Abstract
Objectives: To determine the predictive utility of verbal descriptors to distinguish between pain types following spinal cord injury (SCI).
Design: Cross-sectional.
Setting: USA.
Methods: Participants (n=29) completed the Short Form – McGill Pain Questionnaire (SF-MPQ) for each pain site reported. A total of 64 pain sites were reported with 80% of the sample reporting multiple pain sites. Each pain site was categorized using three different SCI pain classification schemes. The predictive utility of verbal descriptors to distinguish between pain types was examined statistically using (1) each word separately, (2) a combination of words (ie, the SF-MPQ total subscales, the number of words chosen on each scale), and (3) discriminant function analysis.
Results: There was a substantial overlap in the use of verbal descriptors across pain types. Few differences across pain types were found for endorsement of individual words, and differences across pain types were not found for any of the word combination scores. The majority of the verbal descriptors did not enter the step-wise discriminant functions for each SCI pain classification scheme, however, ‘tingling’ and ‘aching’ showed modest predictive utility for neuropathic and musculoskeletal pain, respectively. Correct classification was in the low range (ie, 39% to 82%, average=60%, with a 33% chance level). All three pain classification schemes showed the same general pattern of results.
Conclusion: In general, verbal descriptors alone offered marginal utility with regard to identifying specific pain types following SCI. Future directions alone and implications are discussed.
Similar content being viewed by others
Introduction
Unfortunately, pain is a common secondary complication following spinal cord injury (SCI) with prevalence estimates ranging from 18% to 96%.1,2,3,4,5 Although there is general agreement regarding the importance of research in this area, there is relatively little agreement regarding how to classify the different types of pain following SCI. Indeed, review of the SCI literature produced a total of 29 proposed pain classification schemes (note: Siddal and colleagues were considered as three separate schemes) describing between two and 12 different types of pain.2,3,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32 At least part of the disparity in the SCI pain classification literature may be attributable to the divergent approaches to pain assessment.
In general, pain classification schemes involve some combination of two complementary approaches. The mechanistic approach tends to emphasize the underlying pathophysiology associated with the different types of pain as a means to classify pain, whereas the descriptive approach classifies the different types of pain based on the presenting symptomotology and pain behavior. Table 1 presents a summary of the most common characteristics used to categorize the different types of pain across the 29 classification schemes reviewed. As can be seen, verbal descriptors were the most common characteristic (96% of the classification schemes) used to classify pain following SCI. Using the 29 different classification schemes, the different types of pain were separated into three general categories (ie, mechanical, neuropathic, visceral), and the verbal descriptors associated with each pain category were counted. Table 2 presents a summary of the proportion of scales in the literature using the most common verbal descriptors across pain types. With few exceptions, the results showed that there was (1) little agreement on which verbal descriptors are associated with a particular pain type, and (2) considerable overlap for the use of a specific verbal descriptor across pain types. For instance, the only verbal descriptor with complete agreement across the various pain classification schemes was ‘burning’ as an indicator of neuropathic pain. However, the verbal descriptor ‘burning’ was also used as an indicator of visceral pain in 23% of the classification schemes. Although verbal descriptors are commonly accepted as an important criterion for classification of pain following SCI, there have been no studies, to the authors' knowledge, that have examined the predictive validity of verbal descriptors to classify pain following SCI.
Previous research examining the utility of verbal descriptors for distinguishing between different types of pain has been mixed. For instance, accurate pain classification rates using verbal descriptors, primarily from the McGill Pain Questionnaire,33 have shown considerable promise in some studies (ie, about 65% to 90% accurate classification),34,35,36,37,38,39,40 even between closely related diagnostic groups (eg, trigeminal neuralgia, vs atypical facial pain).41,42,43,44,45 In contrast, others have found little or no benefit from the use of verbal descriptors to classify pain associated with different disease states.46,47,48,49,50,51,52 The inconsistent results within this area of research can be attributed to, in part, several methodological limitations. Of primary concern, previous research has assumed that (1) participants had, and reported on, only one pain site, or, in the case of multiple pain sites or systemic disease, all sites were thought to be a similar pain type, and (2) a disease state (eg, prostate cancer) is associated with only one type of pain. In addition, variability in pain classification [ie, the use of alternate classification schemes] has not been addressed in previous research.
The proposed research was designed to extend previous research examining the utility of verbal descriptors as a mechanism to distinguish between the various types of SCI pain. Participants were allowed to report multiple pain sites, and verbal descriptors were collected for each pain site. In addition, three separate classification schemes were used to categorize the type of pain for each site. Taken together, the current design was thought to allow for a more specific assessment of the pain site of interest, and account for variability in approaches to pain classification.
Methods
Participants
A total of 29 individuals with traumatic onset SCI were recruited for study (note: 28 of these individuals and their pain sites were used in a previous study53 examining the incremental utility of the pain classification criteria on the Donovan17 scheme). To be included for study, participants had to be 18 years or older and have reported experiencing at least one pain site. Participants were recruited from the spinal cord injury clinic at the University of Alabama at Birmingham and through local advertisement. Participants were paid $25 for their participation.
Measures
Three SCI pain classification schemes were chosen that were thought to incorporate the common core characteristics across pain classification schemes, yet also offer unique pain types or classification criteria. The three pain classification schemes chosen for inclusion were (1) the International Association for the Study of Pain (IASP) model,29 (2) the Donovan scheme,17 and (3) the Tunks scheme.30 The pain types and associated classification criteria have been discussed in detail elsewhere.17,29,30 As seen in Table 3, the IASP model classifies pain into five types (ie, nociceptive, musculoskeletal and visceral pain, neuropathic above, at, and below lesion level pain). The Donovan scheme has five pain types (ie segmental nerve/cauda equina, spinal cord, visceral, mechanical, and psychogenic). Finally, the Tunks model identifies nine pain types (ie, above lesion level myofascial, syringomyelia, and non-SCI pain; at lesion level radicular, hyperalgesic border reactions, myofascial (incomplete lesions), and fracture site pain; below level burning, phantom, myofascial (incomplete lesions), and visceral pain; note: myofascial pains were collapsed into one category).
The short-form McGill Pain Questionnaire (SF-MPQ)37 consists of 15 representative words from the sensory (n=11) and affective n=4) categories of the standard long-form McGill Pain Questionnaire. Pain intensity is ranked for each word (see Table 5 for list of descriptors) using a four point Likert scale (0=no pain, 1=mild; 2=moderate, and 3=severe). Two pain scores are derived from the sum of the intensity ratings for the sensory and affective scale. A total score is calculated by summing the sensory and affective scores. The SF-MPQ also includes the Present Pain Intensity (PPI) index of the long-form MPQ, a six point Likert scale ranging from ‘no pain’ to ‘excruciating’. The correlations between the corresponding scales on the short- and long-form MPQ are generally high (r's=0.68 to 0.92).37,54 In addition, the SF-MPQ has been shown to be sensitive to a variety of clinical interventions across numerous medical populations.55 Two additional words from the long form MPQ, tingling and numbness, were added since these words were associated with different pain types on two of the three classification schemes.
Procedure
After obtaining informed consent, participants completed a questionnaire assessing demographic and injury related characteristics. Participants were administered a semi-structured interview designed to elicit information on ‘all of the places you have pain.’ Participants were allowed to report multiple pain sites, however, they were told ‘you may have pain in several different places that to you is the same kind of pain. If this is so, we will ask you to group those pains together and answer questions about them as a group.’ A separate SF-MPQ was completed for each pain site. The semi-structured interview was videotaped, and the type of pain for each site was determined using each of the three different classification schemes. A total of 64 pain sites were classified.
Statistical analysis
For each classification scheme, several statistical methods were used to determine the utility of verbal descriptors for distinguishing between pain types. First, a Chi-square analysis was performed to determine whether the proportion of individuals endorsing each verbal descriptor (four levels) differed across pain types. Next, a separate analysis of variance (ANOVA) for each classification scheme was performed with pain type as the independent grouping factor, and the McGill Pain Questionnaire – Total and subscale scores as the dependent factors. Correspondingly, an ANOVA was performed using pain type as the independent grouping factor, and the mean number of words endorsed on the McGill Pain Questionnaire total scale, and the two subscales as the dependent factors. Finally, a step-wise discriminant function analysis was used to determine if a unique set of verbal descriptors may be associated with the different types of pain. The score for each verbal descriptor in the discriminant function analysis was equal to the value chosen for that word (0=no pain to 3=severe pain). The linear functions were calculated so that scores on all discriminant functions were orthogonal (ie, uncorrelated). Two different step-wise classification methods were used to determine variables that entered the model, (1) change in Wilks' Lambda and (2) maximization of Mahalanobis distance. Both methods generated the same set of significant verbal descriptors. Thus only the results of Wilks' Lambda method were reported. Discriminant function analysis generates G-1 or k discriminant functions, whichever is smaller, where G equals the number of groups and k equals the number of predictor variables. In order to ensure adequate sample size for between group analyses, only the three most common pain types from each classification scheme were used (this excluded 1, 1, and 24 pain sites for the IASP, Donovan, and Tunks classification method, respectively).
Results
Table 4 displays the demographic and medical characteristics of the sample. In general, participants were middle-aged, Caucasian, males with paraplegia and a greater than high school education. Motor vehicle accident was the most common cause of SCI, and time since onset ranged from 1–16 or more years.
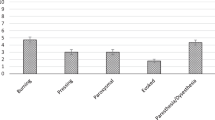
Tables 5, 6 and 7 give the proportion of individuals who reported ‘mild’, ‘moderate’, and ‘severe’ for each verbal descriptor for the three most common pain types within each classification scheme. It should be noted that all of the verbal descriptors were used at least once for each pain type, thus a mutually exclusive set of descriptors did not emerge for any of the pain classification schemes. Chi-square analysis using each classification scheme to examine the proportion of endorsement (ie, none, mild, moderate, severe) for each verbal descriptor across the three most common pain types indicated relatively few significant differences. More specifically, two verbal descriptors, ‘punishing’ and ‘tingling’, were significantly different, P<0.05, using the IASP model, and only one word was significantly different using the Donovan scheme and Tunks model (ie, ‘sickening’ and ‘tingling’, respectively). As may be expected then, ANOVAs using pain type (three most common types for each classification scheme) as the independent grouping factor showed no significant differences, P>0.05, for the SF-MPQ – Total and subscale scores, as well as no significant differences for the mean number of words endorsed on the SF-MPQ total scale and subscales. There were two exceptions to this general finding in that the number of words endorsed on the SF-MPQ – affective scale was significantly different across pain types on the IASP and Donovan classification schemes. More specifically, neuropathic at lesion level pain on the IASP, and segmental nerve pain on the Donovan scheme were associated with endorsement of a greater number of words on the affective scale (‘sickening’, ‘fearful’, ‘punishing’ and ‘tiring-exhausting’).
Discriminant function analysis was performed to determine if a linear combination of verbal descriptors would distinguish between the three most common pain types within each classification scheme. Initial analyses using each classification scheme were performed to ensure adequate compliance with the major assumptions of discriminant function analysis. The skewness statistic for each pain type was well within the normal range (−1.5 to 1.5) for all verbal descriptors. The kurtosis statistic for each verbal descriptor was in the normal range (−1.5 to 1.5) for the IASP model, however, the Donovan and Tunks models had five words that were somewhat outside of this range including ‘sickening’, ‘fearful’, ‘punishing-cruel’, and ‘throbbing’. All of these, with the exception of ‘sickening’, showed a negative kurtosis within an acceptable range of −1.5 to −2.0. Bi-variate correlations between the predictor variables (ie, verbal descriptor scores) were generally in the low range (r=0.000 to 0.63; average=0.24) suggesting little redundancy across predictors. The Box's M test was nonsignificant, P>0.05, for each classification scheme suggesting equal variance – covariance of predictors across pain types.
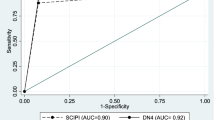
Using the IASP model, only one verbal descriptor, ‘punishing-cruel’, entered into the step-wise discriminant function analysis. Examination of the correlations between the canonical variable of the first, and only, function, and the ‘punishing-cruel’ verbal descriptor indicated an increased likelihood of being classified with ‘nociceptive musculoskeletal’ or ‘neuropathic at lesion level’ pain. Correct classification using the ‘Leave One Out’ jackknife procedure ranged between 64% to 79% (note: only two groups are classified with only one function).
Using the Donovan scheme, four verbal descriptors, ‘sickening’, ‘aching’, ‘tingling’, and ‘tiring’, entered the step-wise discriminant function analysis. The greatest separation in group centroid means was found between mechanical pain, vs the other two pain types (ie, segmental/caudal equina, and spinal cord). Examination of the eigenvalues indicated that the first and second function accounted for 73% and 27% of the variance, respectively. A Chi-square transformation of Wilks Lamda was used to test whether the group means (ie, group centroids for each canonical variable) for each function were significantly different. Results showed that the group means on the first and second discriminant functions were significantly different, P<0.01, indicating the predictive importance of both functions. Examination of significant correlations (r>0.4) between the canonical variable of the first function, and scores of the verbal descriptors indicated an inverse relationship with ‘aching’ (r=−0.41), and a positive correlation (r=0.52) with ‘tingling’. Thus, spinal cord and segmental/cauda equina pain tended to be associated with a ‘tingling’, but not an ‘aching’ sensation, and the reverse was true for mechanical pain. The second function primarily separated segmental/cauda equina pain, from mechanical and spinal cord pain. The verbal descriptors ‘sickening’ (r=0.86), ‘tiring’ (r=0.50), and ‘aching’ (r=0.55) tended to be associated with an increased likelihood of being classified with segmental/cauda equina pain. The classification rates using the ‘Leave One Out’ jackknife procedure were low, ranging from 50% to 63%.
Using the Tunks scheme, three verbal descriptors, ‘sickening’, ‘aching’, and ‘tingling’ entered the step-wise discriminant function analysis. The greatest separation in group centroid means was found between above level myofascial pain, vs two other pain types (ie, below lesion burning and at lesion level radicular). Examination of the eigenvalues indicated that the first and second function accounted for 80% and 20% of the variance, respectively. A Chi-square transformation of Wilks Lamda was used to test whether the group means (ie, group centroids for each canonical variable) for each function were significantly different. Results showed that the group means on the first and second discriminant functions were significantly different, P<0.05, indicating the predictive importance of both functions. Examination of significant correlations (r>0.4) between the canonical variable of the first function, and scores of the verbal descriptors indicated a positive relationship with ‘tingling’ and ‘sickening’ (r's=0.63 and 0.49). Thus, below lesion burning and at lesion level radicular pain tended to be associated with ‘tingling’ and ‘sickening’ sensations, and the reverse was true for myofascial pain. The second function primarily separated below level burning pain, from myofascial and at lesion level radicular pain. The verbal descriptors ‘aching’ (r=0.88) tended to be associated with an increased likelihood of being classified with myofascial or at lesion level radicular pain. The classification rates using the ‘Leave One Out’ jackknife procedure were low, ranging from 39% to 82%.
Discussion
The use of verbal descriptors by individuals to communicate their pain state is clearly a common phenomenon. Moreover, verbal labels show good correspondence to laboratory-induced graded physical pain stimuli,56,57 and generally tend to reliably cluster into the three primary components (ie, sensory, affective, evaluative).58 Indeed, verbal descriptors are common criteria used by most classification schemes to categorize pain following SCI. Unfortunately, the validity of verbal descriptors alone to distinguish between pain types following SCI has yet to be established. Therefore, the primary aim of the current study was to evaluate the utility of verbal descriptors to distinguish between different types of pain following SCI. A secondary aim was to address two important methodological limitations of previous research examining the predictive validity of verbal descriptors. More specifically, three separate classification schemes were used to determine pain type, thus, providing for comparisons of results across classification schemes. In addition, participants were allowed to report multiple, qualitatively different, pain sites serving to ensure that the verbal descriptors reported related to the pain type of interest.
Using univariate statistical methods, a consistent pattern of results emerged that showed substantial overlap in the use of verbal descriptors across pain types. Moreover, all three pain classification schemes showed the same general pattern of results suggesting that the poor predictive validity of verbal descriptors, considered on a univariate basis, is not limited to a specific pain classification scheme. In fact, none of the verbal descriptors were found to be specific to a particular type of pain for any of the pain classification schemes. That is, every verbal descriptor was endorsed at least 8% of the time for each of the three most common pain types across classification schemes (note: one exception; none of the participants endorsed ‘sickening’ for Tunks' myofascial pain). Even when considering endorsement only within the ‘moderate to severe’ intensity range, there was considerable overlap across the three most common pain types for each verbal descriptor. Consistent with this finding, a recent meta-analysis showed that 12 of the 15 words on the SF-MPQ were selected by greater than 20% of subjects across a variety of pain populations.33 Taken together, there does not appear to be a pathognomic verbal descriptor that can be used to identify a specific SCI pain type.
Similar results emerged when considering combinations of verbal descriptors. For instance, none of the classification schemes showed significant means differences across pain types on the various scores associated with the SF-MPQ (ie, total and subscale scores). Nor were significant differences found across pain types when considering the number of words endorsed on the various SF-MPQ scales. Given the considerable overlap in the use of verbal descriptors across pain types, the proportion of individuals that could be accurately classified using multivariate discriminant function analysis was limited. Indeed, the overwhelming majority of verbal descriptors did not enter into the discriminant function model using a step-wise procedure. In terms of consistency across the three classification schemes, a common verbal descriptor that emerged on all three step-wise discriminant functions was not found. Three verbal descriptors, ‘tingling’, ‘aching’, and ‘sickening’, were found to be common across two of the three discriminant function analyses. In general, ‘aching’ tended to be associated with mechanical pain, and ‘tingling’ and ‘sickening’ tended to be associated with neuropathic pain. This finding is consistent with the review of SCI pain classification literature which indicated 78% of the classification schemes considered the word ‘aching’ to be characteristic of mechanical pain, whereas 54% of the classification schemes used the word ‘tingling’ to describe neuropathic pain.
As may be expected given the substantial overlap in the use of verbal descriptors across pain types, a low rate of correct classification was found using the discriminant functions. That is, between 39% to 82% of the pain sites were correctly classified using verbal descriptors. On average, 60% of the pain sites were correctly classified. Thus, the discriminant function models were able to correctly classify pain types at about 30% above what would be expected based on chance alone (ie, the three most common pain types used for analysis, thus, a 33% change rate). Taken together, results suggest that the use of verbal descriptors alone to distinguish between pain types following SCI may be limited. This is particularly true since the methodology of the current study was designed to maximize the predictive validity of verbal descriptors. That is, by excluding other classification criteria (eg, pain duration, time of onset, aggravating factors) from the discriminant model, the amount of shared explanatory variance with other classification criteria was arbitrarily attributed to verbal descriptors.
Although the results of the current study showed minimal support for the use of verbal descriptors as a mechanism to classify SCI pain, there are several methodological concerns within this area of research that limit firm conclusions. Most importantly, it is difficult to determine whether the poor results of the current study should be attributed to the limited predictive validity of verbal descriptors, or to ‘inaccurate’ classification of pain types. Both sides of this equation will need to be clarified in future research so that the use of verbal descriptors, or any other classification criteria, as a mechanism to classify pain can be more specifically determined. On the verbal descriptor side of the equation, Bennett47 discussed several factors that may limit the predictive validity of verbal descriptors including the (1) exclusion of important descriptors for a given pain type, (2) psychometric scaling properties of each descriptor (eg, a restricted range of scores associated with each descriptor, reading level requirements), (3) method of assessment (eg, restricting endorsement to the two or three most important verbal descriptors, vs allowing endorsement of all verbal descriptors associated with a pain site), and (4) the assessment time frame of reference (eg, current pain vs ‘over the past week’). In addition to further clarification of these issues, this area of research would benefit from the establishment of a standard set of verbal descriptors with validated psychometric properties for pain site assessment. Standardization would facilitate comparisons across studies and also allow for the development of pattern analysis across pain populations.
On the pain classification side of the equation, a gold-standard has not emerged. Indeed, there are 29 published classification schemes for pain following SCI. Thus, it has yet to be determined if these results generalize across the various classification schemes. It should be noted, however, that we selected three of the most common classification schemes for study and the results were generally the same across all three classification schemes. In addition to establishing a general consensus for the classification of pain following SCI, the psychometric properties (eg, reliability) and the relative importance of the various classification criteria (eg, location, mitigating factors) have yet to be determined. Along these lines, we are currently examining the psychometric characteristics (eg, inter-rater agreement, the importance of clinician experience in pain rating) of the three classification schemes used in the current study. For instance, three independent raters classified pain sites using the Donovan scheme.53 Inter-rater agreement for pain type was found to range from about 50% to 70%. Moreover, inter-rater agreement did not improve as additional classification criteria were provided.
Ideally, future research in pain classification would benefit from the collection of an extensive set of classification criteria (eg, location, time of onset, verbal descriptors, mitigating factors) which would be used to determine pain type based on several different classification schemes. With this information, a systematic approach, through the use of discriminant function analysis, could be used to determine the relative importance and incremental predictive validity of each criterion, and consistency of results could be compared across classification schemes. In addition, cluster analysis could be used to identify patterns in predictor variables that may be used to classify pain types independent of an underlying classification scheme. Given the inconsistency in pain classification, procedures used to classify pain should be clearly presented including measures taken to ensure participants describe the pain type of interest.
Limitations
There are some important limitations to the current study to consider. First, there may be regional, national, and/or variation in the use of verbal pain descriptors. The sample in the current study consisted of individuals in the Southeastern United States. Thus, the extent to which these findings may vary across other regions or nations is not known. Second, there is evidence to suggest that both the total number of verbal descriptors endorsed and their associated pain intensity ratings, are positively correlated with self-reported psychiatric symptoms (ie, the ‘diffusion hypothesis’).46,59 Participants in the current study were not screened for psychiatric symptoms. Thus, it is unknown whether the extent of overlap in the use of verbal descriptors across pain types may have been over-estimated secondary to psychiatric symptomotology. Third, although our procedures allowed participants to report multiple pain sites so that more specific attributions could be made between verbal descriptors and pain types, it resulted in a lack independence between verbal descriptor endorsement and pain type. More specifically, the McGill Pain Questionnaire was completed for each pain site, and each pain site was subsequently categorized into the appropriate pain type group. Because an individual was allowed to report multiple pain sites, an individual may have been used in more than one pain type group. To the extent that an individual employs a common vocabulary to describe pain that is independent of pain type, the amount of overlap in the use of verbal descriptors across pain types may have been over-estimated. About 80% of the sample reported two or more pain sites. Lastly, the criteria used to classify pain types with the Donovan pain rating scheme and the verbal descriptors used for the study were confounded. More specifically, all three classification schemes employed the use of verbal descriptors that were, in turn, used to predict pain type. Therefore, the amount of explained variance attributable to the verbal descriptors was likely over-estimated. Since accurate classification of pain type based on verbal descriptors was found to be marginal even given this confound, the limited utility of current verbal descriptor scales to classify pain types following SCI can be reasonably asserted.
References
Putzke JD, Richards JS, Hicken BL, DeVivo MJ . Pain following spinal cord injury: Important predictors and impact on quality of life Pain 2001 in press
Siddall PJ et al. Pain report and the relationship of pain to physical factors in the first 6 months following spinal cord injury Pain 1999 81: 187–197
Demirel G, Yllmaz H, Gencosmanoglu B, Kesiktas N . Pain following spinal cord injury Spinal Cord 1998 36: 25–28
Anson CA, Shepherd C . Incidence of secondary complications in spinal cord injury International J Rehab Res 1996 19: 55–66
Johnson RL et al. Secondary conditions following spinal cord injury in a population-based sample Spinal Cord 1998 36: 45–50
Anke AG, Stenehjem AE, Stanghelle JK . Pain and life quality within 2 years of spinal cord injury Paraplegia 1995 33: 555–559
Bedbrook GM . Pain in paraplegia and tetraplegia In: Bedbrook GM (ed) Lifetime Care of the Paraplegic patient New York: Churchill Livingstone 1985 pp 245–248
Beric A . Post-spinal cord injury pain states Anesthesiology Clinics of North America 1997 15: 445–463
Bonica JJ . Introduction: Semantic, epidemiologic, and educational issues In: Casey KL, (ed) Pain and Central Nervous System Disease: The Central Pain Syndromes New York: Raven Press, Ltd 1991 pp 13–29
Britell CW, Mariano AJ . Chronic pain in spinal cord injury Phys Med Rehab 1991 5: 71–82
Bryce TN, Ragnarsson KT . Pain after spinal cord injury Physical Medicine & Rehabilitation Clinics of North America 2000 11: 157–168
Burke DC . Pain in paraplegia Paraplegia 1973 10: 297–313
Christensen MD, Hujsebosch CE . Chronic central pain after spinal cord injury J Neurotrauma 1997 14: 517–537
Davis L, Martin J . Studies upon spinal cord injuries. II. The nature and treatment of pain J Neurosurg 1947 4: 483–491
Davis L . Treatment of spinal cord injuries Arch Surg 1954 4: 488–495
Davis R . Pain and suffering following spinal cord injury Clin Orthop 1975 76–80
Donovan WH, Dimitrijevic MR, Dahm L, Dimitrijevic M . Neurophysiological approaches to chronic pain following spinal cord injury Paraplegia 1982 20: 135–146
Freeman LW, Heimburger RF . Surgical relief of pain in paraplegic patients Arch Surg 1947 55: 433–440
Frisbie JH, Aguilera EJ . Chronic pain after spinal cord injury: an expedient diagnostic approach Paraplegia 1990 28: 460–465
Hohmann GW . Psychological aspects of treatment and rehabilitation of the spinal cord injured person Clin Orthop 1975 81–88
Kaplan LI, Grynbaum BB, Lloyd E, Rusk HA . Pain and spasticity in patients with spinal cord dysfunction JAMA 1962 182: 918–925
Krueger EG . Management of painful states in injuries of the spinal cord and cauda equina Am J Phys Med 1960 39: 103–110
Melzack R, Loeser JD . Phantom body pain in paraplegics: evidence for a central ‘‘pattern generating mechanism’’ for pain Pain 1978 4: 195–210
Michaelis LS . The problem of pain in paraplegia and tetraplegia Bull NY Acad Med 1970 46: 88–96
Nashold Jr BS . Paraplegia and pain In: Nashold Jr BS, Ovelmen-Levitt J, (ed) Deafferentation Pain Syndromes: pathophysiology and Treatment New York: Raven Press, Ltd 1991 pp 301–319
Pollock LJ et al. Pain below the level of injury of the spinal cord Arch Neurol 1951 65: 319–322
Segatore M . Understanding chronic pain after spinal cord injury J Neurosci Nurs 1994 26: 230–236
Siddall PJ, Taylor DA, Cousins MJ . Classification of pain following spinal cord injury Spinal Cord 1997 35: 69–75
Sidall PJ, Yezierski RP, Loeser JD . Pain following spinal cord injury: Clinical features, prevalence, and taxonomy IASP Newsletter 2000 3: 3–7
Tunks E . Pain in spinal cord injured patients In: Bloch RF, Basbaum M, (ed) Management of Spinal Cord Injuries Baltimore, MD: Williams and Wilkins 1986 pp 180–211
Woolsey RM . Chronic pain following spinal cord injury J Am Parapleg Soc 1986 9: 39–41
Guttmann L . Spinal cord injuries: Comprehensive management and research Oxford: Blackwell Scientific 1973 pp 280–305
Wilkie DJ et al. Use of the McGill Pain Questionnaire to measure pain: a meta-analysis Nurs Res 1990 39: 36–41
Chen AC, Treede RD . The McGill Pain Questionnaire in the assessment of phasic and tonic experimental pain: behavioral evaluation of the ‘pain inhibiting pain’ effect Pain 1985 22: 67–79
Dubuisson D, Melzack R . Classification of clinical pain descriptions by multiple group discriminant analysis Experimental Neurology 1976 51: 480–487
Mauro G, Tagliaferro G, Montini M, Zanolla L . Diffusion model of pain language and quality of life in orofacial pain patients Journal of Orofacial Pain 2001 15: 36–46
Melzack R . The short-form McGill Pain Questionnaire Pain 1987 30: 191–197
Turp JC, Kowalski CJ, Stohler CS . Pain descriptors characteristic of persistent facial pain J Orofacial Pain 1997 11: 285–290
Wagstaff S, Smith OV, Wood PH . Verbal pain descriptors used by patients with arthritis Ann Rheum Dis 1985 44: 262–265
Agnew DC, Merskey H . Words of chronic pain Pain 1976 2: 73–81
Grushka M, Sessle BJ . Applicability of the McGill Pain Questionnaire to the differentiation of ‘toothache’ pain Pain 1984 19: 49–57
Haefner HK et al. Use of the McGill Pain Questionnaire to compare women with vulvar pain, pelvic pain and headaches J Reprod Med 2000 45: 665–671
Jerome A et al. Cluster headache pain vs. other vascular headache pain: differences revealed with two approaches to the McGill Pain Questionnaire Pain 1988 34: 35–42
Melzack R, Terrence C, Fromm G, Amsel R . Trigeminal neuralgia and atypical facial pain: use of the McGill Pain questionnaire for discrimination and diagnosis Pain 1986 27: 297–302
Mongini F, Italiano M, Raviola F, Mossolov A . The McGill Pain Questionnaire in patients with TMJ pain and with facial pain as a somatoform disorder J Craniomandibul Pract 2000 18: 249–256
Atkinson JH, Kremer EF, Ignelzi RJ . Diffusion of pain language with affective disturbance confounds differential diagnosis Pain 1982 12: 375–384
Bennett MI . The McGill Pain Questionnaire as an exploratory instrument in discriminant analyses of pain description - Limitations in a pain clinic Pain Clinic 1996 9: 311–318
Charter RA et al. The nature of arthritis pain Br J Rheum 1985 24: 53–60
Hunter M . The Headache Scale: a new approach to the assessment of headache pain based on pain descriptions Pain 1983 16: 361–373
Nehemkis AM, Charter RA . The limits of verbal pain descriptors Perceptual & Motor Skills 1984 59: 251–254
Nehemkis AM, Charter RA . Comparison of arthritis and cancer pain patients: are distinct clinical pain syndromes definable using the McGill Pain Questionnaire? Percept Mot Skills 1984 58: 126
Roche PA, Oei TPS, Heim HM . Pain in prostate cancer patients with and without metastases Pain Clinic 1997 10: 9–17
Richards JS et al. Inter-rater Reliability of the Donovan Spinal Cord Injury Pain Classification Scheme Arch Phys Med Rehab 2001 in press
Dudgeon D, Raubertas RF, Rosenthal SN . The short-form McGill Pain Questionnaire in chronic cancer pain J Pain Symptom Manage 1993 8: 191–195
Katz J, Melzack R . Measurement of pain Surg Clin North Am 1999 79: 231–252
Klepac RK, Dowling J, Hauge G . Sensitivity of the McGill Pain Questionnaire to intensity and quality of laboratory pain Pain 1981 10: 199–207
Janal MN . Concerning the homology of painful experiences and pain descriptors: a multidimensional scaling analysis Pain 1996 64: 373–378
Lowe NK, Walker SN, MacCallum RC . Confirming the theoretical structure of the McGill Pain Questionnaire in acute clinical pain Pain 1991 46: 53–60
Sist TC et al. The relationship between depression and pain language in cancer and chronic non-cancer pain patients J Pain Symptom Manag 1998 15: 350–358
Acknowledgements
Resources for the production of this manuscript were provided by the University of Alabama at Birmingham from the National Institute of Child Health and Human Development, National Institute of Health, Washington, DC, #5 T32 HD7420-10 and via a Rehabilitation Research Training Center grant from the National Institute on Disability and Rehabilitation Research, Office of Special Education and Rehabilitation Services, Department of Education, Washington, DC, #H133B980016-00.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Putzke, J., Richards, J., Hicken, B. et al. Pain classification following spinal cord injury: The utility of verbal descriptors. Spinal Cord 40, 118–127 (2002). https://doi.org/10.1038/sj.sc.3101269
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101269
Keywords
This article is cited by
-
Dopaminergic treatment of restless legs syndrome in spinal cord injury patients with neuropathic pain
Spinal Cord Series and Cases (2016)
-
Management of Neuropathic Pain Associated with Spinal Cord Injury
Pain and Therapy (2015)
-
Screening for neuropathic pain after spinal cord injury with the Spinal Cord Injury Pain Instrument (SCIPI): a preliminary validation study
Spinal Cord (2014)
-
The effect of low-frequency TENS in the treatment of neuropathic pain in patients with spinal cord injury
Spinal Cord (2013)
-
International Spinal Cord Injury Pain Classification: part I. Background and description
Spinal Cord (2012)