich-Jones L, Crown D, Bond RA, Applebaum MH, et al. Users with spinal cord injury experience of robotic Locomotor exoskeletons: a qualitative study of the benefits, limitations, and recommendations. J Neuroeng Rehabil. 2020;17:124. https://doi.org/10.1186/s12984-020-0075.
Cho N, Squair JW, Bloch J, Courtine G. Neurorestorative interventions involving bioelectronic implants after spinal cord injury. Bioelectron Med. 2019;11:10. https://doi.org/10.1186/s42234-019-0027-x.
Donovan WH. Ethics, health care and spinal cord injury: research, practice and finance. Spinal Cord. 2011;49:162–74. https://doi.org/10.1038/sc.2010.106.
Andrade VS, Faleiros F, Balestrero LM, Romeiro V, Santos CBD. Social participation and personal autonomy of individuals with spinal cord injury. Rev Bras Enferm. 2019;72:241–7. https://doi.org/10.1590/0034-7167-2018-0020.
Gordon JS. Bioethics internet encyclopedia of philosophy. 2021. Available at https://iep.utm.edu/bioethic/#H2. accessed 1st. August 2021
Department of Health, Education, and Welfare; National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. The Belmont Report. Ethical principles and guidelines for the protection of human subjects of research. J Am Coll Dent. 2014;81:4–13.
Beauchamp TL, Childress JF. Principles of biomedical ethics. Oxford: Oxford University Press; 1979.
Niebroj L. Bioethics of life programs: taking seriously moral pluralism in clinical settings. Eur J Med Res. 2010;15:98–101. https://doi.org/10.1186/2047-783x-15-s2-98.
Moazam F. Reading Caplan in Karachi. Indian J Med Ethics. 2018;3:66–7. https://doi.org/10.20529/IJME.2017.086.
Ohry A. Ethical questions in the treatment of spinal cord injured patients. Paraplegia. 1987;25:293–5. https://doi.org/10.1038/sc.1987.54.
Ning GZ, Wu Q, Li YL, Feng SQ. Epidemiology of traumatic spinal cord injury in Asia: a systematic review. J Spinal Cord Med. 2012;35:229–39. https://doi.org/10.1179/2045772312Y.0000000021.
Rahman A, Ahmed S, Sultana R, Taoheed F, Andalib A, Arafat SMY, et al. Epidemiology of spinal cord injury in Bangladesh: a five year observation from a rehabilitation center. J Spine. 2017;6:367. https://doi.org/10.4172/2165-7939.1000367.
Yusuf AS, Mahmud MR, Alfin DJ, Gana SI, Timothy S, Nwaribe EE, et al. Clinical characteristics and challenges of management of traumatic spinal cord injury in a trauma center of a developing country. J Neurosci Rural Pr. 2019;10:393–9. https://doi.org/10.1055/s-0039-1695696.
Burns AS, O’Connell C. The challenge of spinal cord injury care in the developing world. J Spinal Cord Med. 2012;35:3–8. https://doi.org/10.1179/2045772311Y.0000000043.
Colero L. A framework for universal principles of ethics. 2021. https://ethics.ubc.ca/papers/invited/colero-html/. accessed 2nd August 2021
Saadah MA. On autonomy and participation in rehabilitation. Disabil Rehabil. 2002;24:977–82.
Tanida N. ‘Bioethics’ is subordinate to morality in Japan. Bioethics. 1996;10:201–11. https://doi.org/10.1111/j.1467-8519.1996.tb00119.x.
Sood A, Gupta J. Patient counselling and consent. Best Pr Res Clin Obstet Gynaecol. 2018;46:43–47. https://doi.org/10.1016/j.bpobgyn.2017.10.002.
Aggarwal A, Davies J, Sullivan R. “Nudge” in the clinical consultation—an acceptable form of medical paternalism? BMC Med Ethics. 2014;17:31. https://doi.org/10.1186/1472-6939-15-31.
Mekki M, Delgado AD, Fry A, Putrino D, Huang V. Robotic rehabilitation and spinal cord injury: a narrative review. Neurotherapeutics. 2018;15:604–17. https://doi.org/10.1007/s13311-018-0642-3.
Waals EMF, Post MWM, Peers K, Kiekens C. Experiences with euthanasia requests of persons with SCI in Belgium. Spinal Cord Ser Cases. 2018;4:62. https://doi.org/10.1038/s41394-018-0101-8.
Tchajkova N, Ethans K, Smith SD. Inside the lived perspective of life after spinal cord injury: a qualitative study of the desire to live and not live, including with assisted dying. Spinal Cord. 2021;59:485–92. https://doi.org/10.1038/s41393-021-00619-3.
Tuszynski MH, Steeves JD, Fawcett JW. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP Panel: clinical trial inclusion/exclusion criteria and ethics. Spinal Cord. 2007;45:222–31. https://doi.org/10.1038/sj.sc.3102009.
Irshad H, Mumtaz Z, Levay A. Long-term gendered consequences of permanent disabilities caused by the 2005 Pakistan earthquake. Disasters. 2012;36:452–64. https://doi.org/10.1111/j.1467-7717.2011.01265.x.
Hajibabaee F, Joolaee S, Cheraghi MA, Salari P, Rodney P. Hospital/clinical ethics committees’ notion: an overview. J Med Ethics Hist Med. 2016;9:17.
Acknowledgements
We gratefully acknowledge the experience sharing of all participants of the group discussion.
Author information
Authors and Affiliations
Contributions
TU gave the idea for the study. He was responsible for collecting responses from the participants and summarizing them for this manuscript. He carried out the revisions and gave approval for the final version of the article. MAS performed the initial literature search. He contributed to writing the first draft, extracting and analyzing data, interpreting results. He gave approval for the final version of the article. FAR performed the literature search, extracted data revised the first draft. He gave approval for the final version of the article. MS contributed to revising the first draft, extracting, and analyzing data, interpreting results, and gave approval for the final version of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Uddin, T., Shakoor, M.A., Rathore, F.A. et al. Ethical issues and dilemmas in spinal cord injury rehabilitation in the developing world: a mixed-method study. Spinal Cord 60, 882–887 (2022). https://doi.org/10.1038/s41393-022-00808-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00808-8