Abstract
Extrapyramidal side-effects (EPSE) of antipsychotic medication are related to the occupancy of dopamine D2 receptors and there appears to be a threshold of D2 occupancy below which clinically EPSE are unlikely to occur. It is unclear whether there are motor changes produced by ‘subthreshold’ levels of D2 occupancy that are not detectable by clinical examination. This study was designed to investigate whether a number of electromechanical instrumental techniques could detect ‘subthreshold’ motor changes and whether these changes correlate with dopamine D2 occupancy as measured by [11C]-raclopride PET scan. Twenty medication naïve patients were studied before and during treatment with low dose haloperidol. Instrumental techniques detected an asymmetrical worsening in motor function with drug treatment despite the failure of the group to experience significant EPSE. These changes did not correlate with D2 occupancy and measurements of rigidity, tremor, and bradykinesia did not closely inter-correlate.
Similar content being viewed by others
Main
Positron emission tomography (PET) has been used to investigate the relationship between occupancy of striatal dopamine D2 receptors and the occurrence of extrapyramidal side effects (EPSE) produced by antipsychotic medication. Several of these studies have suggested that EPSE are more likely to occur when occupancy of D2 receptors is greater than 75–80% (Nordstrom et al. 1993; Kapur et al. 1995; Farde et al. 1992). Studies in Parkinson's disease (PD) such as that published by Bernheimer et al. (1973) also have found that symptoms of PD only become apparent following the loss of 70–80% of dopamine in striatal nuclei. This appears to suggest that normal functioning of the motor system only requires 20–30% of the dopaminergic system to remain unaffected by disease or medication.
More recently evidence has emerged that finer functional impairment may emerge with significantly less loss of dopamine function. In a study of normal adults between the ages of 24 and 86 years, Volkow et al. (1998) found that an age-linked decline in brain dopamine D2 receptors was associated with a linear decline in a number of functional measures. This performance deterioration was seen with a motor task (Finger Tapping Test) as well as measures of frontal lobe function. This challenges the assumption that the brain is able to compensate for any decline in dopaminergic function of less than ∼80%. More recent data in Parkinson's disease also support this notion. Studies of the dopamine transporter (as a marker of striatal dopaminergic neurones) and uptake of radioactively labeled dopa indicate that patients with early PD may have lost only ∼50% of dopaminergic input into the putamen when they first manifest clinical symptoms (Guttman et al. 1997; Morrish et al. 1995).
The picture is further complicated by the measures used in these studies. All previous studies, with the exception of that by Volkow et al. (1998), used subjective rater measurements of EPSE or PD. Volkow et al. (1998) used the Finger Tapping Test, which while a test of motor function, is not a commonly used measure of EPSE. Futhermore, in most studies using clinical assessments, the symptoms of parkinsonism are clumped together and are not analysed or studied separately. It may be somewhat misleading to automatically group these measures of motor dysfunction. Studies in PD have found that the pathology underlying these clinical symptoms may not be uniform. Specifically, there is evidence that the emergence of rigidity and hypokinesia are correlated with the loss of lateral substantia nigra neurons with a subsequent reduction in dopamine in the putamen (Rinne et al. 1989; Rinne 1991). This relationship, however, is not seen with the emergence of tremor, which appears to result from broader neuronal degeneration (Bernheimer et al. 1973; Larochelle et al. 1971; Hassler 1984; Poirier et al. 1975). Similarly, relationships have been found between tyrosine hydroxylase activity, hypokinesia, and rigidity, and between cerebrospinal fluid levels of homovanillic acid and hypokinesia (Rinne 1978; Rinne and Sonninem 1972). Neither of these measures correlate with tremor in PD.
The recent development of a number of instrumental measures of extrapyramidal motor symptoms appears to offer several valuable tools for the investigation of these symptoms as independent entities. Caligiuri (1994) have demonstrated that it is possible to reliably and validly measure parkinsonian rigidity, bradykinesia (Caligiuri et al. 1998) and tremor (Caligiuri et al. 1991). These instrumental measures appear to be sensitive to mild symptoms and may prove to be capable of detecting subclinical levels of parkinsonian symptoms (Caligiuri et al. 1989).
This study had three goals: firstly, to investigate whether instrumental methods could be used to detect subclinical alterations in motor function (AMF) in subjects without overt clinical EPSE and at levels of D2 occupancy below 80%; secondly, to investigate whether subclinical AMF correlate with striatal D2 occupancy; and thirdly, to investigate whether instrumentally measured rigidity, hypokinesia and tremor appear consistently at low levels of D2 occupancy, whether the presence and severity of the individual symptoms will inter-correlate.
METHODS
Subjects
Twenty patients participated in the study. There were 16 males (mean age 29.5 ± 7.6 years) and four females (28.5 ± 7.2 years). Nineteen patients had a diagnosis of schizophrenia and one patient had a delusional disorder (DSM-IV). The diagnoses were established utilizing a structured interview with the patient using a SCID (First et al. 1995), supplemented with information from the family and clinical staff. Patients for the study were recruited within the Schizophrenia Division of the Clarke Institute of Psychiatry, Toronto, Ontario, Canada. Patients with a history of current alcohol or substance abuse were excluded. All patients were considered to be experiencing their first episode of a psychotic illness. Eighteen patients had never been previously treated with antipsychotic medication, one patient had several months of treatment within the last year but had been poorly compliant and had not taken medication for several months. Another patient had taken a few doses of an antipsychotic two weeks prior to entering the study.
All patients provided written informed consent in a format approved by the University of Toronto Review Committee on the Use of Human Subjects. All patients were taking part in a clinical trial of low dose haloperidol and received either 1 or 2.5 mg per day in a single dose, at night. Clinical data from this study will be reported separately. It was predicted that treatment with these doses of medication should result in a low incidence of clinical EPSE.
Haloperidol Plasma Assay
Plasma was obtained at the time of the scans and levels of haloperidol were measured using a Fison TRI0-1000 gas chromatograph-mass spectrometer (GC-MS). The sensitivity of the assay was such that 0.19 ng/ml of haloperidol was quantified with a coefficient of variation (CV) of 6.7%, whereas 1.88 ng/ml of haloperidol was quantified with a CV of 3.2%.
Imaging
All patients received a [11C]-raclopride PET scan between 12 and 13 hours after their last dose of haloperidol and all had been on a fixed dose of medication for at least 10 days (average 14.8 days). All PET scans were performed using 9.71 ± 0.48 mCi of high specific activity [11C]-raclopride [972 ± 419 Ci/mmol] and a GE-2048–15B head scanner. [11C]-raclopride was administered by bolus (59%) plus continuous infusion over 75 minutes. This has previously been described in detail (Houle et al. 1996; Kapur et al. 1996a, b). Striatal (caudate and putamen) and cerebellar regions of interest (ROI) were drawn on two contiguous PET slices. The cerebellar time-activity curve (TAC) was used as an estimate of the free and nonspecific [11C]-raclopride binding. The striatal TAC provided an estimate of non specific and free binding plus the specific binding to receptors. Under these assumptions, it can be shown that the striatal/cerebellar ratio minus one, at the time when the binding is at equilibrium (30–75 minutes in the scan) provides an index proportional to the Bmax/Kd of [11C]-raclopride for the dopamine D2 receptors (the binding potential, BP). We have previously demonstrated that this method is highly reliable (scan-rescan standard deviation of 6%) and correlates well with analytically derived estimates of D2 BP(r > 0.95) (Kapur et al. 1996a, b).
We did not have baseline measures of D2 BP for the patients in this study. Therefore, we used an aged-corrected estimate of D2 BP from a separate pool of 15 age-matched controls and 12 antipsychotic naïve patients with schizophrenia. The pooling of this groups was justified as there was no significant difference between the groups (F[1,24] = 0.36; p = .55) or a significant ‘age × illness’ interaction (F[1,24] = 0.58; p = .45). This is consistent with previous studies of D2 BP of patients with schizophrenia (Hietala et al. 1994; Farde et al. 1990). Haloperidol induced receptor occupancy was determined by the following:  where D2 BPBas is the age-corrected D2 BP baseline, and D2 BPHal is the D2 BP for patients on haloperidol.
where D2 BPBas is the age-corrected D2 BP baseline, and D2 BPHal is the D2 BP for patients on haloperidol.
Both estimates of ‘unoccupancy’, i.e., the observed binding potential, and occupancy were used for analysis in the study as it is not resolved whether the development of antipsychotic EPSE relates to the number of occupied receptors or to the actual number of free unaffected receptors available for functioning (Fitzgerald et al. 1999).
Instrumental Measures
All instrumental measures of extrapyramidal side effects (IEPS) were administered by a single investigator. All signals generated were low pass filtered (20Hz) and digitised (100 samples/sec) using a laboratory microcomputer. Kinematic variables such as amplitude and velocity were collected using waveform analysis software (Pegasus for Windows 1.2; Lakeshore Technologies, Inc., Chicago, IL). All measures were taken prior to the commencement of medication and again at the time of PET scanning. All measures were taken on both sides of the body.
Tremor
Hand tremor was measured with a hand force transducer. The subject was required to exert an isometric force (0.3 N) against a rigid beam with visual feedback provided by an oscilloscope displayed on a computer monitor. The measurement of tremor was estimated as the degree of error in the digitised force signal due to force fluctuation in the 3–7 Hz frequency range. The raw force wave forms were subjected to a bidirectional digital filter with a low pass cut-off of 3 Hz. The tremor index was derived from the force error difference between the unfiltered and filtered waveforms. For example, if the unfiltered force error was 5.0% and the filtered error was 4.0%, the tremor index would be 1.0%. That is, 1.0% of the steadiness error was due to tremor. It has previously been demonstrated that tremor elicited by sustained force is a sensitive method of detection of parkinsonian tremor in this frequency range (Caligiuri et al. 1991).
Rigidity
Muscle rigidity was measured with a device that transduces force and rotation simultaneously. These variables were measured during the passive movement of the wrist. The measurement was performed in a resting state and during activation of the non-test limb. A rigidity index was calculated as the degree of increase in stiffness produced by activation of the non-test limb. This methodology reduces variability due to muscle mass bulk, is sensitive to mild rigidity, and can be measured with good test-retest reliability (Caligiuri et al. 1991, 1989).
Bradykinesia
Two methods were used to measure bradykinesia. The mechanics of the first method have been described recently in some detail (Caligiuri et al. 1998). In this procedure, rapid alternating movements or RAMS, the subject was instructed to move his/her wrist rapidly back and forth while holding an electrogoniometer handle that measures wrist rotation. During this rapid alternating wrist flexion and extension both amplitude and frequency were measured. Movement speed was derived from a Fourier transformation and a model based upon previously obtained normal control data used to control for the extent of movement. This procedure generated a residual score that represents the difference between the measured movement speed and that predicted from the control data given the subject's amplitude of movement.
The second methodology (peak mean ballistic movement velocity) used the same apparatus as the first but was designed to measure the maximum velocity of movement that could be achieved by the subject. During this experiment the subject was told to make a short maximum velocity movement when cued by the investigator. Thirty trials were performed and the position/time curve recorded. The first derivative of this curve was taken to give a graphical representation of movement velocity and the mean of the highest five velocity peaks was calculated.
Data Analysis
Data were analysed from both sides of the body and the side with the greatest change between pre and post treatment separately. Within subject paired t-tests were used to examine for changes with treatment from baseline to the time of PET scan. A repeated measures general linear model was used to look for an effect of dose on these changes. Independent sample t-tests were used to look for differences within the group. Partial Pearson correlational analyses were conducted to examine the relationship between dopamine receptor occupancy, plasma haloperidol levels and IEPS scores at the time of PET scan, controlling for IEPS scores at baseline. Correlational analyses between scores of IEPS were performed after converting these measures to z-scores.
RESULTS
Dopamine D2 receptor occupancy in the 20 patients ranged from 38.1 to 86.7% (mean 66.1%). Eighteen of the twenty subjects had D2 occupancy levels less than 80%. There was no significant difference between occupancy values on the left (mean 65.4 ± 13.2%) and right (65.7 ± 13.3%) sides (t = −0.81, df = 19, p = .43). Occupancy values did not significantly vary with age or sex. Plasma haloperidol values ranged from 0.19 to 1.95 ng/ml (mean 0.86 ng/ml).
When examined at the time of PET scan, only two patients had clinical EPSE and one patient had been commenced on antiparkinsonian medication. These patients had occupancy values of 78.6%, 81.1%, and 79.4%. These three patients had higher mean IEPS scores on several measures than the patients without EPS but this did not reach significance on any measure.
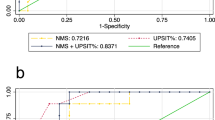
In regards to our first objective, scores on all four measurements were found to have worsened significantly with treatment when the more vulnerable side was analysed separately (see Table 1). For each patient, the more vulnerable side was consistent across IEPS measures. In eight patients, all four measures performed were worse on one side and in all other patients, three out of the four measures were performed most poorly on the same side. The distribution of the more vulnerable side for each IEPS measure is presented in Figure 1. There was no dose time interaction effect for any of the measures; the change was not more dramatic for patients treated with 2.5 mg rather than 1 mg per day.
In regards to the relationship between subclinical AMF and D2 occupancy, the results of the partial correlational analyses are presented in Table 2 . There were no significant correlations between IEPS scores and D2 occupancy or plasma haloperidol levels. There were no correlations with binding potential values.
Furthermore, there were no significant correlations between the measures of stiffness, tremor, and bradykinesia. The two methods of assessing bradykinesia did correlate significantly (r = 0.57, p = .008).The relationships between change on the more vulnerable side with treatment for the 4 measures of IEPS are presented in Table 3. There was no relationship between handedness and side vulnerability.
DISCUSSION
To our knowledge, this study is the first published report that explores the relationship between medication induced dopaminergic blockade and motor impairment as assessed by electromechanical means. There are a number of interesting findings. Firstly, it appears possible to detect motor changes in patients treated with antipsychotic drugs that have induced relatively low levels of D2 occupancy and no EPSE. Secondly, at low levels of D2 occupancy, motor changes appear to present asymmetrically. Thirdly, these motor changes do not appear to correlate with dopamine D2 receptor occupancy. Finally, instrumentally measured symptoms of tremor, rigidity, and bradykinesia do not correlate closely with one another at a low level of D2 occupancy.
As was suspected, the study has confirmed that there appear to be motor changes in patients who experience low levels of antipsychotic induced dopamine blockade. These changes present asymmetrically such that the differences were significant only on the more vulnerable side. For each patient, the more vulnerable side was consistent across measures of IEPS and the more vulnerable side was divided between the left (13 patients) and right (7 patients) sides in the patient group.
Asymmetrical presentation of motor symptoms is also frequently seen in early PD, unilateral symptoms often existing for months prior to the development of bilateral impairment. This appears to reflect asymmetry in the progression of basal ganglia pathology (Wenning et al. 1998; Rinne et al. 1995). It has been proposed that antipsychotic EPSE may demonstrate less asymmetry than that seen in PD (Tarsey 1989; Hausner 1986). However, this may be less true for acutely treated patients than chronically treated patients (Caligiuri et al. 1989). Given the findings of this study, it would appear that early motor changes in antipsychotic EPSE also appear to exhibit substantial asymmetry and the presentation of patients with bilateral symptoms mainly represents a higher degree of dopaminergic blockade.
Why should antipsychotic EPSE present asymmetrically at low levels of D2 occupancy? It is possible that this may relate to an asymmetrical distribution of antipsychotic medication in the brain (Tomer et al. 1987), although this appears unlikely given the equal values for right and left sided occupancy and binding potential seen in this study. It is possible that it may relate to laterality variations in dopaminergic hyperactivity such as the right sided dopaminergic hyperactivity proposed by Bracha (1987). For example, right sided dopaminergic hyperactivity would result in ipsilateral EPSE as the dose of antipsychotic medication required to return the right striatum to normal dopaminergic functioning would reduce left striatal dopaminergic function into the parkinsonian range. Several studies have also suggested the existence of an asymmetry of D2 receptor density in schizophrenia (Reynolds et al. 1987; Crawley et al. 1986), although these seems unlikely to be the explanation for the findings in our study given the equality of radiotracer binding.
It was surprising that the motor changes we found, in patients with low levels of D2 occupancy, did not correlate with D2 occupancy and this result is not consistent with a recently published study that found a correlation between D2 occupancy and a measure of reduction in hand writing (Kuenstler et al. 1999). Importantly, both studies detect the presence of subtle motor changes in patients with low D2 occupancy levels despite quite divergent methodologies. It is possible that the differences in correlations between the two studies is explained by several differences including the inclusion of several patients in the study of Kuenstler et al. (1999) with very high levels of D2 occupancy and differences in the patient group. Whilst almost all patients in our sample were neuroleptic naïve, all patients in the study of Kuenstler et al. (1999) had received prior antipsychotic therapy.
In our study, this lack of a correlation was consistent across all measures of IEPS and appears to be a robust finding. In this study, most patients had D2 occupancy levels insufficient to produce clinical EPSE. It is clear that in patients with a higher degree of D2 blockade, clinical EPSE do relate to D2 occupancy and the development of EPSE appears to be a threshold phenomena which exhibits itself only after a certain level of D2 occupancy is reached (Farde et al. 1992). It also seems likely that in patients treated with doses sufficient to induce higher levels of D2 blockade, that there may be a relationship between instrumentally measured motor changes and D2 occupancy, as at these occupancy levels the instrumental measures are likely to be measuring true clinical EPSE. The motor changes that were detectable in this study, however, do not appear to share the same relationship with D2 occupancy and it may be the case that these subclinical AMF have a different pathophysiological basis or that the effects are too small for a correlation to be apparent.
Another interesting finding is the lack of close relationships between the individual measurements of IEPS. As would be expected, there was a close relationship between the two measures of bradykinesia. Furthermore, the correlations between tremor, rigidity, and bradykinesia (0.37 and 0.27) were limited but indicated some relationship. This data appears to support the scarce literature concerned with pathophysiological differences between symptoms of parkinsonism. Specifically, this points to differences in the underlying pathophysiology of these symptoms, although rigidity and bradykinesia appear to share some similarities (Bernheimer et al. 1973; Larochelle et al. 1971; Hassler 1984; Poirier et al. 1975; Rinne 1978; Rinne and Sonninem 1972). It is possible that the differences between symptoms are more pronounced at low levels of dopaminergic disruption.
Several issues need to be considered in regards to our methodology. Firstly, the instrumental techniques used to measure motor functioning were developed for the measurement of clinical EPSE, not the subclinical motor changes we were looking for in the study. However, they have been applied in a variety of clinical populations, including neuroleptic naïve patients (Caligiuri et al. 1993), a reasonable equivalent population to that found here. Secondly, it is possible that the failure of the study to detect a significant relationship between subclinical AMF and dopamine occupancy was a type II error resulting from a small real effect at low occupancy levels, the relatively small sample size, and a high degree of variability in the IEPS measures. Nonetheless, this appears unlikely as there is no indication of a trend towards positive correlations across the measures. Finally, in the absence of a placebo control group it is not possible to unequivocally attribute the change in IEPS scores to drug treatment. However, any learning effect would be expected to improve, not worsen task performance, especially as the patients clinically improved over the time period. Additionally, a number of these measures have demonstrated quite reasonable degrees of test-retest reliability, specifically test-retest coefficients of 0.98 (Caligiuri et al. 1998), 0.87 (Caligiuri et al. 1989), and 0.73 (Caligiuri et al. 1991).
It has been suggested that there may be a threshold for the onset of the therapeutic and motor side effects of antipsychotic medication. Specifically, if patients can be treated with doses of medication that achieve less than ∼80% D2 occupancy, normal functioning of the motor system may be achieved in the majority. Thus, if therapeutic benefits are achieved at lower occupancy levels, there may be a therapeutic window free of major complications. The current study supports the notion that clinical EPSE are uncommon at low levels of D2 occupancy but does not support the notion that the motor system is unaffected at these levels. If these changes are not clinically apparent, what is the significance of this finding? Theoretically, it is an important additional piece of evidence in the growing body of work that indicates that motor changes appear with 50–60% loss of dopaminergic function rather than closer to 80%. In this, it is consistent with the findings of studies in normal aging (Volkow et al. 1998) and in patients with early PD (Guttman et al. 1997; Morrish et al. 1995).
These findings may also be clinically relevant. Despite the fact that these changes are not detectable during standard clinical examination, it does not imply that they do not have functional implications. Patients being treated in the community with these medications are likely to engage in a variety of tasks requiring a reasonable degree of motor performance such as driving a motor vehicle or operating machinery in an employment setting. It is unclear how this level of neuromotor dysfunction may affect those tasks. Additionally, the presence of subclinical motor changes may prove an important clue as to the future likelihood of patients developing tardive dyskinesia. There is evidence that the presence of EPSE is a risk factor for the future development of tardive dyskinesia (Chouinard et al. 1988) and it remains to be shown whether the ‘subclinical’ motor changes demonstrated here may also relate to the future development of tardive movement disorder.
These questions may become increasingly relevant with the development of an increasing diversity of atypical antipsychotic medications with wider range of D2 receptor occupancy. For example, clozapine which has placebo like levels of clinical EPSE, blocks up to 65% of D2 receptors (Farde et al. 1992; Kapur 1998). Olanzapine, while having a low incidence of EPSE, appears to block D2 receptors in the 60–80% range (Nyberg et al. 1998; Kapur et al. 1998). It remains to be established whether these medications induce subclinical EPSE and what the implications of this will be. It is unclear whether anticholinergic medication removes EPSE or, alternatively, suppresses it to a subclinical state.
Research has only recently begun to reevaluate the degree of dopaminergic neuronal dysfunction associated with the development of motor impairment. Evidence in both normal aging and PD indicates that changes may be seen with as little as 50–60% dopaminergic loss. This study indicates that relatively low levels of antipsychotic-induced dopamine receptor blockade result in subclinical alterations in motor functioning. These changes do not correlate with striatal dopamine D2 blockade. The study also indicates that the changes do not present uniformly at these low levels of dopamine D2 occupancy and that these symptoms will often present asymmetrically.
References
Bernheimer H, Birkmayer W, Hornykiewicz O, Jellinger K, Seitelberger F . (1973): Brain dopamine and the syndromes of Parkinson and Huntington. J Neurol Sci 20: 415–455
Bracha HS . (1987): Asymmetric rotational (circling) behavior, a dopamine-related asymmetry: Preliminary findings in unmedicated and never-medicated schizophrenic patients. Biol Psychiatry 22: 995–1003
Caligiuri MP . (1994): Portable device for quantifying parkinsonian rigidity. Mov Disord 9: 57–63
Caligiuri MP, Bracha S, Lohr JB . (1989): Asymmetry of neuroleptic-induced rigidity; development of quantitative methods and clinical correlates. Psychiatry Res 30: 275–284
Caligiuri MP, Lohr JB, Bracha S, Jeste DV . (1991): Clinical and instrumental assessment of neuroleptic-induced parkinsonism in patients with tardive dyskinesia. Biol Psychiatry 29: 139–148
Caligiuri MP, Lohr JB, Jeste DV . (1993): Parkinsonism in neuroleptic-naïve schizophrenic patients. Am J Psychiatry 150: 1343–1348
Caligiuri MR, Lohr JB, Ruck RK . (1998): Scaling of movement velocity: A measure of neuromotor retardaton in individuals with psychopathology. Psychophysiology 35: 431–437
Chouinard G, Annable L, Ross-Chouinard A, Mercier P . (1988): A 5-year prospective longitudinal study of tardive dyskinesia: Factors predicting appearance of new cases. J Clinical Psychopharmacol 8(suppl 4):21S–26S
Crawley JC, Owens DG, Crow TJ, Poulter M, Johnstone EC, Smith T, Oldland SR, Veall N, Owen F, Zanelli GD . (1986): Dopamine D2 receptors in schizophrenia studied in vivo [letter]. Lancet 2: 224–225
Farde L, Nordstrom A, Wiesel FA, Pauli S, Halldin C, Sedvall G . (1992): Positron emission tomographic analysis of central D1 and D2 dopamine receptor occupancy in patients treated with classical neuroleptics and clozapine: Relation to extrapyramidal side effects. Arch Gen Psychiatry 49: 538–544
Farde L, Wiesel FA, Stone-Elander S, Halldin C, Norstrom AL, Hall H, Sedvall G . (1990): Dopamine Receptors in Neuroleptic Naïve Schizophrenic Patients. Arch Gen Psychiatry 47: 213–219
First M, Spitzer R, Gibbon M, Williams J . (1995): Structured Clinical Interview for DSM-IV Axis I Disorders—Clinician Version. Washington, DC, American Psychiatric Press
Fitzgerald PB, Kapur S, Seeman P . (1999): Neuroreceptor studies in psychotic disorders in the elderly: Potential for understanding antipsychotic effects. In Howard R, Rabins P (eds), Late Life Onset Schizophrenia: An International Perspective. Petersfield, UK, Wrightson Biomedical Publishing, in press
Guttman M, Burkholder J, Kish SJ, Hussey D, Wilson A, DaSilva J, Houle S . (1997): [11C]RTI-32 PET studies of the dopmine transporter in early dopa-naive Parkinson's disease: Implications for the symptomatic threshold. Neurology 48: 1578–1583
Hassler RG . (1984): Role of the pallidul and its transmitters in the therapy of parkinsonian rigidity and akinesia. Adv Neurol 40: 1–14
Hausner RS . (1986): Neuroleptic-induced parkinsonism and Parkinson's disease. J Clin Psychiatry 44: 13–16
Hietala J, Syvalahti E, Vuorio K, Nagren K, Lehikoinen P, Ruotsalainen U, Rakkolainen V, Lehtinen V, Wegelius U . (1994): Striatal D2 dopamine receptor characteristics in neuroleptic naive-schizophrenic patients studied with positron emission tomography. Arch Gen Psychiatry 51: 116–123
Houle S, Kapur S, Hussey D, Jones C, DaSilva J, Wilson AA, Cunningham B, Bailey D, Jones T . (1996): Measurement of [11C]-raclopride binding using a bolus plus infusion protocol. In Myers R (ed), Quantification of brain function using PET. San Diego, CA, Academic Press, pp 262–265
Kapur S . (1998): A new framework for investigating antipsychotic action in humans: Lessons from PET imaging. Mol Psychiatry 3: 135–140
Kapur S, Remington G, Zipursky RB, Wilson AA, Houle S . (1995): The D2 dopamine receptor occupancy of risperidone and its relationship to extrapyramidal symptoms: A PET study. Life Sci 57: PL103–PL107
Kapur S, Remington G, Jones C, Wilson A, DaSilva J, Houle S, Zipursky R . (1996a): High levels of dopamine D2 receptor occupancy with low dose haloperidol treatment: A PET study. Am J Psychiatry 153: 948–950
Kapur S, Zipursky R, Jones C, Remington G, Wilson A, DaSilva J, Houle S . (1996b): The D2 receptor occupancy profile of loxapine determined using PET. Neuropsychopharmacology 15: 562–566
Kapur S, Zipursky R, Remington G, Jones C, DaSilva J, Wilson A, Houle S . (1998): The 5-HT2 and D2 receptor occupancy of Olazapine in schizophrenia: A PET investigation. Am J Psychiatry 155: 921–928
Kuenstler U, Juhnhold U, Knapp WH, Gertz H-J . (1999): Positive correlation between reduction in handwriting area and D2 dopamine receptor occupancy during treatment with neuroleptic drugs. Psychiatry Res 90: 31–39
Larochelle L, Bedard B, Poirer L, Sourkes T . (1971): Correlative neuroanatomical and neuropharmacological study of the temor and catatonia in the monkey. Neuropharmacology 10: 273–288
Morrish PK, Sawle GV, Brooks DJ . (1995): Clinical and [18F] dopa PET findings in early Parkinson's disease. J Neurol Neurosurg Psychiatry 64: 314–319
Nordstrom AL, Farde L, Wiesel FA, Forslund K, Pauli S, Halldin C, Uppfeldt G . (1993): Central D2-dopamine receptor occupancy in relation to antipsychotic drug effects—a double-blind PET study of schizophrenic patients. Biol Psychiatry 33: 227–235
Nyberg S, Nilsson U, Okubo Y, Halldin C, Farde L . (1998): Implications of brain imaging for the management of schizophrenia. Intl Clin Psychopharmacol 13(suppl 3):15S–20S
Poirier LJ, Pechadre JC, Larochelle L, Dankova J, Boucher R . (1975): Stereotaxic lesions and movement disorders in monkeys. In Meldrum BS, Marsden CD (eds), Advances in Neurology, volume 10. New York, New York, Raven Press, pp 5–22
Reynolds GP, Czudek C, Bzowej N, Seeman P . (1987): Dopamine receptor asymmetry in schizophrenia [letter]. Lancet 1: 979
Rinne JO . (1991): Niagral degeneration in Parkinson's disease in relation to clinical features. Acta Neurol Scand 84(suppl 136):87S–90S
Rinne JO, Laihinen A, Ruottinen H, Ruotsakainen U, Nagren K, Lehikoinen P, Oikonen V, Rinne UK . (1995): Increased density of dopamine D2 receptors in the putamen, but not in the caudate nucleus in early Parkinson's disease: A PET study with [11C]-raclopride. J Neurol Sci 132: 145–161
Rinne JO, Rummukainen J, Paljarvi L, Rinne UK . (1989): Dementia in Parkinson's disease is related to neuronal loss in the medial substantia nigra. Ann Neurol 26: 47–50
Rinne UK . (1978): Recent advances in research on parkinsonism. Acta Neurol Scand 67(suppl):S77–S112
Rinne UK, Sonninem V . (1972): Acid monamine metabolites in the cerebrospinal fluid of patients with Parkinson's disease. Neurology 22: 62–67
Tarsey . (1989): Neuroleptic-induced movement disorders. In Quinn NP, Jenner PG (eds), Disorders of Movement: Clinical, Pharmacological and Physiological Aspects. London, UK, Academic Press, pp 361–393
Tomer R, Mintz M, Kempler S, Sigal M . (1987): Lateralized neuroleptic-induced side effects are associated with asymmetric visual evoked potentials. Psychiatry Res 22: 311–318
Volkow ND, Gur RC, Wang GJ, Fowler JS, Moberg PJ, Ding YS, Hitzemann R, Smith G, Logan J . (1998): Association between decline in brain dopamine activity with age and cognitive and motor impairment in healthy individuals. Am J Psychiatry 155: 344–349
Wenning GK, Donnemiller E, Granata R, Riccabona G, Poewe W . (1998): 123I-B-CIT and 123I-IBZM-SPECT scanning in levodopa-naïve Parkinson's disease. Mov Disord 13: 438–445
Acknowledgements
The authors thank the patient volunteers, their families, and the clinical staff involved in their care, especially Dr. C.S. Shammi. We also thank Erin Toole, Doug Hussey, Kevin Cheung, Armando Garcia. and Jenny Lee for expert technical assistance; Kalyna Butler and Piri Babos for pharmacy services; Astra Arcus A.B. for providing the precursor for the synthesis of [11C]-raclopride and Dr. Alan Wilson for supervising the radiochemical syntheses. This work was supported by a grant from the National Alliance for Research in Schizophrenia and Depression. Dr. Kapur was supported by a Clinician Scientist award from the Medical Research Council of Canada.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Fitzgerald, P., Kapur, S., Caligiuri, M. et al. Instrumentally Detected Changes in Motor Functioning in Patients with Low Levels of Antipsychotic Dopamine D2 Blockade. Neuropsychopharmacol 22, 19–26 (2000). https://doi.org/10.1016/S0893-133X(99)00081-0
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(99)00081-0