Abstract
Congenital clefts and other developmental anomalies of the atlas vertebra are rarely encountered. They are incidental findings discovered while investigating the cervical spine following trauma. Differentiation of developmental variants of the atlas from the burst fracture of Jefferson is essential to prevent unnecessary medical intervention.
Similar content being viewed by others
Case history
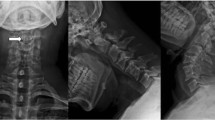
A 29-year-old snow boarder swerved to avoid a skier. He somersaulted and landed on his back. There was no history of head injury or loss of consciousness. He walked into the examination room complaining of neck pain but with no radiation of the pain to his arms or sub-occipitally. Lhermitte's sign was not reported, and neurological examination was normal. Antero-posterior and lateral cervical spine radiography down to C7/T1, including flexion/extension views, were normal. Open-mouth radiography revealed a mid-line defect in the anterior arch of the atlas (Figure 1), which raised the suspicion of a fracture. Computed tomography (CT) confirmed the presence of a congenital anterior mid-line cleft and also showed a similar mid-line cleft in the posterior arch (Figure 2). The patient was reassured and treated symptomatically with simple analgesics. On review 1 week later he was completely free of neck pain.
Discussion
Ossification of the posterior arch of the atlas begins around the seventh week of intra-uterine life in two centres of ossification, one in each half of the posterior arch. The endochondrial ossification proceeds dorsally, and fusion usually occurs around the third year of life. In about 2% of infants another ossification centre in the region of the posterior tubercle is found, uniting secondarily with the lateral processes of the arch.1,2 The anterior arch develops from one or more ossification centres, which usually appear during the first year of life. Fusion of the anterior arch to the lateral masses, to form the neurocentral synchrondrosis, normally occurs by the seventh year of life (Figure 3).3,4
Posterior mid-line clefts of the atlas, rachischisis or spina bifida occulta, are well recognised and are attributed to the defective or absent development of the cartilaginous preformation of the arch and not to a disturbance of the ossification.5 Geipel noted in 1613 dissections of the atlas that 4% had a cleft of the posterior arch; 97% of these were median clefts, while the rest were located laterally through the sulcus of the vertebral artery.6
Anterior mid-line clefts, however, are much rarer, accounting for only 0.1% in the Geipel series.6 In this case the ossification centre in the anterior arch of the atlas fails to develop. The arch is thus formed from ventral extensions of the lateral masses that fail to fuse anteriorly. These mid-line clefts are usually associated with posterior mid-line clefts, as in our patient, and are seldom found in isolation.7
Differentiation of developmental anomalies, particularly clefts of the atlas from the more common Jefferson burst fracture needs to be made as soon as possible after the suspicion is raised. This is necessary not only to allay the anxieties of the patient and medical staff, but also to commence definite management, which differs drastically between the two conditions. In the case of the mid-line clefts of the atlas, provided that ligamentous and bony injury has been excluded by appropriate imaging, definitive management is usually symptomatic with simple analgesics if necessary. With the Jefferson fracture however, treatment consists of external immobilisation of the cervical spine with a Sternal Occipital Mandibular Immobilisation (SOMI) brace or Halo fixation vest for up to 16 weeks.8
Differentiation of the developmental anomalies from burst fractures of the atlas can be made from close inspection of the lateral cervical and open-mouth radiographs and confirmed by CT. On the lateral radiograph the cortical bone of the anterior arch may be absent or indistinct when a cleft is present.7 Linear tomography may further reveal smooth corticated margins, which contrast with the sharp non-corticated appearance of a fracture. In addition, developmental anomalies may be associated with an atlanto–axial lateral offset of 1–2 mm if there are both anterior and posterior defects. This, however, does not indicate abnormal spread of the atlas and is not clinically significant. A Jefferson fracture should be suspected with an offset greater than 3 mm in an adult (Figure 4).9
Conclusion
It is important to differentiate congenital mid-line clefts of the atlas from a Jefferson fracture. This can be done by close inspection of the plain radiographs, and confirmed by CT.
References
Von Torklus D, Gehle W . The upper cervical spine Grune & Stratton: New York 1972 25
Gehweiler J, Osbourne R, Becker R . The Radiology of Vertebral Trauma Saunders: Philadelphia 1980 p 55
Warwick R, Williams PL (eds). Gray's Anatomy 36th Ed Churchill Livingstone (Edinburgh) 1980 3: 283
Wackenheim A . Roentgen Diagnosis of the Craniovertebral Region Springer-Verlag: Berlin, Heidelberg, New York 1974 p 199
Geipel P . Zur Kenntnis der spanltbildungen des Atlas und Epistopheus. Teil IV Zentralbl Allg Pathol 1955 94: 19–84
Schulze P, Buurman R . Absence of the posterior arch of the atlas Am J Roent 1980 134: 178–180
Gehweiler J, Daffner R, Roberts L . Malformation of the atlas vertebra simulating the Jefferson fracture Am J Roent 1983 140: 1083–1086
Hadley M et al. Acute Traumatic Atlas Fractures: Management and Long-Term Outcome Neurosurgery 1988 23: 31–35
Chambers A, Gaskill M . Mid-line anterior atlas clefts: CT findings Journal of Computer Assisted Tomography 1992 16: 868–870
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Prempeh, R., Gibson, J. & Bhattacharya, J. Mid-line clefts of the atlas: a diagnostic dilemma. Spinal Cord 40, 92–93 (2002). https://doi.org/10.1038/sj.sc.3101230
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101230
Keywords
This article is cited by
-
Posttraumatischer Tortikollis beim Schulkind
Der Unfallchirurg (2010)
-
Partielle Aplasie des Atlasbogens beim Kind
Der Unfallchirurg (2009)
-
C1-2 vertebral anomalies in 22q11.2 microdeletion syndrome
Pediatric Radiology (2008)






