Abstract
Study design: Literature review and presentation of an experimental model of human spinal cord injury, (SCI).
Objectives: Experimental designs seek to mimic and model the physical processes by which human SCI occurs and replicate the variety of chronic pathologies that characterize its long term effects. The variations in biological processes that are present between species have contributed to recent difficulties in generalizing experimental findings to the human condition. In this review, one finds: (1) a discourse on the pathological nature of the chronic human lesion, (2) a consideration of how the physical properties of soft tissue injury result in acute and chronic changes in the spinal substance, (3) a description of a device (ESCID) that is able to replicate and dynamically monitor physical indices of SCI as they take place in experimental models, and (4) a summary of how use of this device in different species has allowed the biomechanical descriptors of such injuries to be easily compared even in murine models.
Setting: Ohio State University, Ohio, USA.
Results: Careful attention to the details of injury device design has finally allowed a direct comparison of contusion-type injury models in the rat and mouse. Biomechanical outcomes with predictive capabilities have evolved that allow the investigator to create the range of pathologies seen in the human lesion even in these small vertebrates. The predictive cytopathology and our ability to manipulate the mouse genome will allow the testing of specific hypotheses related to cause and effect in experimental spinal cord injuries. Since the biomechanics, pathology, and chronic outcomes appear to be similar to those seen in the human, these animal models should facilitate rapid progress in the design of human therapeutics.
Conclusions: Biomechanics of certain elements of experimental spinal injury are surprisingly accurate descriptors of acute and chronic pathologies in the spinal cord. This tenet applies across species and has often allowed more accurate design of clinical trials in the past few decades. As molecular approaches to this problem evolve, the use of species with known genomes appear warranted. Models that take advantage of these approaches are likely to produce innovations that quicken the pace of human trial strategies.
Similar content being viewed by others
Introduction
Human spinal cord injury (SCI) is diverse in its causes, pathology and functional consequences. The modeling of such a lesion, however, is a necessary parallel to the pursuit of clinical interventions that will interrupt the cytopathology of chronic spinal destruction. There is an extensive literature that describes the physical, anatomical and physiological sequelae of experimental SCI that spans the better part of the last century.1,2,3 In models where such information is available, the experimental biomechanical descriptors of the injury process are able to predict the subsequent acute and chronic pathophysiology of the spinal cord. Such correlations are remarkable given the complicated combination of membranes, fluid-filled spaces and soft tissue elements that are involved within the spinal compartment.4,5,6,7,8,9 It is also becoming apparent that MRI technology is improving to the degree that long term human and animal lesions can be easily assessed and compared.10,11,12 High field MRI technology in the future will allow better tissue resolution so that specific aspects of lesion pathology can be assessed to explain functional outcomes. An appreciation and utilization of such approaches will surely avoid current tendencies to explain much of the human lesion and its consequences by examining post-mortem pathology.
In the context of recent human data, it is appropriate to reflect on the degree to which our present experimental models mimic the physical processes of the human injury and accurately reveal the variety of chronic pathologies and outcomes seen in human lesions.13 As the pattern of molecular mechanisms that contribute to the pathophysiology of SCI are revealed in our animal models, a closer examination of the correspondence between injury biomechanics, tissue pathology, physiological predictors and neurological evaluation is necessary. In this article, we examine the coincidence of the physical and biological factors in an established, predictive model of mouse spinal cord injury that mimics specific features found in a variety of human SCI pathologies. It is hoped that the genetic advantages of a murine model (eg the ability to manipulate its genome) will allow rapid dissection of the complex molecular events that promote damage and prevent functional repair of the spinal cord after contusion type spinal injury. If our experimental models are chosen and evaluated with care, such approaches should quickly translate into presumptive therapeutics in the clinical setting.
Modeling of human SCI etiology and pathology
Fast, experimental contusion type lesions seem to accurately mimic those sustained after rapid subluxation of elements of the vertebral column under a variety of conditions in the human.6,7,8,9,14 While a number of alternative experimental methods for external compression have been employed to injure the spinal cord (eg slow compression, pneumatic impaction), the acute gross appearance of the human and animal cords observed after SCI is quite similar (eg minor swelling, small hemorrhagic foci). Tissue pathology, while difficult to discern in the immediate time period, quickly evolves into a classical series of stereotypical events involving gray matter dissolution, white matter partial or complete demyelination and partial malacia followed the appearance of small cystic inclusions or large, interloculated syrinx cavities.6,7,8,9,11 However, careful analysis of the clinical histopathology reveals extensive variation of features associated with the wound healing process (eg gliosis, connective tissue deposition, sensory fiber growth, demyelination, and cyst formation).6,7,8,9 This range of evolution of the descriptive cytopathologies is mimicked in the experimental contusion lesion with various aspects of the pathologic response found in animal models ranging from carnivores to rodents.1 Recent efforts to trace and characterize affected pathways and cells outside of the immediate lesion area have expanded the concept of a `distributed lesion' and explain much of the natural history of lesion development from a neurological perspective.15 The distributed lesion in this context refers to the obvious and subtle pathophysiology of cells at locations well removed from the original lesion site that may die or be functionally affected by processes stemming from the initial physical insult. Frank transection in both animals and humans is often associated with a relative stabilization of pathological change and neurological outcomes.11 However, such injuries are encountered rarely in the clinic. Thus, it is the partial lesion injury which is most common, and is often associated with the potential for continuing pathology that may be conducive to intervention strategies (ie evolving pain syndromes). `Stabilization' of an SCI lesion must therefore be thought of as the result of continuing processes of tissue destruction, abortive repair and wound healing around the injury site.16 One exciting aspect of such repair is that plasticity of spinal elements is still possible and thus becomes the focus of recent strategies to improve locomotor capacities by extensive retraining regimens in carnivores, rodents and humans.17,18 Unique molecular strategies that take advantage of these intrinsic repair processes by supplementing positive alterations and suppressing negative ones are evolving.16,19,20,21 Yet targeting individual cellular and molecular processes is complicated by their frequently dual nature. For example, one of the long term keys to effective repair may be the control of the local immune response since compelling data now exists to suggest both positive and negative aspects of immunomodulation on functional outcome in animal models.19,20,22,23,24,25
One key to understanding the variety of immunopathologies in the human and animal models has been elucidation of specific molecular events that precipitate defined aspects of histopathology. The relative contributions of these temporal and site specific changes is now sufficiently clear to begin work targeting therapies at the molecular level.1,16 For instance, given the relative importance of destructive macrophages in the spinal lesion that are derived from blood-borne monocytes,24 it might be appropriate to block chemokine receptors which contribute to the recruitment of monocytes to the lesion site. Thus, using these conceptual approaches, the similarities between the animal and human lesions provide a means to evaluate the consequences of molecular interventions on the resulting cytopathology and functional outcomes.
We have hypothesized that the secondary pathology process is a consequence of interactions between the physical and biological conditions present at the initial time of injury. Thus, a key to this comparative process is finding ways to mimic, as closely as possible, the start of the injury process in the experimental model. The physical forces imparted to the spinal tissue are likely to differ greatly between injuries sustained by variations in impact velocity, amplitude or duration. In the case described here, we will concentrate on the description and measurement of these parameters as one injures the soft tissues of the spinal cord. The ensuing physical, biomechanical descriptors permit a clear comparison of this process across species and inevitably permit specific hypotheses to be tested in man. With these data, one can evaluate whether or not the descriptors that accurately reflect the physics of the lesion process predict the biological outcomes in a way that makes the modeling process relevant to the human lesion.
Physics and soft tissue injury
In the clinical setting, SCI is often initiated when the bone of the vertebral column impinges upon the fluid-filled dural sac and compresses its contents. While this may be rapid or slow, continuing or very transient, the key determinant of mechanical trauma is the energy transfer through the complicated system of membranes (dura, arachnoid, arachnoid trabecula, and pia) and fluid in the sub-arachnoid space (CSF) to the soft tissue of the spinal cord. Since the size of the intravertebral and subarachnoid spaces and the physical properties of the gray and white matter vary greatly, it should come as no surprise to find a wide range of consequences of even rapid trauma along the length of the neuraxis. These physical variables undoubtedly contribute to the finding that regions of the spinal cord with a small subdural space (eg cervical regions) are at most risk for contusive type SCI.26 Thus, energy transfer must be considered in any plausible model of human SCI. Likewise, the resulting consequences of stretch and strain on the cellular components of the injury site should be considered.27,28 A flexion/extension, contusive type injury that occurs most often in humans, is often over in several milliseconds thus allowing only a short period of time in which to measure these important early clues.1 The energy transfer after initial impact can be compared to a wave or pressure pulse of the type that occurs in the vascular system during rapid systolic filling. This wave travels along the spinal compartment and is continually modified by reflections, size and physical characteristics of the spinal compartment. The speed of propagation of this event in the meningeal membranes probably exceeds 4–5 meters/s so that reflected pressure waves are likely to contribute to the surface/tissue distortion associated with initial, fast vertebral movement. The subsequent parabolic movement of tissue up and down the spinal cord likely contributes to tissue damage favoring early gray matter destruction due to orientation of the gray substance and white matter pathways.29,30 In spite of these initial stresses, it is rare, even in human injuries, to see little more than small petechial hemorrhages in histological preparations of the spinal cord in the first few hours after an injury has occurred. The evolution of these processes into necrotic and apoptotic forms of cellular destruction over the first few days after injury, however, occurs in stereotypical ways suggesting that the magnitude of these early physical events likely determines the course of subsequent tissue pathology. It has been our approach, in the model described below, to directly measure these early events experimentally by controlling the passive stress/strain of the dural compartment prior to the injury and estimating the pressure pulse during the injury sequence itself. In the future, a careful analysis of these factors should also allow one to account for differences such as age, size and tissue composition in modeling the human lesion.
Since one knows a priori that variance of these physical factors would affect injury outcomes, continuous estimates of displacement and force in the spinal compartment during injury has allowed a reliable mimicking of the human lesion in a variety of species with excellent predictability of neurological outcomes.2,16,31,32,33 As one moves from carnivores to rats and inevitably to murine models, this approach also allows one also to change injuries in predictable ways using established physical parameters. Theoretically, one can estimate and compensate for the effects of changes in velocity and age-induced changes in the meningeal compartments in such models.
Injury dynamics and device design
Previous versions of the model system to be described have appeared in the literature and have proven their worth in terms of descriptive biomechanics that are predictive of injury outcomes in species from carnivores to rodents. Under the auspices of the International Spinal Research Trust, we have simplified, the design and developed the necessary device hardware and computer software to restructure a spinal injury system that has been exported to other laboratories. The ability of this system to utilize both the rat and the mouse as experimental models is of obvious importance in terms of generating and mimicking historical patterns of biomechanics thus allowing the transfer of decades of information gleaned from the rat model into the mouse. The mouse therefore can become a major focus of injury modeling in the foreseeable future.16,33,34
The basic injury device (ESCID-2000) utilizes an electromagnet to produce a rapid, single impact spinal cord contusion. The electromagnet is controlled via computer interface using commercially available hardware/software that precipitates the impact sequence. Briefly, a vertical impounder controlled by the computer interface is rapidly moved in an accurate, reproducible pattern over very short, calibrated distances (usually less than 1.0 mm) during the injury sequence. As in the rat, injury is produced in anesthetized mice after a dorsal laminectomy is performed at the T9 vertebral process. Critical steps in this process include: (1) careful stabilization of the vertebral column before injury, (2) standardized site and size of the laminectomy, and (3) reproducible dimpling of the dural surface (to achieve a 1500 dynes `touch' signal) just before injury to insure a similar starting point. The latter touch sensitivity of the shaft of the impactor before the injury also allows dynamic assessment of probe biomechanics. For example, this measure allows interpretation of whether the probe is touching nearby tissues outside the spinal envelope in the small, microscopically monitored space of the laminectomy site. The importance of these critical procedures has been discussed elsewhere.34
A simplified diagram of the injury device is included here to illustrate design principles (Figures 1 and 2). As illustrated, both touch (Figure 1B) and injury (hit, Figure 2A) signals are generated using the Labview Software (National Instruments) on a conventional PC. These signals are used to drive the probe attached to the Ling shaker via a power amplifier. A pre-adjusted mechanical stop platform arrests the probe at a displacement (between 0.3–1.5 mm) that directly determines the magnitude of injury in each animal. As the independent variable, displacement at three levels (0.3; 0.5 and 0.8 mm) produces the necessary range of injuries needed for modeling in the mouse since animals largely recover most motor control after injuries of 0.3 mm displacement while remaining severely impaired at 0.8 mm (see Ma et al33 for more details). Accurate transducers directly monitoring force and displacement at up to 8000 samples/s permit one to directly observe hit dynamics which occur over the 23 ms epoch (Figure 2B). For instance, the shape of the unrestricted force curve can be used to assess if the probe has touched adjacent tissue during its downward trajectory. The dynamic biomechanical measurements of displacement and force are then used to compute additional derived variables known to be important predictors of the injury process (eg impulse momentum, velocity of probe movement, power and energy) (Figure 3).
Diagrammatic representation of the ESCID-2000 injury device for experimental rat and mouse spinal cord contusion injury. (A) The injury device is controlled by a PC computer containing an A-D converter. The desired voltage sequence is amplified and passed to an electromagnetic shaker (Ling Dynamics, Inc.). Movement of the Shaker diaphragm causes displacement of a vertical shaft. Displacement and Force/Acceleration transducers mounted on the injury device are used to record the biomechanical parameters of impact for analysis by the investigator and storage in Ascii format. (B) The injury sequence is initiated from a point of fixed force reading from the surface of the exposed spinal cord dura. The entire injury device is lowered slowly onto the surface of the dura while monitoring the force measured from the force transducer (downward arrow). A 60 Hz oscillation of the probe in this mode allows sensitive detection of the small force measurement. Upon touching the cord surface, the force recording reverses and then increases as the pressure of the cord and meninges is imparted onto the vertical probe. For mouse injuries, a fixed starting force of 1500 dynes is applied. This force has been shown to produce no greater cellular reaction than laminectomy alone. A Stop nut is fixed on the vertical probe shaft and a Stop platform is fixed to the structure of the injury device. The distance between the Stop nut and Stop platform is carefully calibrated between 0.3 and 1.5 mm, providing the fixed displacement distance for injury
The injury sequence is controlled by the voltage output of the computer. (A) Movement of the vertical shaft by a fixed voltage sequence leads to a reproducible, single impact on the surface of the exposed dura. The hit sequence is composed of a vertical displacement, plateau, and retraction of the probe. The mechanical Stop platform (see Figure 1) facilitates a flat impact sequence. After a plateau of 12–14 ms, the probe is retracted from the surface of the dura and the subject is removed from the apparatus. (B) Immediate feedback of the displacement and force measurements is made using the computer software and stored to disk for later analysis
Measured and derived biomechanical parameters from a representative 0.5 mm displacement injury in C57Bl/6 mouse, using the ESCID-2000 (current version of the injury device). Data points were collected at the rate of 8000 s. Peak displacement occurs immediately prior to the peak force of impact. The peak impulse momentum is reached just prior to retraction of the impact probe. Future studies using this device would allow manipulation and assessment of the relationship between velocity and energy of impact on behavioral and histological parameters
The biomechanical measures obtained during the injury provide important data about the physical properties of the tissue during impact. These estimates have been examined at the completion of our experiments to assess their relative roles as predictors of injury outcomes. Each of these parameters appears to reflect slightly different aspects of the functional outcome sequelae. Thus early behavioral outcomes (day 1) are better predicted by maximum impulse/momentum while later locomotor scores correlate best with maximum displacement.33 Likewise, future analyses will determine the extent to which the various histopathological findings are predicted by the biomechanics and associated neurological recovery measures.
Relevant indices of histopathology
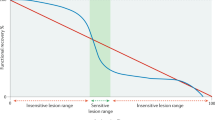
Consideration of the biomechanics of the injury process suggests that the carefully controlled contusion injury should provide the most relevant biological conditions for testing potential therapeutic interventions in clinical SCI. However, the success of our modeling objectives is determined by how reliable and predictive our outcome measures are of the clinical picture. In this regard, we have taken great pains to characterize our evaluation of the lesion histopathology in our animal models. The rat contusion injury has become widely accepted as a model of clinical SCI cases in which progressive necrosis leads to the formation of large cavities and fluid filled cysts.35,36,37,38,39,40,41,42,43 The lesion pathology can be defined in terms of such outcome measures as residual white and gray matter sparing, cavitation, and tissue shrinkage.44,45,46,47 A similar contusion of the C57Bl/6 mouse spinal cord results in the development of a dense fibrotic tissue scar at the lesion site, which more closely mimics the connective tissue scar features associated with clinical laceration and maceration injuries.6,7,8,9 A direct comparison of the chronic histopathology of the contusion lesion in these two species is thus possible using the injury device described herein. One of the most striking features of such a comparison is that the three-dimensional volume of tissue damage is very similar in topography and relative extent (Figure 4). Thus, the use of the two models in parallel will permit the direct evaluation of interventions on a wide range of relevant histopathological features that could not be fully assessed using either model alone. In addition, the development of comparable behavioral and neurophysiological outcome measures in the two species will be important for pursuing future studies with promising therapeutic strategies.
Photomicrographs of transverse sections through rat (A,C,E,G; 14 μm) and mouse (B,D,F,H; 10 μm) spinal cord tissues. Sections are stained with Luxol Fast Blue to reveal glycolipids in myelin. Horizontal scale bar in (A)=500 μm and applies to all panels from the rat. Scale bar in (B)=200 μm and applies to all mouse sections. (A,B) Midthoracic spinal cord sections from animals sustaining laminectomy only. (C–H) Sections from animals at 6 (rat) or 8 (mouse) weeks after a moderate contusion injury. Vertical scale bars in (E,F) indicate displacement from an initial starting `touch' force of 3000 dynes for rat and 1500 dynes for mouse. The epicenter was defined as the section from each section with the least LFB staining along the peripheral rim. Rostral and caudal sections were taken from the indicated distance from the epicenter. Cystic cavities in the rat injury are indicated by asterisks (*). Regions of fibrous scar tissue formation are indicated in the corresponding mouse sections by (+). Note the enlarged central canal region in both species (∧)
In recent years, the cellular and molecular tools available to neurohistologists have facilitated an explosion of information about the biological events and changes in cellular function that are initiated by SCI. To date, however, attempts to determine the role of each process in the resulting chronic histopathology have relied on mostly descriptive evaluations of staining patterns at the injury epicenter. We now understand much more of the complex environmental changes that interact in secondary pathophysiology after injury.48 It has thus become clear that the accurate evaluation of these cellular and molecular events must take into account the regional differences and temporal features of the lesion pathology. Recent progress in the visualization and quantitative analysis of histopathology in three dimensions has made such analyses feasible and useful for the complex lesion that is formed following spinal contusion injury (Figure 5). We have shown previously that distinct histopathological outcome measures can be obtained by changing the amplitude of displacement in our injury models.33,34 A similar three dimensional analysis will provide the most sensitive measure of the effects of variations in biomechanical parameters as well as genetic or pharmacological manipulations on the pathology of the chronic lesion.
Examples of three-dimensional analysis of histopathology following contusion injury in the mouse. (A) Series of serial 10 μm sections, spaced 100 μm apart to reveal the morphological features of the lesion site. Sections obtained from a specimen 9 weeks after 0.8 mm displacement injury were stained with anti-fibronectin antibody (Sigma rabbit polyclonal, 1 : 2000), and the biotinylated secondary antibody visualized with diaminobenzidine (DAB). Scale=200 μm. (B) Quantitative analysis comparing the proportional area occupied by fibronectin staining in sections distributed along the rostro-caudal axis of the lesion at 9 weeks after displacement at 0.3 mm, 0.5 mm or 0.9 mm. Bars represent mean+/−SEM for 4–8/group. Distinct differences in three dimensional lesion size are evident with the three different injury levels33. (C) Computerized three dimensional reconstruction aids visualization of the morphological characteristics of the lesion. Sections stained with antibodies raised against the CR3 receptor found on macrophages and microglia at 1 week post-injury (Mac-1; Serotec, Inc.) and the sections reconstructed using MCID imaging software (Imaging Research, St. Catharines, Ontario, CA, Canada). The computerized reconstructions permit visualization of the cellular components of the lesion as it is rotated in three dimensions and cut along different planes of section as shown
Behavior as the ultimate test of model validation
Pathological sequelae of spinal injuries inevitably affect the behavioral capacities of the organism for long periods of time after injury. Behavioral masking in animals is often a term used to explain altered capacities that are not reflected in overt pathology. The obvious advantage of the injured human patient is that we can use language to potentially overcome at least some of these masking effects. Alternatively, as suggested above, behavioral outcomes are often the result of a combination of positive and negative influences on evolving pathologies in the chronically injured patient. It is therefore somewhat surprising that our animal models in the rat and mouse show such an excellent correlation between the biomechanical injury descriptors and a range of acute and chronic behavioral trials.33,49 As our behavioral trials improve, even in the mouse model, it will be important to continue a comparison between the variety of species used as spinal cord models with the capacities seen after the human lesion so that even more effective, predictive modeling can be accomplished. Unique therapeutic strategies are likely to follow.
Summary
Careful modeling strategies have resulted in a range of animal models that mimic the great majority of pathologies seen after human spinal cord injury. In the future, present designs utilizing murine models should allow us to take advantage of the elegant capacities to alter the genome in this species. The testing of specific mechanistic hypotheses imputing the role of specific genetic loci in the acute and chronic pathology of SCI is an obvious advantage of such work. It may also allow an extension of such models into the aging population where there appears to be a need for close examination of the mechanisms of SCI. The consistent application of such models across laboratories will also result in more rapid advances in the clinical trials that will address the problem.
References
Narayan RK, Wilberger Jr JR, Povlishock JT (eds). Neurotrauma New York: McGraw-Hill 1996
Aguayo AJ et al. Spinal Cord Injury: Emerging Concepts Proceedings of an NIH Workshop Bethesda, MD, National Institutes of Health 1997
Marwah J, Dixon CE, Banik NL (eds). Traumatic CNS Injury Scottsdale: Prominent Press 2001
Kakulas BA . Pathology of spinal injuries CNS Trauma 1984 1: 117–129
Kakulas BA . The clinical neuropathology of spinal cord injury. A guide to the future Paraplegia 1987 25: 212–216
Bunge RP et al. Observations on the pathology of human spinal cord injury: A review and classification of 22 new cases with details from a study of chronic spinal cord compression with extensive focal demyelination Adv Neurol 1993 59: 75–89
Kakulas BA . A quantitative study of tissue elements in human spinal cord injuries (SCI) Annual Review, International Spinal Research Trust 1996 pp 28–33
Bunge RP, Puckett WR, Hiester ED . Observations on the pathology of several types of human spinal cord injury, with emphasis on the astrocyte response to penetrating injuries In: Seil FJ (ed) Neuronal Regeneration, Reorganization, and Repair Philadelphia: Lippincott-Raven Publishers 1997 305–315
Kakulas BA . A review of the neuropathology of human spinal cord injury with emphasis on special features J Spinal Cord Med 1999 22: 119–124
Chakeres DW et al. MR imaging of acute spinal cord trauma AJNR 1987 8: 5–10
Wang D et al. A clinical magnetic resonance imaging study of the traumatised spinal cord more than 20 years following injury Paraplegia 1996 34: 65–81
Narayana PA . Magnetic Resonance of Spinal Cord Injury In: Marwah J, Dixon CE, Banik NL (eds) Traumatic CNS Injury Scottsdale: Prominent Press 2001 138–178
Graham DI, McIntosh TK, Maxwell WL, Nicoll JAR . Recent advances in neurotrauma J Neuropathol Exp Neurol 2000 59: 641–651
Metz GAS et al. Validation of the Weight-Drop Contusion Model in Rats: A Comparative Study of Human Spinal Cord Injury J Neurotrauma 2000 17: 1–17
Beattie MS, Stokes BT, Bresnahan JC . Experimental spinal cord injury: strategies for acute and chronic intervention based on anatomic, physiologic and behavioral studies In: Stein DG, Sabel BA (eds) Pharmacologic Approaches to the Treatment of Brain and Spinal Cord Injury New York: Plenum Publishing Corp 1988 43–74
Jakeman L, Ma M, Stokes BT . Considering the use of transgenic mice in spinal cord research In: Marwah J, Dixon CE, Banik NL (eds) Traumatic CNS Injury Scottsdale: Prominent Press 2001 180–201
Barbeau H, Rossignol S . Recovery of locomotion after chronic spinalization in the adult cat Brain Res 1987 412: 84–95
Edgerton VR et al. Potential of adult mammalian lumbosacral spinal cord to execute and acquire improved locomotion in the absence of supraspinal input J Neurotrauma 1992 9: Suppl 1 S119–S128
Popovich PG, Whitacre C, Stokes BT . Is spinal cord injury an autoimmune disorder? The Neuroscientist 1998 4: 71–76
McTigue DM, Popovich PG, Jakeman LB, Stokes BT . Strategies for spinal cord injury repair Prog Brain Res 2000 128: 3–8
Ramer MS, Harper GP, Bradbury EJ . Progress in spinal cord research – a refined strategy for the International Spinal Research Trust Spinal Cord 2000 38: 449–472
Lazarov-Spiegler O et al. Transplantation of activated macrophages overcomes central nervous system regrowth failure FASEB J 1996 10: 1296–1302
Lazarov-Spiegler O, Rapalino O, Agranov G, Schwartz M . Restricted inflammatory response in the CNS: a key impediment to axonal regeneration? Mol Med Today 1998 4: 337–342
Popovich PG et al. Depletion of hematogenous macrophages promotes partial hindlimb recovery and neuroanatomical repair after experimental spinal cord injury Exp Neurol 1999 158: 351–365
Hauben E et al. Passive or Active Immunization with Myelin Basic Protein Promotes Recovery from Spinal Cord Contusion J Neurosci 2000 20: 6421–6430
Meyer PR . Spinal Cord Injury In: Young RR and Woolsey RM (eds) Diagnosis and Management of Disorders of the Spinal Cord Philadelphia: W.B. Saunders 1995 pp 103–104
Lucas JH . In vitro models of mechanical injury J Neurotrauma 1992 9: 117–120
Pike BR . Mechanical Injury to Cell and Tissue Cultures In: Marwah J, Dixon CE, Banik NL (eds) Traumatic CNS Injury Scottsdale: Prominent Press 2001 pp 204–230
Blight AR . An overview of spinal cord injury models In: Narayan RK, Wilberger JE, Povlishock JT (eds) Neurotrauma New York: McGraw Hill 1996 p 1395
Blight A . Mechanical factors in experimental spinal cord injury J Am Paraplegia Soc 1988 11: 26–34
Stokes BT, Noyes DH, Behrmann DL . An electromechanical spinal injury device with dynamic sensitivity J Neurotrauma 1992 9: 187–195
Stokes BT, Horner PJ . Spinal cord injury modeling and functional outcome assessment In: Narayan RK, Wilberger JE, Povlishock JT (eds) Neurotrauma New York: McGraw Hill 1996 pp 1395–1403
Ma M, Basso DM, Walters P, Stokes BT, Jakeman LB . Behavioral and histological outcome following graded contusion injury in C57Bl/6 mice Exp Neurol 2001 169: 239–254
Jakeman LB et al. Traumatic spinal cord injury produced by controlled contusion in mouse J Neurotrauma 2000 17: 299–319
Gale K, Kerasidis H, Wrathall JR . Spinal cord contusion in the rat: behavioral analysis of functional neurologic impairment Exp Neurol 1985 88: 123–134
Wrathall JR, Pettegrew RK, Harvey F . Spinal cord contusion in the rat: production of graded, reproducible, injury groups Exp Neurol 1985 88: 108–122
Young W . Secondary CNS injury J Neurotrauma 1988 5: 219–221
Young W . NASCIS J Neurotrauma 1990 7: 113–114
Stokes BT . Experimental spinal cord injury: a dynamic and verifiable injury device J Neurotrauma 1992 9: 129–131
Anderson TE, Stokes BT . Experimental models for spinal cord injury research: Physical and physiological considerations J Neurotrauma 1992 9: Suppl 1 S135–S142
Stokes BT, Noyes DH, Behrmann DL . An electromechanical spinal injury device with dynamic sensitivity J Neurotrauma 1992 9: 187–195
Young W . Secondary injury mechanisms in acute spinal cord injury J Emerg Med 1993 11: Suppl 1 13–22
Beattie MS et al. Endogenous repair after spinal cord contusion injuries in the rat Exp Neurol 1997 148: 453–463
Noyes DH, Bresnahan JC . Spinal cord lesion volume and impact parameters Biophys J 1981 33: 93a
Bresnahan JC, Beattie MS, Todd FD3, Noyes DH . A behavioral and anatomical analysis of spinal cord injury produced by a feedback-controlled impaction device Exp Neurol 1987 95: 548–570
Bresnahan JC, Beattie MS, Stokes BT, Conway KM . Three-dimensional computer-assisted analysis of graded contusion lesions in the spinal cord of the rat J Neurotrauma 1991 8: 91–101
Popovich PG et al. Depletion of hematogenous macrophages promotes partial hindlimb recovery and neuroanatomical repair after experimental spinal cord injury Exp Neurol 1999 158: 351–365
Zhang Z, Krebs CJ, Guth L . Experimental analysis of progressive necrosis after spinal cord trauma in the rat: etiological role of the inflammatory response Exp Neurol 1997 143: 141–152
Behrmann DL, Bresnahan JC, Beattie MS, Shah BR . Spinal cord injury produced by consistent mechanical displacement of the cord in rats: behavioral and histologic analysis J Neurotrauma 1999 9: 197–217
Acknowledgements
This work was supported by the International Spinal Research Trust (STR029) and the NIH (NS-37321).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Stokes, B., Jakeman, L. Experimental modelling of human spinal cord injury: a model that crosses the species barrier and mimics the spectrum of human cytopathology. Spinal Cord 40, 101–109 (2002). https://doi.org/10.1038/sj.sc.3101254
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101254
Keywords
This article is cited by
-
Innovative mouse model mimicking human-like features of spinal cord injury: efficacy of Docosahexaenoic acid on acute and chronic phases
Scientific Reports (2019)
-
Diffusion tensor imaging of the mouse brainstem and cervical spinal cord
Nature Protocols (2013)
-
Clinical canine spinal cord injury provides an opportunity to examine the issues in translating laboratory techniques into practical therapy
Spinal Cord (2006)
-
Neuropathology: the foundation for new treatments in spinal cord injury
Spinal Cord (2004)
-
Post-traumatic inflammation following spinal cord injury
Spinal Cord (2003)