Abstract
Local and systemic oxidative stress in intraocular pressure (IOP) elevation and optic nerve damage may be involved in the pathogenesis of glaucoma. We reported previously that a lower level of systemic antioxidative capacity is associated with IOP elevation in open-angle glaucoma (OAG). We assessed the correlation between the visual field sensitivity value, i.e., mean deviation (MD) and systemic levels of prooxidants and antioxidants by analyzing the blood biochemistry in 202 patients with glaucoma. Serum levels of lipid peroxides, ferric-reducing activity and thiol antioxidant activity were measured using the diacron reactive oxygen metabolite (dROM), biological antioxidant potential (BAP) and sulfhydryl (SH) tests, respectively, using a free-radical analyzer. Univariate and multivariate analyses suggested a positive correlation between MD and BAP (R = 0.005 and P = 0.0442 by a multiple regression model adjusted for seven demographic parameters), but no significant associations between the MD and the dROM (R = 0.002 and P = 0.8556) and SH tests (R = −0.001 and P = 0.8280). Use of more antiglaucoma medication and primary OAG rather than normal tension glaucoma also were associated significantly with worse visual field damage. This large and comprehensive assessment of the association between systemic redox status and visual field damage in OAG suggests that lower systemic antioxidant capacity measured by ferric-reducing activity is associated with more severe visual field damage in OAG that partly explained its roles in IOP elevation.
Similar content being viewed by others
Introduction
Glaucoma is a leading cause of irreversible blindness worldwide1 including in Japan2. The death of retinal ganglion cells (RGCs) and RGC axon loss causes glaucomatous optic neuropathy, in which elevated intraocular pressure (IOP) is the primary risk factor3. The IOP in patients with primary open-angle glaucoma (POAG) increases because of reduced aqueous humor outflow at the trabecular meshwork (TM)4. Treatment using hydrogen peroxide affects the cytoskeletal structure and cell-matrix interactions in TM cells5; depletion of glutathione and hydrogen peroxide treatment decrease the TM outflow facility6.
Oxidative stress results from formation of multiple reactive oxygen species including superoxide, hydrogen peroxide and hydroxyl radicals that can help in the formation and propagation of free radicals. The net oxidative burden between the prooxidant and antioxidant systems is oxidative stress, which damages cellular and tissue macromolecules, resulting in cellular and tissue dysfunction and death. Various oxidative stresses have been reported to induce RGC death in experimental studies7,8 and free-radical scavengers prevent glaucomatous tissue injury, specifically, glutamate- and IOP-induced RGC death9,10 and tumor necrosis factor α-induced axonal injury11. Evidence suggests that oxidative stress is involved in IOP elevations and RGC loss in POAG and POAG without marked IOP elevation such as that in normal tension glaucoma (NTG).
We reported significantly lower systemic antioxidant capacity levels in patients with OAG including POAG and glaucoma secondary to exfoliation syndrome (EX) compared with controls12. Although some studies found a correlation between glaucoma severity (i.e., IOP or visual field damage) and ocular13,14 or systemic15,16 levels of oxidative stress in humans, the role of systemic oxidative stress in the pathogenesis of glaucoma is largely unknown. We investigated a possible correlation between visual field damage and systemic levels of prooxidants and antioxidants in OAG (i.e., POAG and NTG).
Results
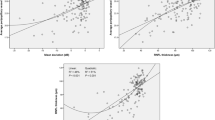
We measured the serum levels of systemic oxidative stress markers, i.e., lipid peroxides, ferric-reducing activity and thiol antioxidant activity using the diacron reactive oxygen metabolite (dROM), biological antioxidant potential (BAP) and sulfhydryl (SH) tests using a free-radical analyzer. Visual field damage was estimated as the mean deviation (MD) value of static perimetry as described in the Methods section. The subject demographic data and MD and oxidative stress marker values in 202 subjects with OAG are shown in Table 1. In this dataset, the average MD, dROM, BAP and SH test values were −10.5 ± 10.1 decibels, 354.6 ± 62.8 U.Carr, 1,955.8 ± 276.7 μmol/L and 612.9 ± 98.1 μmol/L, respectively.
By univariate analyses (Table 2), a lower BAP value was associated significantly (r = 0.1550 and P = 0.0276) with worse MD, while the dROM (r = −0.0121 and P = 0.8644) and SH test (r = −0.0380 and P = 0.5918) results were not associated with MD. Other than the BAP, other parameters possibly associated with worse MD were use of a higher number of glaucoma medications (P < 0.0001), an IOP higher than that previously recorded (P = 0.0005) and higher diastolic blood pressure (DBP) (P = 0.0068) among the continuous parameters (Table 2) and among the categorical parameters male gender (P = 0.0018), POAG rather than NTG (P = 0.0001) and current smoking (P = 0.0198) (Table 3).
To adjust for the possible confounding effects by other parameters, the association between MD and systemic oxidative stress markers were analyzed by multiple regression analysis. Seven parameters that showed a significant association with the MD by the univariate analyses were substituted into the multiple regression model together with one of the oxidative stress markers in each model (Table 4). The positive correlation between the MD and BAP remained significant (R = 0.005 and P = 0.0442) after adjustment for seven demographic parameters. Multivariate analyses did not find an association between the MD and dROM (R = 0.002 and P = 0.8556) or the SH test (R = −0.001 and P = 0.8280) (Table 4).
Discussion
The current study, which included 202 subjects with OAG, is the largest such study to assess the systemic redox status in glaucoma15,17,18,19,20,21,22,23,24,25,26,27,28,29. Yagci et al. reported increased protein carbonylation, a measure of protein oxidation, in aqueous and serum samples from patients with EX compared with controls19. Koliakos et al. identified significantly lower levels of antioxidative stress enzyme catalase activities in aqueous and serum samples from patients with EX compared with controls20. Nucci et al. also reported significantly lower total antioxidant capacity in aqueous humor and blood samples from patients with POAG compared with controls26. These studies indicated that the systemic antioxidant capacity reflects the local ocular redox status.
A few studies have evaluated the association between systemic oxidative stress and visual field damage. A significant correlation was found between a higher aqueous humor 8-hydroxy-2′-deoxyguanosine (8-OHdG) level, a marker of oxidative stress-induced DNA damage and a higher 8-OHdG level and lower antioxidant capacity levels in serum samples from patients with glaucoma (n = 28) but not between local/systemic 8-OHdG levels and the visual field MD15. A significant association was reported between the systemic vitamin E level and the clinical glaucoma parameters (n = 160), that is, IOP, optic nerve head alterations and visual field sensitivity; however, the study included mixed types of glaucoma in a case group23. The various types of glaucoma, i.e., open-angle and angle-closure glaucomas or primary and secondary glaucomas, have different etiologies; thus, separate analyses of each glaucoma type seemed more appropriate. Current study is the largest and the most comprehensive assessment of the association between systemic redox status and visual field damage in POAG and the significant association identified between the MD and BAP in the current study was unique. The difference in the sample number may explain the discrepancy between the previous and current studies.
A few groups have investigated the effects of local or systemic oxidative stress on glaucoma parameters. Increased 8-OHdG levels in TM specimens from humans were associated with higher IOP30 and more severe visual field loss13,14 in OAG and increased aqueous humor oxidative stress was associated with higher IOP in patients with EX31. We found previously that the systemic BAP level was lower in patients with higher IOP levels. The odd ratios suggested that, compared with subjects with the highest BAP value, subjects with the lowest BAP value have, respectively, 17 and 25 times higher chances of being classified into the IOP groups with the second highest and highest values16. The current study showed that, other than the BAP, use of more glaucoma medications and the presence of POAG rather than NTG were associated consistently with more severe visual field damage (Table 4). Considering these findings, in addition to the direct insults by oxidative stress on the RGCs, decreased systemic antioxidant capacity may be associated with neuronal damage through elevated IOP.
We did not identify a significant association between the dROM level and MD; this agreed with our previous observation of no significant association between the dROM and IOP levels16. Glaucomatous damage in the TM or neuronal cells may result from local increases in oxidative stress due to local compensation for systemic oxidative stress by systemic reduction of antioxidant capacity in each individual. The current study also found no significant association between the SH and MD. The glutathione and thioredoxin systems may be major thiol-mediated redox systems in humans, although the plasma glutathione level is 100 to 1,000 times higher than that of thioredoxin32,33. A negative correlation was found between age and total glutathione levels in red blood cells with no significant difference in the total glutathione level between patients with glaucoma and controls18. Thus, the current SH level may correspond mainly to the total glutathione level; however, that requires clarification. Previous studies have reported that thioredoxin system dysregulation may be a factor in the pathogenesis of glaucoma9,10,34,35,36. The thioredoxin level should be measured separately from other thiol groups.
The results of the current comprehensive large-scale study suggested that lower systemic antioxidant capacity measured by ferric-reducing activity is associated with more severe visual field damage in OAG, which is partly explained by its roles in IOP elevation.
Methods
Subjects
The study adhered to the tenets of the Declaration of Helsinki. The institutional review boards of Shimane University Hospital and Iinan Hospital, Shimane, Japan, reviewed and approved the research. All subjects provided written informed consent. In the current study, 202 Japanese subjects with OAG (POAG or NTG) were chosen from a previously established dataset of 531 subjects12,16. Briefly, OAG was diagnosed based on open iridocorneal angles bilaterally, the characteristic appearance of glaucomatous optic neuropathy such as enlargement of the optic disc cup or focal thinning of the neuroretinal rim, corresponding visual field defects identified using the Humphrey Visual Field Analyzer Swedish Interactive Thresholding Algorithm central 30-2 program (Carl Zeiss Meditec, Dublin, CA) in at least one eye and no evidence of secondary glaucoma bilaterally. Subjects with the history of untreated IOP of 21 mmHg or higher in at least one eye were considered to have POAG and other subjects with no history of untreated IOP of 21 mmHg or higher were considered to have NTG.
Recording clinical parameters and collecting blood samples
To avoid the possible confounding effect of systemic diseases37,38,39, we questioned subjects about a history of severe systemic diseases during an interview before study entry as previously described12,16. In addition to a history of severe systemic diseases, to adjust for the possible confounding effects of other factors such as differences in nutrition, blood pressure, blood glucose and smoking habits40,41,42, we recorded the presence or absence of diabetes, current smoking, time since the last meal and systolic and diastolic blood pressures (SBP and DBP, respectively) and pulse rate before blood samples were collected as well as the IOP measured and the number of glaucoma medications on the day of sample collection, the highest known IOP previously recorded in the medical charts and visual field MD values. Venous blood specimens were collected from the antecubital vein into evacuated tubes. During all handling procedures, including transportation from the clinical setting to the laboratory and centrifugation, the temperature was maintained at 4 °C. Serum samples obtained by centrifugation of the collected venous blood were stored at 4 °C until oxidative stress measurements.
Oxidative stress measurements
All blood analyses were performed using a free-radical analyzer system (FREE Carpe Diem, Wismerll Company Ltd., Tokyo, Japan). Based on the manufacturer’s recommendation, all analyses were performed within 48 hours of venous blood collection to avoid falsely high or low results. To analyze the serum levels of reactive oxygen metabolites, antioxidant capacity and thiol-antioxidant capacity, the dROM, BAP and SH tests were performed, respectively. The results of dROM testing were expressed in arbitrary units (U.Carr), one unit of which corresponds to 0.8 mg/L of hydrogen peroxide40,43; the results of the BAP test were expressed in μmol/L of the reduced ferric ions; the results of the SH test were expressed as μmol/L of the SH groups. A comparison of the measured levels of oxidative stress between the non-glaucoma and glaucoma groups was reported previously12.
Statistical analysis
The data are expressed as the means ± standard deviations and analyzed using JMP statistical software version 11.00 (SAS Institute, Inc., Cary, NC). In the analyses of the subjects with bilateral glaucoma, the eye with the worse (lower) MD between both eyes was the study eye. A possible association with the MD was analyzed using the Spearman’s rank correlation test for continuous data (i.e., age; number of glaucoma medications; highest IOP recorded; IOP on the day of sample collection; SBP; DBP; pulse rate; time since the last meal and dROM, BAP and SH tests) and the unpaired t-test for categorical data (i.e., sex, glaucoma type, diabetes and current smoking status). The associations between the MD and oxidative stress parameters also were analyzed by multiple regression analyses; the parameters associated with the MD by univariate analyses (i.e., Spearman’s rank correlation test or unpaired t-test) were substituted into the multiple regression models together with the oxidative stress parameters. P < 0.05 was considered statistically significant.
Additional Information
How to cite this article: Tanito, M. et al. Association between systemic oxidative stress and visual field damage in open-angle glaucoma. Sci. Rep. 6, 25792; doi: 10.1038/srep25792 (2016).
References
Foster, A. & Resnikoff, S. The impact of Vision 2020 on global blindness. Eye. 19, 1133–1135 (2005).
Iwase, A. et al. Prevalence and causes of low vision and blindness in a Japanese adult population: the Tajimi Study. Ophthalmology. 113, 1354–1362 (2006).
Weinreb, R. N. & Khaw, P. T. Primary open-angle glaucoma. Lancet. 363, 1711–1720 (2004).
Alvarado, J. A. & Murphy, C. G. Outflow obstruction in pigmentary and primary open angle glaucoma. Arch Ophthalmol. 110, 1769–1778 (1992).
Zhou, L., Li, Y. & Yue, B. Y. Oxidative stress affects cytoskeletal structure and cell-matrix interactions in cells from an ocular tissue: the trabecular meshwork. J Cell Physiol. 180, 182–189 (1999).
Kahn, M. G., Giblin, F. J. & Epstein, D. L. Glutathione in calf trabecular meshwork and its relation to aqueous humor outflow facility. Invest Ophthalmol Vis Sci. 24, 1283–1287 (1983).
Himori, N. et al. Critical role of Nrf2 in oxidative stress-induced retinal ganglion cell death. J Neurochem. 127, 669–680 (2013).
Yokoyama, Y. et al. The role of calpain in an in vivo model of oxidative stress-induced retinal ganglion cell damage. Biochem Biophys Res Commun. 451, 510–515 (2014).
Inomata, Y. et al. Thioredoxin inhibits NMDA-induced neurotoxicity in the rat retina. J Neurochem. 98, 372–385 (2006).
Munemasa, Y., Ahn, J. H., Kwong, J. M., Caprioli, J. & Piri, N. Redox proteins thioredoxin 1 and thioredoxin 2 support retinal ganglion cell survival in experimental glaucoma. Gene Ther. 16, 17–25 (2009).
Kitaoka, Y. et al. Axonal protection by 17beta-estradiol through thioredoxin-1 in tumor necrosis factor-induced optic neuropathy. Endocrinology. 152, 2775–2785 (2011).
Tanito, M., Kaidzu, S., Takai, Y. & Ohira, A. Status of systemic oxidative stresses in patients with primary open-angle glaucoma and pseudoexfoliation syndrome. PLoS One. 7, e49680 (2012).
Izzotti, A., Sacca, S. C., Cartiglia, C. & De Flora, S. Oxidative deoxyribonucleic acid damage in the eyes of glaucoma patients. Am J Med. 114, 638–646 (2003).
Sacca, S. C., Pascotto, A., Camicione, P., Capris, P. & Izzotti, A. Oxidative DNA damage in the human trabecular meshwork: clinical correlation in patients with primary open-angle glaucoma. Arch Ophthalmol. 123, 458–463 (2005).
Sorkhabi, R., Ghorbanihaghjo, A., Javadzadeh, A., Rashtchizadeh, N. & Moharrery, M. Oxidative DNA damage and total antioxidant status in glaucoma patients. Mol Vis. 17, 41–46 (2011).
Tanito, M., Kaidzu, S., Takai, Y. & Ohira, A. Correlation between systemic oxidative stress and intraocular pressure level. PLoS One. 10, e0133582 (2015).
Yildirim, O. et al. Role of oxidative stress enzymes in open-angle glaucoma. Eye. 19, 580–583 (2005).
Gherghel, D., Griffiths, H. R., Hilton, E. J., Cunliffe, I. A. & Hosking, S. L. Systemic reduction in glutathione levels occurs in patients with primary open-angle glaucoma. Invest Ophthalmol Vis Sci. 46, 877–883 (2005).
Yagci, R., Ersoz, I., Erdurmus, M., Gurel, A. & Duman, S. Protein carbonyl levels in the aqueous humour and serum of patients with pseudoexfoliation syndrome. Eye. 22, 128–131 (2008).
Koliakos, G. G., Befani, C. D., Mikropoulos, D., Ziakas, N. G. & Konstas, A. G. Prooxidant-antioxidant balance, peroxide and catalase activity in the aqueous humour and serum of patients with exfoliation syndrome or exfoliative glaucoma. Graefes Arch Clin Exp Ophthalmol. 246, 1477–1483 (2008).
Cumurcu, T. et al. Increased oxidative stress in patients with pseudoexfoliation syndrome. Ophthalmic Res. 43, 169–172, doi: 10.1159/000272019 (2010).
Yuki, K., Murat, D., Kimura, I. & Tsubota, K. Increased serum total antioxidant status and decreased urinary 8-hydroxy-2′-deoxyguanosine levels in patients with normal-tension glaucoma. Acta Ophthalmol. 88, e259–264 (2010).
Engin, K. N., Yemisci, B., Yigit, U., Agachan, A. & Coskun, C. Variability of serum oxidative stress biomarkers relative to biochemical data and clinical parameters of glaucoma patients. Mol Vis. 16, 1260–1271 (2010).
Majsterek, I. et al. Evaluation of oxidative stress markers in pathogenesis of primary open-angle glaucoma. Exp Mol Pathol 90, 231–237 (2011).
Erdurmus, M. et al. Antioxidant status and oxidative stress in primary open angle glaucoma and pseudoexfoliative glaucoma. Curr Eye Res. 36, 713–718 (2011).
Nucci, C. et al. Increased malondialdehyde concentration and reduced total antioxidant capacity in aqueous humor and blood samples from patients with glaucoma. Mol Vis. 19, 1841–1846 (2013).
Yuki, K. & Tsubota, K. Increased urinary 8-hydroxy-2′-deoxyguanosine (8-OHdG)/creatinine level is associated with the progression of normal-tension glaucoma. Curr Eye Res. 38, 983–988 (2013).
Demirdogen, B. C., Ceylan, O. M., Isikoglu, S., Mumcuoglu, T. & Erel, O. Evaluation of oxidative stress and paraoxonase phenotypes in pseudoexfoliation syndrome and pseudoexfoliation glaucoma. Clin Lab. 60, 79–86 (2014).
Lopez-Riquelme, N. et al. Endothelin-1 levels and biomarkers of oxidative stress in glaucoma patients. Intl Ophthalmol. 35, 527–532 (2014).
Izzotti, A., Longobardi, M., Cartiglia, C. & Sacca, S. C. Mitochondrial damage in the trabecular meshwork occurs only in primary open-angle glaucoma and in pseudoexfoliative glaucoma. PLoS One. 6, e14567 (2011).
Beyazyildiz, E. et al. Disturbed oxidant/antioxidant balance in aqueous humour of patients with exfoliation syndrome. Jpn J Ophthalmol. 58, 353–358 (2014).
Nakamura, H. et al. Chronic elevation of plasma thioredoxin: inhibition of chemotaxis and curtailment of life expectancy in AIDS. Proc Natl Acad Sci. 98, 2688–2693 (2001).
Michelet, F. et al. Blood and plasma glutathione measured in healthy subjects by HPLC: relation to sex, aging, biological variables and life habits. Clin Chem 41, 1509–1517 (1995).
Lamoke, F. et al. Loss of thioredoxin function in retinas of mice overexpressing amyloid beta. Free Radic Biol Med. 53, 577–588 (2012).
Fatma, N. et al. PRDX6 attenuates oxidative stress- and TGFbeta-induced abnormalities of human trabecular meshwork cells. Free Radic Res. 43, 783–795 (2009).
Miyamoto, N. et al. Quercetin induces the expression of peroxiredoxins 3 and 5 via the Nrf2/NRF1 transcription pathway. Invest Ophthalmol Vis Sci. 52, 1055–1063 (2011).
Vassalle, C., Pratali, L., Boni, C., Mercuri, A. & Ndreu, R. An oxidative stress score as a combined measure of the pro-oxidant and anti-oxidant counterparts in patients with coronary artery disease. Clin Biochem. 41, 1162–1167 (2008).
Nakayama, K. et al. Reduction of serum antioxidative capacity during hemodialysis. Clin Exp Nephrol. 11, 218–224 (2007).
Shimano, M. et al. Reactive oxidative metabolites are associated with atrial conduction disturbance in patients with atrial fibrillation. Heart Rhythm. 6, 935–940 (2009).
Cornelli, U., Terranova, R., Luca, S., Cornelli, M. & Alberti, A. Bioavailability and antioxidant activity of some food supplements in men and women using the D-Roms test as a marker of oxidative stress. J Nutr. 131, 3208–3211 (2001).
Martinovic, J. et al. Long-term effects of oxidative stress in volleyball players. Int J Sports Med. 30, 851–856 (2009).
Kotani, K., Koibuchi, H., Miyamoto, M., Yamada, T. & Taniguchi, N. Relationship between reactive oxygen metabolites and carotid intima-media thickness in subjects with hypercholesterolemia. Med Princ Pract. 19, 496–498 (2010).
Carratelli, M. et al. Reactive oxygen metabolites and prooxidant status in children with Down’s syndrome. Int J Clin Pharmacol Res. 21, 79–84 (2001).
Acknowledgements
This work was supported partly by a Grant-in-Aid for Scientific Research C from The Ministry of Education, Culture, Sports, Science and Technology (MEXT) (M.T.). The authors are grateful to Ms. Ryoko Takahashi for her technical help with the dROM, BAP and SH measurements.
Author information
Authors and Affiliations
Contributions
M.T., S.K., Y.T. and A.O. conceived and designed the experiments. M.K., S.K. and Y.T. collected the samples and performed the experiments. M.T. analyzed the data. M.T., S.K., Y.T. and A.O. wrote and reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Tanito, M., Kaidzu, S., Takai, Y. et al. Association between systemic oxidative stress and visual field damage in open-angle glaucoma. Sci Rep 6, 25792 (2016). https://doi.org/10.1038/srep25792
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep25792
This article is cited by
-
Comprehensive measurements of hydroxylinoleate and hydroxyarachidonate isomers in blood samples from primary open-angle glaucoma patients and controls
Scientific Reports (2019)
-
Is primary open-angle glaucoma an ocular manifestation of systemic disease?
Graefe's Archive for Clinical and Experimental Ophthalmology (2019)
-
Glaucoma is associated with plasmin proteolytic activation mediated through oxidative inactivation of neuroserpin
Scientific Reports (2017)
-
Age- and sex-dependency of the association between systemic antioxidant potential and glaucomatous damage
Scientific Reports (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.