Abstract
Study design
Cross-sectional.
Objectives
To assess the reliability and validity of the French version of the Spinal Cord Injury Pain Instrument (SCIPI) and to determine its performance versus “Douleur Neuropathique 4 questions” (DN4) in diagnosing neuropathic pain (NeuP).
Setting
Clinique romande de réadaptation, spinal cord injury (SCI) center in the French-speaking part of Switzerland.
Methods
Backward and forward translation in French of the 4-item SCIPI were performed by native speakers in both languages. Thirty persons with SCI were included in the validation study. Internal consistency was measured with the Kuder-Richardson (KR-20) coefficient. Cohen’s kappa coefficients were used to assess the test–retest reliability and the agreement between SCIPI and DN4. Clinical assessment was used as the reference standard to diagnose NeuP. The area under the receiver operator characteristics curve (AUROC) was used to assess the performance of diagnostic tests.
Results
KR-20 coefficient of internal consistency was 0.50 (95% CI 0.26, 0.74). Test–retest reliability coefficient was 0.86 (95% CI 0.76, 0.95). The best cutoff value was 2 points, resulting a sensitivity of 88% (95% CI 69%, 98%) and a specificity of 92% (95% CI 75%, 99%). SCIPI had an AUROC of 0.90 (95% CI 0.82, 0.98), which was not significantly lower than the AUROC for DN4, 0.92 (95% CI 0.85, 0.99, p = 0.56). Agreement between SCIPI and DN4 was of 0.88 (95% CI 0.77, 1.00).
Conclusion
The French version of the SCIPI is a reliable and valid tool that can identify the presence of NeuP in an individual with SCI.
Similar content being viewed by others
Introduction
Pain is one of the major secondary conditions experienced by people with spinal cord injury (SCI), with 60 to 80% of them referring some pain [1,2,3,4,5]. Pain classification is a complex task. The International SCI Pain group updated in 2012 the SCI pain taxonomy and proposed a standardized classification with pain type and subtype, defining four categories: nociceptive pain (subtype: musculoskeletal, visceral, other), neuropathic pain (NeuP) (subtype: at-level, below-level, other), other pain and unknown pain [6, 7].
To efficiently manage pain, it is of great importance to diagnose adequately pain types. NeuP, defined by the International Association for the Study of Pain as “pain caused by a lesion or disease of the somatosensory nervous system” [8] is a very common health condition post-SCI. The systematic review and meta-analysis of Burke et al. reported a pool point prevalence of 53% [9].
Assessment methods of NeuP vary across studies. Several questionnaires [10] have been developed to differentiate NeuP from non-neuropathic pain (NNeuP) and thus to assist clinicians to identify individuals with NeuP. The “Douleur Neuropathique 4 questions” (DN4) [11] is one of the validated questionnaires that is commonly used in daily practice. It was developed in 2005 by the French NeuP Group to discriminate NeuP on a population presenting pain associated with a definite neurological or somatic lesion. This 10-item questionnaire includes both sensory descriptors (7 items) and sensory examination (3 items). The DN4 has been used only sparsely in the SCI population.
In 2014, Bryce et al. [12] developed the Spinal Cord Injury Pain Instrument (SCIPI), a screening tool for NeuP specifically validated in the SCI population. Composed originally of seven items, it was reduced to four items. There is no clinical examination part so it can be administrated by non-clinicians and can be used on self-report basis or interview. Recently, the German version of the SCIPI has been validated in terms of screening performance compared to the painDETECT questionnaire and to the International Association for the Study of Pain grading system [13]. However, data related to the construct’s properties such as internal consistency, test–retest reliability have not been investigated. Whether the screening performance of SCIPI is comparable to the DN4 is questionable. In addition, there is no current validated French version of the SCIPI.
The main objective of this study was to assess the reliability and validity of the French version of the 4-item SCIPI questionnaire and to determine its performance versus DN4 in diagnosing NeuP.
Methods
This study was conducted at the Clinique romande de réadaptation Suva in Sion (Switzerland), the specialized SCI unit in the French-speaking part of Switzerland. Before enrollment, written informed consent was obtained individually from all participants. The regional medical ethics committee (CER-VD) was contacted, and prior approval was not required for this study. All procedures complied with Declaration of Helsinki and its subsequent amendments.
The first part of the study consisted of the translation and cross-cultural adaptation of the SCIPI in French, whereas the second part consisted of the validation process.
Cross-cultural adaptation
Before the adaptation of the questionnaire, we obtained the permission for translation and validation in French from the developers [12]. The translation was performed using a multistep approach as advised by the current guidelines [14, 15]. Six steps were performed. (1) A forward translation from English to French by two native French speakers who were fluent in English was realized. One was informed of the concept being covered by the questionnaire and had a clinical background; the other was not informed about the objective of the study and was considered as “naïve”. (2) A synthesis of the two translations was realized by an expert panel of three persons to resolve any discrepancies. The 1st version of the French SCIPI was formulated. (3) The back translation from French to English was realized by two native English speakers fluent in French and considered as “naïve”. (4) A consensus meeting with an expert committee took place. The objective was to compare the original English version with the back-translated versions and to address any discrepancies. Finally, the first French version was refined and a prefinal French version was obtained. (5) This new version was administrated to a convenience sample of five French-speaking persons with SCI. They were asked to make commentaries on the meaning of each item, any difficulties encountered, ambiguity, and comprehension. (6) Finally, a definitive French version was validated during a new consensus meeting.
Validation study
Thirty individuals with SCI were included in the study. Inclusion criteria were as follow: adult participant with a traumatic or non-traumatic SCI suffering from pain that persisted over 1 week. Exclusion criteria were: other neurological diagnoses and insufficient French language skills.
Each person was asked to rate his pain severity on a numerical rating scale, with 0 = no pain and 10 = worst pain imaginable. This was done for the three worst pain sites, characterized by anatomical location, the person reported. The SCIPI and DN4 questionnaires were administered in a random order. For the test–retest reliability, the persons were assessed a second time, 2–3 days later, with the SCIPI questionnaire.
Clinical pain classification in NeuP or NNeuP is realized as a clinical routine in the center. It was carried out either by a SCI specialized physician or by a nurse specialized in pain management and was reported in the medical record. In some cases, in addition to the physical examination, complementary exams, such as evoked potential test, electromyography, or magnetic resonance imaging, were performed to confirm the diagnosis.
Questionnaires
The original English version of the 4-item SCIPI questionnaire is a sensitive and specific screening tool for differentiating NeuP and NNeuP pain in SCI individuals. A score of 1 is given to each positive answer and a score of 0 to each negative answer. The total score is calculated as the sum of the 4 items. A cutoff score of 2, to identify NeuP, appears to have good sensitivity, 73%, and specificity, 78% [12].
The DN4 questionnaire is composed of ten items. A score of 1 is given to each positive answer and a score of 0 to each negative answer. The total score is calculated as the sum of the items. A cutoff score of 4 gives a sensitivity of 83%, a specificity of 90%, and an accuracy of 86% [11].
Statistics
Categorical variables (gender, cause of injury, American Spinal Injury Association (ASIA) impairment scale, level of injury, number of pain sites) were presented using number and percentage. Continuous variables with normal distributions (age, pain intensity) were presented using mean and standard deviation. Continuous variable with non-normal distribution (time since injury) was presented using median, 25 and 75% percentiles.
The internal consistency of SCIPI and DN4 was assessed using Kuder-Richardson coefficient (KR-20) and Cronbach’s alpha, respectively. Values can range from 0 (no internal consistency) to 1 (perfect internal consistency).
Cohen’s kappa coefficients were used to assess the test–retest reliability of SCIPI, as well as the agreement between SCIPI and DN4. Interpretation of those coefficients was as follow: <0.20 = poor, 0.21 to 0.40: fair, 0.41 to 0.60 = moderate, 0.61 to 0.80 = good and 0.81 to 1 = almost perfect [16].
A principal component analysis was applied to inspect the underlying structure of the SCIPI questionnaire. Eigenvalues from the initial, unrotated solution were inspected. To help determine the number of components, we set the minimum value of eigenvalues to be retained to 1. A component consists of a vector of numerical values between −1 and 1, referred as loading factor. The overall Kaiser–Meyer–Olkin measure of sampling adequacy was also examined, which acceptable value is considered as above of 0.5 [17].
The clinical assessment was used as the reference standard to diagnose NeuP. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of the SCIPI and DN4 (cutoff 4 points) were expressed as proportions with 95% confidence intervals (CI) using the exact binomial distribution.
Receiver operating characteristic (ROC) curves were drawn with clinical assessment as outcome variable and the two screening questionnaires (SCIPI, DN4) as the classifier variables. The overall diagnostic performance of screening tests was expressed by the ROC area under the curve (AUROC) with the estimation of the 95% CI. The null hypothesis of equal test performance was tested by comparing AUROCs of the two types of diagnostic questionnaires (reject the null hypothesis at P < 0.05).
All statistical tests were performed using STATA 16.0 for Windows (Stata Corporation, College Station, Texas, US).
Results
Cross-cultural adaptation
We encountered some difficulties for the English to French translation related to grammatical and comprehension aspects. For example, by literally translating the questions, we observed that while we were waiting for a “yes” or “no” answer, the response was either pins and needles or tingling. We therefore decided to privilege the conceptual rather than literal translation. For the back translation to English, we also put emphasis on conceptual and cultural equivalence. We tested the prefinal French version of SCIPI on 5 French-speaking persons with SCI, whose characteristics are defined in Table 1. Two of them made commentaries and suggested to modify terms for reasons of comprehension. The final version of the French SCIPI questionnaire is presented in Table 2.
Validation study
Thirty participants with SCI and pain were included. Their demographic and clinical characteristics are presented in Table 1. They reported a total of 54 pain sites distributed as follow: lower limb (35%), upper limb (33%), and trunk (32%). Clinical diagnosis of NeuP or NNeuP was available for 51 pain sites. In three situations, the uncertainty was too high to accurately define the pain type. Classification between NeuP and NNeuP was distributed as follow, 25 pain sites (49%) were considered as NeuP and 26 (51%) as NNeuP. Distribution of pain subtype for NP was as follow: 9 (36%) at-level, 15 (60%) below-level and 1 (4%) other neuropathic SCI pain.
Internal consistency, assessed by a KR-20 coefficient or Cronbach’s alpha, was of 0.50 (95% CI 0.26, 0.74) for SCIPI and of 0.77 (95% CI 0.41, 0.86) for DN4.
SCIPI questionnaire was administrated twice, 2.7 ± 0.7 days apart. The agreement for individual questions between both tests was high, ranging from 94.4% to 98.2% and 89% for the total score. Table 3 represents the test–retest reliability for each item. Test–retest reliability coefficient was very good with a kappa value of 0.86 (95% CI 0.76, 0.95). The third question “Does the skin over the area of pain or inside your body where the pain is located feel hot or burning or cold or freezing?” presented the lowest score (Cohen’s kappa = 0.88, 95% CI 0.77, 1.00).
The overall Kaiser–Meyer–Olkin measure of sample adequacy was 0.54, which is above the acceptable value of 0.5, confirming the suitability of our sample size for the performance of principal component analysis. Table 4 shows the eigenvalues, the variance explained by each component, and the factor loadings of each component. Most of the variance is explained by component 1 (41%) and component 2 (26%), resulting in a cumulative variance of 67%. The component 3 and 4 showed to be the least important as they explained a smaller proportion of variance and had an eigenvalue <1 (Table 4). For the component 1, the first three questions of the SCIPI showed a loading >0.5. For the component 2, the fourth question of the SCIPI showed the highest loading of 0.93 (Table 4).
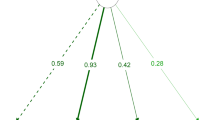
The best performance of SCIPI to distinguish NeuP from NNeuP was obtained with a cutoff point of 2. It resulted in a sensitivity of 88% (95% CI 69%, 98%), a specificity of 92% (95% CI 75%, 99%), a PPV of 92% (95% CI 73, 99%) and a NPV of 89% (95% CI 73%, 99%). The values using different cutoff points are presented in Table 5. For DN4, using the usual cutoff point of 4, the sensitivity was of 92% (95% CI 74%, 99%), the specificity of 92% (95% CI 75%, 99%), the PPV of 92% (95% CI 74%, 99%) and the NPV of 92% (95% CI 75%, 99%) (Table 5). The agreement between SCIPI and DN4 was excellent, with a value of 94.4% and a kappa coefficient of 0.88 (95% CI 0.77, 1.00, p < 0.001). The SCIPI had an AUROC of 0.90 (95% CI 0.82, 0.98), which was not significantly lower than the AUROC for the DN4 (0.92; 95% CI 0.85, 0.99; p = 0.56). Figure 1 represents the ROC curves or SCIPI and DN4.
Discussion
The purpose of this study was to realize a cross-cultural adaptation of the SCIPI for a French-speaking population with SCI. During the translation process, the emphasis was intentionally put on conceptual and cultural equivalence rather than linguistic equivalence. Under these circumstances, we could obtain a good consensus.
We demonstrated that the French version of SCIPI is a reliable instrument to discriminate between NeuP on NNeuP in a population with SCI. Moreover, it presents a good construct validity compared to clinical assessment and high agreement with the DN4 questionnaire.
SCIPI demonstrated a low internal consistency. However, it is important to notice that there is no agreement on the standard for alpha or KR-20 coefficient of reliability. A high value (>0.90) could mean item redundancy, or narrow coverage of the construct [18]. A value above 0.7 is considered acceptable [19]. The DN4 has a good internal consistency when using this threshold, but for the SCIPI, the value was considered as low. Many parameters influence the measurement and the interpretation of the coefficient, for example: the number of items or the underlying unidimensional assumptions and uncorrelated errors of all items. Bryce et al. [12] in the original version, noted also that included items are not strongly correlated with one another (except possibly items 1 and 2). The included items might not be unidimensional due to the idiosyncratic nature of pain and the underlying mechanisms that may cause NeuP. As the number of items influences the KR-20 coefficient, and the SCIPI having only 4 questions, a low coefficient is though expected for this construct.
We demonstrated a very good test–retest reliability (κ = 0.86) for the SCIPI. To our knowledge, the reliability has not been published elsewhere. Hallström and Norrbrink explored in a SCI population four other screening tools known to diagnose NeuP [20]. They found similar test–retest reliability for the Neuropathic Pain Questionnaire and the Leeds Assessment of Neuropathic Symptoms and Signs (κ = 0.89 and κ = 1, respectively).
Principal component analysis, showed two important principal components for the SCIPI questionnaire which explained 67% of the total variance of data (component 1 and 2). In addition, question 4 (pain occurs at insensate area) is quite discriminated from the first three questions concerned the pain descriptors. Previous study found one principal component explaining 46% of the total variance and all items having a loading >0.4 [12]. Differences in results between our and previous study might be explained at least by the sample size and the variations in population characteristics.
In accordance with the original version [12], we found that a cutoff ≥2 points was the most appropriate value to identify NeuP. With this value, SCIPI correctly discriminated 90% of the examined pain types (NeuP vs. NNeuP) whereas DN4 identified correctly 92% of them. Moreover, the coefficient of correlation between both questionnaires was very high (0.88) and the overall screening performance of SCIPI and DN4 (ROC AUC) was also comparable with excellent discrimination capacity. This suggests that both screening tools measure the same construct and have equivalent strong psychometric properties. Franz et al. [13] compared the German version of SCIPI to the painDETECT questionnaire, a validated self-administrated tool that addresses the quality of NeuP symptoms. They found a high correlation between both questionnaires (Spearman’s rho 0.76).
The performance of SCIPI in discriminating between NeuP and NNeuP showed to be very good, with good sensitivity (88%), specificity (92%), and high PPV and NPV values. Franz et al. [13] obtained a comparable sensitivity but lower specificity for the German SCIPI version. The sensitivity and specificity were also lower in the original English version [12]. Some methodological aspects could explain this observation. For example, in the preliminary validation study of SCIPI, participants were at least moderately depressed, which was a potential source of selection bias. Another important factor is that the sensitivity and specificity of a test often vary with the prevalence of the examined disease. Overall, the specificity tends to be lower with higher disease prevalence [21]. The prevalence of NeuP in our study was 49% compared with 63% in the previous study [12], which could explain the slightly higher specificity of our French version.
It should be noted that we expected a false negative rate of 11% by using the cutoff point of 2. If maximizing sensitivity is of importance in screening, a cutoff value of ≥1 point would be appropriate with a 100% sensitivity. We could therefore exclude a diagnosis of NeuP with certainty for those with a value of 0. However, for those with a score ≥1 point, we would need further testing to confirm the diagnosis.
The performance of SCIPI was comparable to that of DN4, but the SCIPI questionnaire is easier to perform than the DN4, which includes items that require clinical examination. SCIPI can be administered by interview or even self-report and needs less training than the DN4. Therefore, it is promising to use in low-resource settings.
The main limitation of this study is that the pain clinical examination was not realized in a standardized manner. However, it is realized as a clinical routine by experienced clinicians specialized in paraplegiology or specialized pain nurses in the SCI unit. Therefore, classification can be trusted. Moreover, the prevalence of NeuP we found (49%) is quite similar to the one obtained by Burke et al. (53%) [9].
Compared with others who studied the validity of SCIPI [12, 13], our population varies slightly. Time since injury is lower in our population, with 37% of the participants being injured within the last 6 months and we have a greater proportion of persons with incomplete lesion. It is also necessary to note that we had a smaller number of participant (n = 30) and of pain sites (n = 54) compared to the original study (n = 36 and 82, respectively) and the german validation study (n = 88 and 97, respectively) which can also affect the relatively low internal consistency we obtained.
In conclusion, The French version of the SCIPI is a reliable and valid tool that can identify the presence of NeuP in an individual with SCI and can improve the diagnosis and the management of NeuP. On a larger scale, it can also be used to estimate the prevalence of NeuP in a population with SCI and consequently, as it is a questionnaire that can be self-administrated without need of any prior physical examination, can be used in any epidemiological cohort. This questionnaire has therefore a real usefulness, for both clinical and research purposes.
Data availability
All relevant data are within the published article. Additional data are available from the corresponding author on reasonable request.
References
Brinkhof MW, Al-Khodairy A, Eriks-Hoogland I, Fekete C, Hinrichs T, Hund-Georgiadis M, et al. Health conditions in people with spinal cord injury: contemporary evidence from a population-based community survey in Switzerland. J Rehabil Med. 2016;48:197–209.
Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ. A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain. 2003;103:249–57.
van Gorp S, Kessels AG, Joosten EA, van Kleef M, Patijn J. Pain prevalence and its determinants after spinal cord injury: a systematic review. Eur J Pain. 2015;19:5–14.
Norrbrink Budh C, Lund I, Ertzgaard P, Holtz A, Hultling C, Levi R, et al. Pain in a Swedish spinal cord injury population. Clin Rehabil. 2003;17:685–90.
Ehrmann C, Reinhardt JD, Joseph C, Hasnan N, Perrouin-Verbe B, Tederko P, et al. Describing functioning in people living with spinal cord injury across 22 countries: a graphical modeling approach. Arch Phys Med Rehabil. 2020;101:2112–43.
Bryce TN, Biering-Sorensen F, Finnerup NB, Cardenas DD, Defrin R, Ivan E, et al. International Spinal Cord Injury Pain (ISCIP) Classification: Part 2. Initial validation using vignettes. Spinal Cord. 2012;50:404–12.
Bryce TN, Biering-Sorensen F, Finnerup NB, Cardenas DD, Defrin R, Lundeberg T, et al. International spinal cord injury pain classification: part I. Background and description. March 6-7, 2009. Spinal Cord. 2012;50:413–7.
Jensen TS, Baron R, Haanpaa M, Kalso E, Loeser JD, Rice ASC, et al. A new definition of neuropathic pain. Pain. 2011;152:2204–5.
Burke D, Fullen BM, Stokes D, Lennon O. Neuropathic pain prevalence following spinal cord injury: a systematic review and meta-analysis. Eur J Pain. 2017;21:29–44.
Attal N, Bouhassira D, Baron R. Diagnosis and assessment of neuropathic pain through questionnaires. Lancet Neurol. 2018;17:456–66.
Bouhassira D, Attal N, Alchaar H, Boureau F, Brochet B, Bruxelle J, et al. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain. 2005;114:29–36.
Bryce TN, Richards JS, Bombardier CH, Dijkers MP, Fann JR, Brooks L, et al. Screening for neuropathic pain after spinal cord injury with the spinal cord injury pain instrument (SCIPI): a preliminary validation study. Spinal Cord. 2014;52:407–12.
Franz S, Schuld C, Wilder-Smith EP, Heutehaus L, Lang S, Gantz S, et al. Spinal Cord Injury Pain Instrument and painDETECT questionnaire: convergent construct validity in individuals with Spinal Cord Injury. Eur J Pain. 2017;21:1642–56.
Acquadro C, Conway K, Hareendran A, Aaronson N. European regulatory I and quality of life assessment G. Literature review of methods to translate health-related quality of life questionnaires for use in multinational clinical trials. Value Health. 2008;11:509–21.
Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, et al. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value Health. 2005;8:94–104.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Field A. Discovering statistics using IBM SPSS statistics. 4th ed. London: Sage Publications; 2013.
Panayides P. Coefficient alpha: interpret with caution. Europes J Psychol. 2013;9:687–96.
Fermanian J. Validation of assessment scales in physical medicine and rehabilitation: how are psychometric properties determined? Ann Readapt Med Phys. 2005;48:281–7.
Hallstrom H, Norrbrink C. Screening tools for neuropathic pain: can they be of use in individuals with spinal cord injury? Pain. 2011;152:772–9.
Leeflang MM, Rutjes AW, Reitsma JB, Hooft L, Bossuyt PM. Variation of a test’s sensitivity and specificity with disease prevalence. CMAJ. 2013;185:E537–44.
Acknowledgements
We thank all participants who took part in this study and all people involved in the translation procedure and in the clinical pain classification. We thank also Thomas N. Bryce for permission to undertake the transcultural translation of his instrument.
Author information
Authors and Affiliations
Contributions
FR conducted the search, designed the protocol, participated in consensus meeting for the translation, screened for potentially eligible participants, acquired the data, interpreted the results and drafted the original paper. BL designed the protocol, participated in consensus meeting for the translation, revised thoroughly the paper, and approved the final version. JX designed the protocol, participated in consensus meeting for the translation, revised thoroughly the paper, and approved the final version. DHP analyzed the data, interpreted the results, participated in drafring the original paper, revised thoroughly the paper, and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
None necessary according to the regional medical ethics committee (CER-VD).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Reynard, F., Léger, B., Jordan, X. et al. Cross-cultural adaptation and validation of the French version of the Spinal Cord Injury Pain Instrument (SCIPI). Spinal Cord 60, 990–995 (2022). https://doi.org/10.1038/s41393-022-00815-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-022-00815-9